When it comes to responding effectively in critical situations, knowing the correct procedures can make the difference between life and death. It’s essential to familiarize oneself with key protocols that can be used to assist someone in need until professional help arrives. In this section, we will explore the fundamental practices that are necessary to manage emergencies, focusing on immediate actions that anyone can take.
These practices involve recognizing symptoms, applying vital interventions, and understanding the tools available to enhance the chances of survival. Whether it’s a medical emergency or a sudden accident, knowing how to act quickly and correctly is crucial. This guide will provide clear explanations of what should be done in such scenarios, helping individuals prepare for the unexpected.
Mastering these techniques is not just about following steps; it’s about having the confidence and knowledge to make quick decisions under pressure. By reviewing the principles outlined here, you’ll be better equipped to respond in life-threatening situations with composure and effectiveness.
Overview of Emergency Response Assessment A
This assessment focuses on evaluating an individual’s ability to perform critical actions in emergency situations. It tests knowledge of life-saving interventions, proper techniques, and the correct sequence of steps to take when facing medical crises. Mastery of these skills is essential for anyone looking to assist others during urgent health events, and it ensures that responders are ready to act swiftly and effectively under pressure.
Purpose and Scope of the Assessment
The purpose of this evaluation is to verify a person’s competency in handling emergencies, such as cardiac arrest or choking. The content of the assessment covers a range of scenarios where prompt action can prevent further harm or even save lives. It examines theoretical knowledge alongside practical ability, ensuring individuals understand both the ‘why’ and the ‘how’ of key interventions.
Key Areas Tested in the Evaluation
Among the core areas tested are the techniques for airway management, chest compressions, and the correct use of emergency equipment. Participants are expected to demonstrate how to recognize critical conditions and respond with appropriate measures, including the use of automated external defibrillators (AEDs) and administering rescue breaths. The evaluation ensures responders are prepared for various real-world situations, empowering them to make decisions with confidence.
Understanding Key Concepts in Emergency Response
In any emergency situation, it is crucial to have a clear understanding of the fundamental concepts that guide effective intervention. The ability to recognize life-threatening conditions and apply the correct measures can significantly impact the outcome. This section delves into the essential principles of immediate care, covering the core techniques and their importance in maintaining a victim’s survival until professional help arrives.
Essential Techniques for Managing Critical Conditions
One of the foundational elements of responding to emergencies is knowing how to assess and address vital functions, such as breathing and circulation. Chest compressions are a key component in restoring blood flow during cardiac arrest, while airway management ensures that the victim can breathe effectively. In many cases, these steps are performed simultaneously to maximize the chances of survival.
The Importance of Timely Intervention
Intervening early can make the difference between life and death. Rapid response is essential, as delays can lead to further complications. Whether using a defibrillator or performing rescue breathing, acting quickly increases the likelihood of a positive outcome. Understanding the timeline of necessary actions and the tools required to assist in these interventions is crucial for anyone involved in emergency care.
Steps in Performing CPR Effectively
When faced with a person experiencing cardiac arrest, knowing the correct procedure for resuscitation is essential to increase the chances of survival. Cardiopulmonary resuscitation (CPR) is a series of deliberate actions that help restore blood circulation and oxygen to vital organs, particularly the brain and heart. This section outlines the critical steps involved in performing CPR effectively, ensuring that each action is carried out with precision and confidence.
Assessing the Situation and Victim
Before starting CPR, it is important to assess the situation quickly. Ensure that the environment is safe for both you and the victim. Check for responsiveness by gently tapping the person and calling out. If the individual is unresponsive and not breathing, immediately proceed to initiate CPR. Time is critical, and swift action can prevent brain damage and other serious complications.
Administering Chest Compressions and Rescue Breathing
The first step in CPR is performing chest compressions to restore blood circulation. Place the heels of your hands on the center of the chest, just below the sternum. Press down hard and fast, aiming for at least two inches deep and a rate of 100-120 compressions per minute. After 30 compressions, give two rescue breaths, ensuring the chest rises with each breath. If you are untrained or unable to provide breaths, continue compressions until help arrives. Chest compressions alone can be life-saving if performed properly.
