Effective understanding of heart activity through diagnostic tools plays a vital role in the medical field. Properly analyzing electrical signals from the heart enables healthcare professionals to detect abnormalities, assess overall cardiac health, and determine appropriate treatments.
For those preparing to assess complex heart signals, it’s essential to become familiar with various patterns and disturbances that can indicate underlying health conditions. Mastery in reading these signals is crucial, not only for clinical practice but also for excelling in related assessments. Accurate interpretation is key to ensuring timely and correct interventions for patients in critical care.
In this guide, we will explore the key strategies and tips for effectively mastering the intricacies of heart signal analysis. Understanding core principles, recognizing common patterns, and avoiding common pitfalls will help in achieving success in practical applications and examinations alike.
Heart Signal Analysis and Assessment Techniques
Accurate evaluation of cardiac electrical activity is essential for diagnosing various heart conditions. Understanding the distinct patterns produced by the heart allows practitioners to identify abnormalities and ensure proper treatment. This section delves into the critical aspects of heart signal analysis, providing the knowledge needed for success in practical assessments.
Key Concepts for Effective Cardiac Assessment
Familiarity with heart patterns and their implications is fundamental for any healthcare professional involved in monitoring heart function. It is important to grasp the significance of different waveforms and intervals that appear on diagnostic charts. A systematic approach to identifying irregularities, such as arrhythmias or blockages, ensures quicker diagnosis and more accurate treatment plans. Comprehensive understanding of these concepts helps in mastering the art of heart signal reading.
Avoiding Common Mistakes During Analysis
Common errors in identifying heart abnormalities often arise from misinterpreting subtle differences in heart patterns. Practitioners must develop the ability to recognize these variations and interpret them with precision. Being aware of typical pitfalls, such as overlooking minor wave irregularities or confusing similar conditions, helps increase accuracy. Attention to detail and consistent practice are crucial for refining this skill.
Understanding Heart Signal Basics
Accurate analysis of heart activity is vital for diagnosing various cardiovascular conditions. The electrical impulses generated by the heart create patterns that provide essential information about its function. A clear understanding of these basic signals is the foundation for recognizing irregularities and making informed medical decisions.
Components of Heart Electrical Activity
The heart’s electrical system produces a series of waveforms that correspond to different phases of cardiac function. These waveforms are typically recorded during diagnostic procedures. Understanding how each component of the waveform correlates to the heart’s actions is essential for proper assessment and diagnosis.
| Waveform | Phase of Cardiac Cycle | Significance |
|---|---|---|
| P wave | Atrial depolarization | Indicates the electrical impulse passing through the atria |
| QRS complex | Ventricular depolarization | Reflects the electrical impulse traveling through the ventricles |
| T wave | Ventricular repolarization | Shows the recovery phase of the ventricles after contraction |
Key Considerations for Accurate Reading

Mastering the basics of heart signals involves recognizing the distinct patterns and intervals that correspond to each phase of the heart cycle. By understanding the duration and appearance of waveforms, practitioners can more accurately identify irregularities and assess heart function. Consistent practice and attention to detail are critical for improving this skill over time.