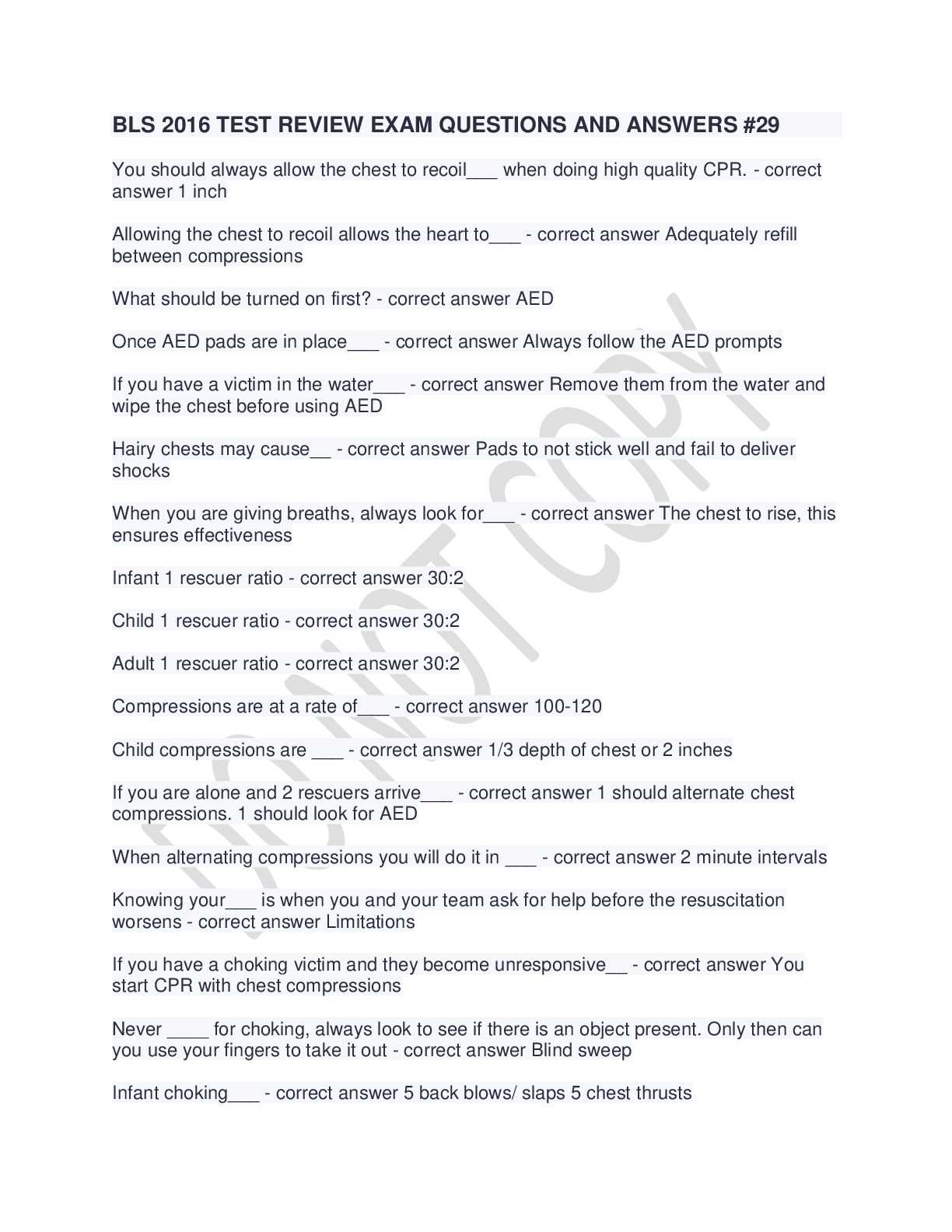
Common Questions in BLS Exam A
When preparing for a certification test in emergency care, there are certain questions that often appear, focusing on key concepts and techniques. These questions are designed to assess an individual’s understanding of life-saving practices and their ability to apply them in real-world situations. In this section, we will highlight some of the most common queries that test knowledge in critical care procedures and interventions.
Frequently Asked Questions
- What is the correct sequence of steps for performing CPR?
- How do you assess if a person is breathing or unresponsive?
- What is the recommended depth for chest compressions in adults?
- When should an Automated External Defibrillator (AED) be used?
- How should you perform rescue breathing for an adult victim?
Scenario-Based Questions
In addition to theoretical knowledge, scenario-based questions test how well individuals can apply what they’ve learned in specific emergency situations. These questions typically involve:
- Determining the first steps in an unconscious, non-breathing victim.
- Making decisions about whether to perform chest compressions or administer other interventions.
- Identifying signs of choking and the appropriate action to take.
Answering these questions requires a combination of knowledge, quick thinking, and an understanding of emergency procedures to ensure a positive outcome in critical situations.
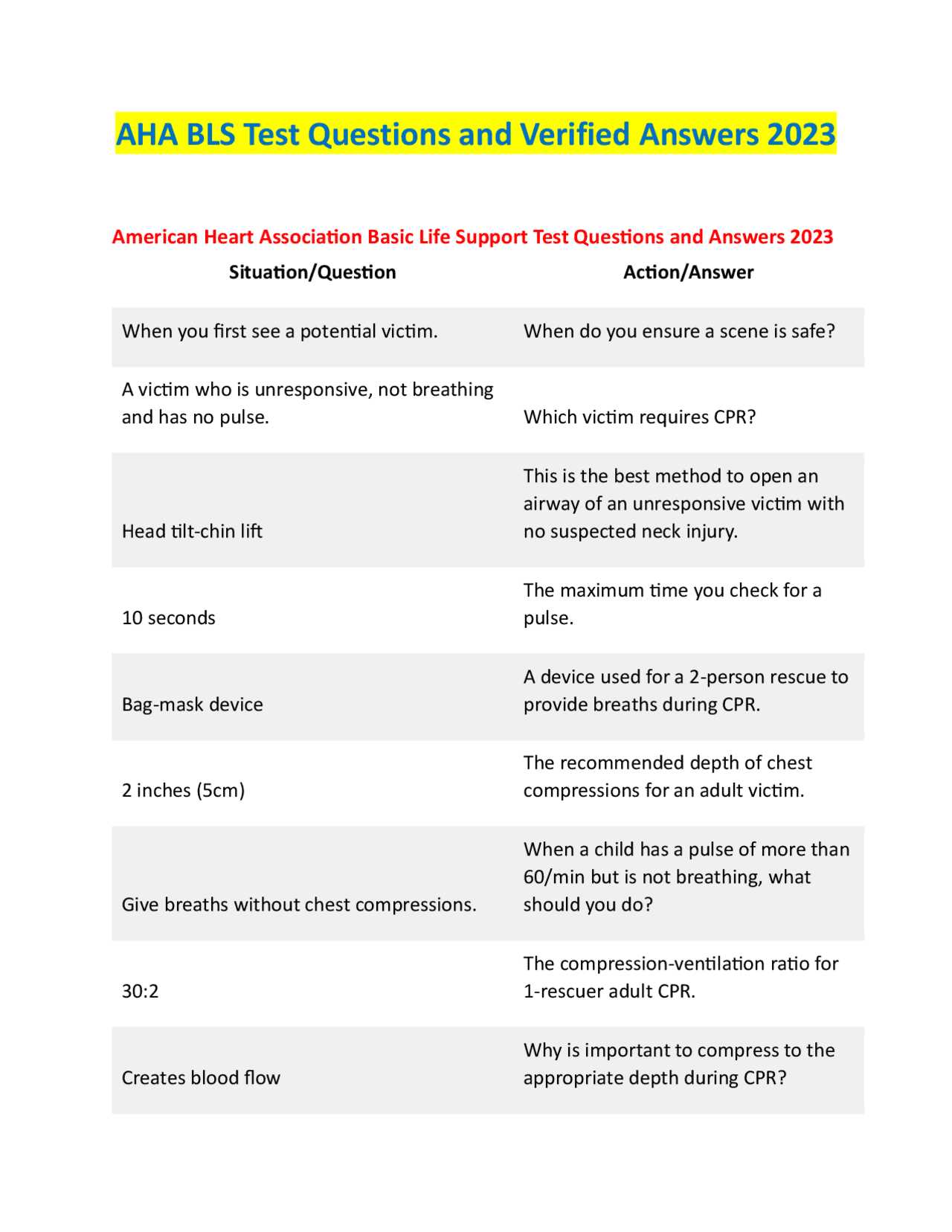
How to Assess Airway and Breathing
One of the first priorities when responding to an unconscious individual is to evaluate their ability to breathe and whether their airway is clear. Ensuring that the airway is open is essential for oxygen to reach the lungs and circulate through the body. In this section, we will explore the steps to properly assess these vital functions, which are crucial for determining the next course of action in an emergency situation.
Step-by-Step Guide to Airway and Breathing Assessment
The process involves checking both the victim’s airway and breathing. Here is a structured approach to follow:
| Step | Description |
|---|---|
| 1. Check Responsiveness | Gently tap or shake the victim to check if they respond. If unresponsive, proceed to the next step. |
| 2. Open the Airway | Place the victim on their back and tilt the head backward to open the airway, ensuring the tongue doesn’t block it. |
| 3. Check for Breathing | Look for chest rise, listen for breath sounds, and feel for airflow by placing your cheek near the victim’s mouth and nose. |
| 4. Determine Intervention | If the victim is not breathing or is breathing abnormally, begin rescue breathing or chest compressions as needed. |
Signs of Obstruction and Difficulty in Breathing
If the victim shows signs of choking or difficulty breathing, immediate action is necessary to clear the airway. Signs include:
- Inability to speak or cough
- Labored or noisy breathing
- Complete absence of breath
In these cases, further intervention, such as performing the Heimlich maneuver or using a suction device if available, may be required. Knowing how to act in such situations can save lives.
The Role of Chest Compressions
Chest compressions are a critical intervention when someone experiences cardiac arrest. By manually compressing the chest, the heart can be artificially stimulated to pump blood, supplying oxygen to vital organs like the brain. In emergencies, these compressions serve as the primary method of maintaining circulation until professional medical help can take over or further life-saving measures are implemented.
Why Chest Compressions Matter
Effective chest compressions help preserve brain function by ensuring that oxygenated blood continues to circulate throughout the body. The primary benefits include:
- Restoring Blood Flow: Chest compressions simulate the pumping action of the heart, ensuring blood reaches vital organs.
- Increasing Survival Rates: Early and continuous chest compressions can significantly improve the chances of survival in cardiac arrest victims.
- Buy Time: They help buy valuable time until an Automated External Defibrillator (AED) or advanced medical help is available.
Proper Technique for Chest Compressions
To perform chest compressions effectively, certain guidelines must be followed:
- Hand Placement: Place the heel of one hand on the center of the chest, just below the sternum. Place your other hand on top, interlocking the fingers.
- Compression Depth: Push down hard and fast, at least 2 inches deep for adults, allowing the chest to fully recoil between compressions.
- Compression Rate: Aim for a compression rate of 100 to 120 compressions per minute, similar to the tempo of the song “Stayin’ Alive” by the Bee Gees.
- Continuous Action: Do not pause for more than a few seconds between compressions to maintain circulation.
When performed correctly, chest compressions are a vital part of saving lives during emergencies. They increase blood flow and give the heart a better chance of restarting, while also improving the likelihood of recovery and minimizing damage to the brain and other organs.
Recognizing Cardiac Arrest Symptoms
Understanding the signs of cardiac arrest is crucial in emergency situations, as quick recognition can make the difference between life and death. This condition occurs when the heart stops beating effectively, leading to a lack of blood flow to vital organs. Being able to identify the symptoms early allows responders to act swiftly, providing the necessary interventions to restore circulation and improve survival chances.
Common Symptoms of Cardiac Arrest
While cardiac arrest can happen suddenly, there are certain key indicators to watch for. These include:
- Unresponsiveness: The person may collapse or be completely unresponsive when you attempt to communicate or shake them.
- Absence of Breathing: The individual may stop breathing or exhibit irregular, gasping breaths.
- Loss of Pulse: A strong pulse may no longer be felt at the neck or wrist, indicating that the heart is no longer pumping blood.
Identifying the Severity
In some cases, the symptoms of cardiac arrest can be mistaken for other medical conditions, so it’s important to assess the situation quickly. If any of the following are observed, immediate intervention is necessary:
- Sudden collapse without warning or after a brief period of chest discomfort.
- Complete unresponsiveness, with no eye movement or response to external stimuli.
- Complete cessation of regular breathing or presence of only gasping breaths.
Recognizing these symptoms early is essential for prompt action, including starting chest compressions and using an AED if available. Early defibrillation and continuous care can dramatically increase the chances of survival in cases of cardiac arrest.
Importance of Timely Defibrillation
In emergency situations where the heart stops beating effectively, restoring its rhythm is crucial for survival. Timely defibrillation is one of the most effective ways to treat certain types of cardiac arrest, where the heart experiences irregular or chaotic electrical activity. Without quick intervention, the chances of recovery diminish rapidly, making it vital to act without delay. Early use of a defibrillator can significantly improve outcomes, increasing the likelihood of survival and reducing the risk of long-term damage to the heart and brain.
Why Defibrillation Is Critical
Defibrillation works by delivering a controlled electric shock to the heart, which can reset its electrical activity, allowing it to beat normally again. The primary benefits include:
- Restores Normal Heart Rhythm: By shocking the heart, defibrillation helps re-establish a stable and functional rhythm.
- Increases Survival Rates: Immediate defibrillation within the first few minutes of cardiac arrest significantly increases the chance of survival.
- Minimizes Brain Damage: Restoring blood flow as soon as possible helps prevent brain damage due to a lack of oxygen.
How Quickly Defibrillation Should Be Administered
The window for effective defibrillation is very narrow. Every minute counts when it comes to restoring normal heart function. Here’s a general timeline of how time affects the survival rate:
- Within 1 minute: The survival rate is approximately 90%, with the immediate use of an Automated External Defibrillator (AED).
- After 3 minutes: Survival rates decrease by 7-10% per minute without defibrillation.
- After 10 minutes: The chance of survival drops dramatically, and the likelihood of recovery without severe neurological damage is minimal.
In emergency situations, immediate access to defibrillation equipment and prompt action can make all the difference. It is essential for individuals to know how to use an AED and act quickly when faced with a cardiac arrest victim.
Proper Use of an AED
An Automated External Defibrillator (AED) is a life-saving device that can be used to treat victims of cardiac arrest. It is designed to analyze the heart’s rhythm and, if necessary, deliver a controlled shock to help restore a normal heartbeat. Knowing how to use an AED properly is essential, as timely application can significantly increase the chances of survival and minimize damage to the brain and other vital organs. This section covers the key steps for effectively using an AED in an emergency situation.
Steps for Using an AED
While AEDs are designed to be user-friendly, it is important to follow a clear procedure for optimal effectiveness. The main steps to follow include:
- Turn on the AED: Power on the device by pressing the power button. Most AEDs will provide verbal instructions once activated.
- Prepare the Victim: Ensure the person is lying flat on their back, on a firm surface. Remove any clothing that covers the chest area.
- Apply Electrodes: Place the electrode pads on the bare chest. Follow the visual instructions on the pads for correct placement.
- Allow the AED to Analyze: Once the pads are attached, the AED will automatically analyze the heart’s rhythm. Ensure no one is touching the person during this time.
- Deliver a Shock if Advised: If the AED determines that a shock is needed, it will instruct you to press the shock button. Make sure the area is clear of people before delivering the shock.
- Continue CPR if Needed: If the shock is delivered, continue performing CPR as instructed by the AED until emergency medical services arrive or the person shows signs of life.
Key Considerations When Using an AED
When using an AED, several factors should be kept in mind to ensure both safety and effectiveness:
- Clear Area: Always ensure that no one is touching the victim when the AED is analyzing the heart rhythm or delivering a shock.
- Battery and Maintenance: Ensure the device is regularly maintained and that the battery is charged. Check for any expiry dates on the pads to ensure proper functionality.
- Use AED Immediately: Quick action is essential. The sooner you use an AED after the onset of cardiac arrest, the better the chances of survival.
Proper use of an AED is an invaluable skill in emergencies. With the right training, anyone can confidently operate an AED and potentially save a life.
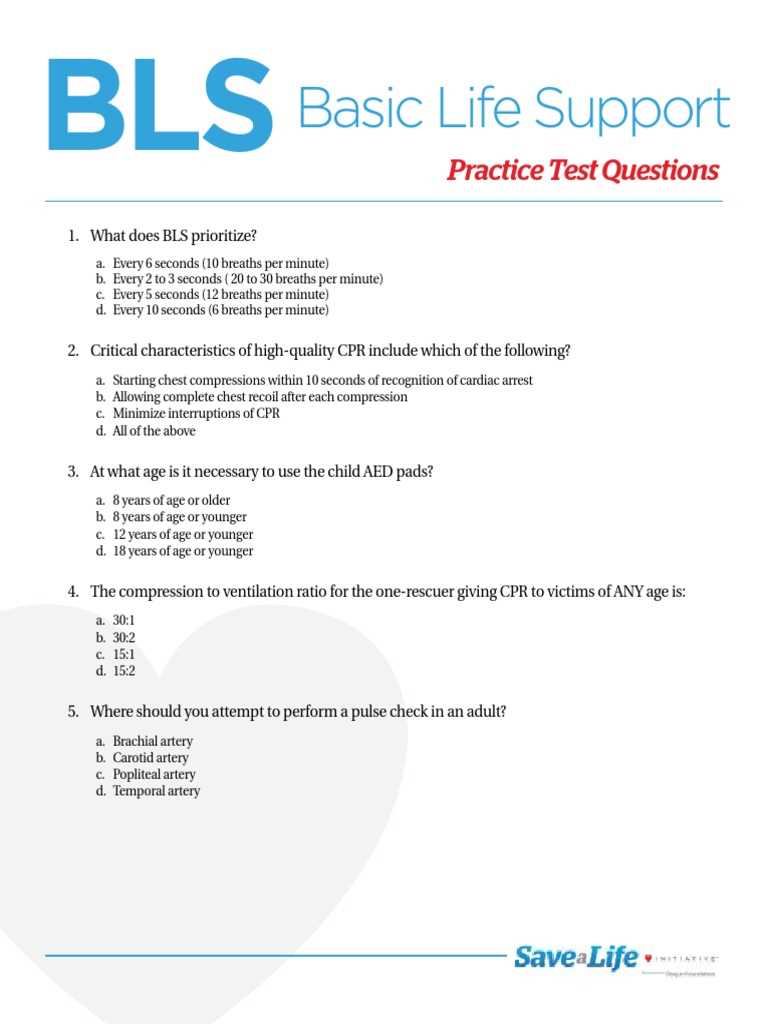
Difference Between Adult and Child BLS
When responding to a medical emergency, it’s important to understand that the procedures for assisting an adult and a child in cardiac distress vary slightly. While the core principles remain the same, there are significant differences in how to approach resuscitation in children compared to adults. These variations are based on the physiological differences between children and adults, such as the size of the body and the structure of the chest, as well as the cause of the emergency. Tailoring the response to these differences is essential for effective care and increasing the chances of survival.
Key Differences in Chest Compressions
One of the most noticeable differences in performing resuscitation between adults and children is the method used for chest compressions:
- Depth of Compressions: For adults, compressions should be at least 2 inches deep, whereas for children, compressions should be about 1/3 of the chest depth, roughly 1.5 inches.
- Hand Placement: In adults, compressions are typically done with both hands on the center of the chest. In children, one hand may be sufficient, or two fingers in infants under one year old.
- Compression Rate: The compression rate remains the same for both adults and children, which is 100 to 120 compressions per minute.
Rescue Breathing and Other Considerations
Another key difference is in the method of rescue breathing and the number of breaths given:
- Rescue Breaths: For both adults and children, two rescue breaths should be given after every set of 30 chest compressions. However, for infants, the breaths should be gentle and should cover the infant’s nose and mouth.
- Use of an AED: In cases of sudden cardiac arrest, adults should receive an AED shock as soon as available. For children aged 1-8, a pediatric-specific AED pad should be used. If unavailable, the adult pads are appropriate but should be placed with care to avoid injury.
Understanding these critical differences ensures that resuscitation is performed correctly and effectively, optimizing the chances of a positive outcome for both adults and children in emergency situations.
Managing Choking Victims in BLS
Choking is a life-threatening situation that can occur when a person’s airway becomes blocked by an object, such as food or a foreign item. When someone is unable to breathe properly, immediate action is required to clear the obstruction and restore normal breathing. Knowing how to handle a choking emergency is crucial for providing effective care until professional help arrives. This section explains the key steps to manage choking incidents and highlights the differences in techniques based on the age of the victim.
Steps for Managing Choking in Adults
For adults and children over one year of age, the following procedures should be followed when dealing with choking:
- Encourage Coughing: If the person is coughing, encourage them to continue. Coughing is the body’s natural response to expel the object from the airway.
- Back Blows: If the person is unable to cough or breathe, give up to five back blows. Stand behind them, support their chest, and deliver forceful blows between the shoulder blades using the heel of your hand.
- Abdominal Thrusts (Heimlich Maneuver): If back blows do not work, perform abdominal thrusts by placing your hands above the person’s navel and applying quick, inward and upward pressure to expel the object.
- Repeat as Necessary: Continue alternating between back blows and abdominal thrusts until the object is expelled or the person becomes unconscious.
Managing Choking in Infants
For infants under one year old, choking management requires a different approach. Since infants’ airways are smaller and more fragile, the following steps should be taken:
- Back Slaps: Place the infant face down on your forearm, supporting the head and neck. Give up to five firm back slaps between the shoulder blades using the heel of your hand.
- Chest Thrusts: If the back slaps do not clear the airway, turn the infant onto their back and deliver up to five chest thrusts. Use two or three fingers in the center of the chest, just below the nipple line, applying quick and gentle thrusts.
- Repeat if Needed: Continue performing back slaps and chest thrusts until the object is dislodged or emergency services arrive.
Key Considerations for Choking Emergencies
The following guidelines are important when managing any choking situation:
| Consideration | Adults and Children Over 1 Year | Infants Under 1 Year |
|---|---|---|
| Back Blows | Up to 5 firm blows between shoulder blades | Up to 5 back slaps between shoulder blades |
| Abdominal Thrusts | Use Heimlich maneuver if the obstruction is not cleared | Do not perform abdominal thrusts |
| Chest Thrusts | Not recommended for adults | Use if back slaps are ineffective |
| Unconscious Victims | Begin CPR if the person becomes unresponsive | Begin CPR and follow choking procedures if the infant becomes unresponsive |
By following these guidelines and recognizing the differences in approach for adults and infants, you can effectively manage a choking emergency and help save a life. Always seek immediate professional medical assistance when needed.
Rescue Breathing Techniques Explained
In emergencies where a person is not breathing or is struggling to breathe, immediate intervention is essential to provide oxygen to the body and prevent further complications. One of the key interventions in such situations is rescue breathing, which helps deliver air to the victim’s lungs when they cannot do so on their own. This technique is vital for maintaining oxygen flow to vital organs until professional help arrives or normal breathing is restored. In this section, we will explore the proper techniques and guidelines for performing rescue breathing.
Rescue breathing should only be performed if the victim is unresponsive and not breathing or breathing abnormally. The following steps outline the procedure for administering rescue breaths effectively:
| Step | Action |
|---|---|
| 1. Check for Breathing | Assess the victim’s chest for movement or listen for breath sounds for up to 10 seconds. If the person is not breathing, proceed to the next step. |
| 2. Open the Airway | Position the victim on their back. Gently tilt their head back and lift their chin to open the airway. This helps prevent the tongue from blocking the throat. |
| 3. Provide Rescue Breaths | Pinch the victim’s nose shut, cover their mouth with yours, and give two slow, steady breaths. Ensure the chest rises with each breath, indicating that air is entering the lungs. |
| 4. Continue with CPR | If the person remains unresponsive and continues to not breathe, resume chest compressions while alternating with rescue breaths until help arrives. |
For adults, two rescue breaths are typically given after every 30 chest compressions, following the standard protocol for CPR. However, for infants and children, the process may vary slightly. The breaths should be given more gently for children and infants, as their lung capacity is smaller. Below is a quick comparison of rescue breathing for different age groups:
| Age Group | Breath Duration | Compression to Breath Ratio |
|---|---|---|
| Adults | 1 second per breath | 30 chest compressions to 2 breaths |
| Children (1 year to puberty) | 1 second per breath | 30 chest compressions to 2 breaths |
| Infants (under 1 year) | 1 second per breath, smaller volume | 30 chest compressions to 2 breaths (with two fingers for compressions) |
It’s important to note that in cases where you are unsure of the victim’s condition or if you are alone, you can perform hands-only CPR, which focuses on chest compressions alone until help arrives. However, when rescue breathing is required, it significantly improves the chances of survival, especially in cases of cardiac arrest caused by respiratory issues.
Performing rescue breathing correctly is critical in preserving brain function and preventing severe damage to vital organs. Remember, prompt action can be life-saving, so always call emergency services immediately if you find yourself in such a situation.
Handling Unresponsive Victims Safely
When encountering an individual who is unresponsive, it is crucial to handle the situation with care and urgency to ensure their safety. Immediate action can prevent further harm, but it’s equally important to avoid causing additional injuries during the rescue process. This section will cover the necessary steps to manage unresponsive victims effectively while minimizing risks to both the victim and the rescuer.
The first step when approaching an unresponsive person is to assess their condition and determine if they are breathing. In cases where the victim is unresponsive but breathing, placing them in a recovery position is essential. This position helps keep their airway clear and prevents choking. However, if the victim is not breathing or has irregular breathing, more urgent actions such as starting chest compressions or rescue breathing may be required.
Properly Checking for Responsiveness
Before taking further steps, it’s essential to check if the victim is responsive. This can be done by gently tapping their shoulder and shouting loudly to see if they respond. If there is no response, it’s critical to immediately call emergency services and proceed with life-saving techniques.
Steps to Safely Handle an Unresponsive Victim
- Assess Breathing: Check if the victim is breathing normally. If not, prepare to perform CPR.
- Clear the Airway: Tilt the head back and lift the chin to open the airway, ensuring it’s free from obstructions.
- Recovery Position: If the person is breathing but unresponsive, carefully roll them onto their side to prevent choking. This helps clear the airway and allows fluids to drain from the mouth.
- CPR if Necessary: If the person is not breathing, start chest compressions and rescue breaths immediately.
For infants and children, the handling process may differ slightly. For example, infants should be placed on their back with their head slightly lower than the body to help keep the airway open. Additionally, the force used in compressions should be gentle, considering the size and fragility of young victims.
Throughout the process, it’s important to stay calm and focused. Clear communication with any bystanders is also essential to coordinate further actions and ensure the safety of the victim.
In all cases, once professional help arrives, follow their instructions and provide the necessary information about the victim’s condition and the actions already taken.
Understanding the Chain of Survival
The Chain of Survival is a critical concept that outlines the essential steps needed to improve the chances of survival following a sudden cardiac event or medical emergency. It consists of interconnected actions, each of which plays a vital role in delivering timely care. A prompt and effective response is crucial for increasing the victim’s odds of recovery. This section delves into the key elements of the Chain of Survival and their significance in emergency response situations.
Key Links in the Chain
The Chain of Survival is typically divided into several key stages, each building upon the last. These steps include:
- Early Recognition and Early Access to Help: Recognizing a medical emergency as soon as it occurs and calling for help immediately is the first and most important step. Quick access to professional assistance significantly increases survival rates.
- Early CPR: Performing chest compressions and rescue breaths can help sustain circulation and oxygen flow to vital organs while awaiting advanced medical care.
- Early Defibrillation: Using an automated external defibrillator (AED) within minutes of cardiac arrest can restore normal heart rhythm, greatly improving survival chances.
- Advanced Life Support: Once emergency responders arrive, they can provide advanced treatments like medications and other interventions to stabilize the victim.
- Post-Resuscitation Care: Proper follow-up care in the hospital is necessary to ensure long-term recovery and reduce the risk of further complications.
The Importance of Early Action
Each link in the Chain of Survival is crucial for optimizing outcomes. Delays in any stage can reduce the chances of a successful recovery. Early recognition and intervention are especially critical, as they buy the victim valuable time until professional help arrives. When people are trained to recognize emergencies and respond quickly, they can make a life-saving difference.
By understanding and applying the steps of the Chain of Survival, individuals and communities can enhance their ability to respond effectively to sudden medical emergencies, ultimately saving lives.
Critical Mistakes to Avoid in BLS
Responding to medical emergencies requires quick thinking and precise actions. While many individuals have been trained to handle such situations, it’s easy to make mistakes that can compromise the outcome. Understanding common errors and knowing how to avoid them is crucial in ensuring the best possible chances for recovery. This section highlights critical mistakes to avoid when providing emergency assistance, helping responders improve their effectiveness and minimize risks.
Common Mistakes to Avoid
There are several common pitfalls that responders may encounter in emergency scenarios. These errors can hinder the victim’s recovery and, in some cases, lead to further complications:
- Failure to Assess the Situation: One of the most important first steps is ensuring the scene is safe before taking any action. Failure to quickly assess the environment can expose both the responder and the victim to unnecessary danger.
- Incorrect Chest Compression Depth: Proper chest compression depth is essential for circulating blood effectively. Compressions that are too shallow or too deep can compromise the victim’s chances of survival.
- Inadequate Ventilation: Providing rescue breaths is crucial for oxygenating the victim’s lungs. Shallow breaths or insufficient air volume can limit oxygen flow, reducing the effectiveness of the intervention.
- Delayed Use of AED: Delaying the use of an automated external defibrillator (AED) can significantly decrease the victim’s chances of survival. It is important to use the AED as soon as possible after cardiac arrest is suspected.
- Failure to Continue Until Help Arrives: Stopping CPR prematurely or giving up too soon can be detrimental. It’s essential to continue until professional medical help arrives or the victim shows signs of recovery.
Strategies for Effective Response
Avoiding these critical mistakes requires both knowledge and practice. Regular training, staying calm, and adhering to established guidelines are key to providing efficient and effective emergency care. Responders should remain confident in their abilities and make sure to follow the proper procedures without hesitation.
By recognizing and avoiding these common errors, individuals can increase their chances of delivering life-saving care during a medical emergency, improving outcomes for the victims they assist.
Reviewing BLS Exam A Answer Key
In order to improve performance and understanding of emergency care techniques, reviewing the solution guide for any assessment is essential. This helps reinforce correct procedures and clarify any areas of confusion. In this section, we will walk through common questions typically found in this type of evaluation, focusing on the key concepts and the rationale behind each correct response. This will provide a comprehensive review of critical actions that are vital for responders in emergency situations.
Key Areas Covered in the Evaluation
The review process involves analyzing the most important concepts, which are often tested during the assessment. By revisiting these questions and their corresponding answers, individuals can solidify their understanding and ensure they are ready for real-life scenarios. Here are some of the core areas that are commonly assessed:
- Recognition of Medical Emergencies: Understanding when and how to intervene during emergencies such as cardiac arrest, respiratory failure, or choking.
- Chest Compression Techniques: The correct depth, rate, and timing for performing effective chest compressions to maintain circulation.
- Rescue Breathing Methods: Proper techniques for providing artificial ventilation to victims who are not breathing, ensuring sufficient oxygenation.
- Use of AED: Identifying when to deploy an automated external defibrillator (AED) and the steps for its correct use.
- Scene Safety and Patient Assessment: Evaluating the environment and ensuring the area is secure before beginning any intervention.
Why Reviewing is Important
After taking the assessment, revisiting the solution guide helps confirm your understanding of each step. It’s also an opportunity to highlight common misconceptions or mistakes, and learn from them. Here’s why reviewing the answer key is beneficial:
- Clarification: By revisiting the solution key, you can clear up any uncertainties regarding specific procedures and protocols.
- Reinforcement: Regularly reviewing key concepts strengthens your knowledge and enhances memory retention, making you more confident in applying the skills during real situations.
- Better Preparedness: Understanding the correct answers helps you feel more confident when responding to actual medical emergencies.
- Identifying Improvement Areas: The review process may highlight areas that need further study or practice, allowing you to refine your skills and techniques.
By thoroughly reviewing the solution guide, you ensure that you are well-prepared for any situation requiring immediate medical assistance, allowing you to act quickly and effectively when needed the most.
Final Tips for BLS Exam Preparation
As you approach the assessment for emergency medical response techniques, it’s important to ensure you are well-prepared and confident in your skills. A thorough understanding of the critical steps involved in responding to medical crises can make all the difference in a real-life situation. This section offers some final advice to help you optimize your preparation and ensure you are ready for the challenges the evaluation may present.
First and foremost, review the key concepts thoroughly. Familiarity with the proper techniques for recognizing medical emergencies, performing effective chest compressions, administering rescue breathing, and using an AED is essential. Understanding each of these steps will not only help you pass the test but will also equip you to respond correctly when needed.
In addition to reviewing the content, practice is key. Repeatedly practicing the steps in a simulated environment will help you build muscle memory, ensuring you can perform the procedures effectively and confidently under pressure. Many training centers offer hands-on practice sessions, and it’s important to take advantage of these opportunities to practice with peers or instructors who can provide feedback.
Another useful tip is to create a study schedule leading up to the assessment. Break down your study time into manageable sections, focusing on one technique or concept at a time. Make sure to revisit any areas you find challenging, and allocate extra time for those topics. Don’t forget to also rest and take breaks to avoid burnout, as mental clarity is crucial for effective learning.
Finally, stay calm and confident during the test. Knowing that you’ve prepared thoroughly will allow you to approach the assessment with composure. Remember, the evaluation is not just about memorizing information but about demonstrating your ability to think critically and apply techniques when faced with a crisis. The more calm and focused you remain, the better your performance will be.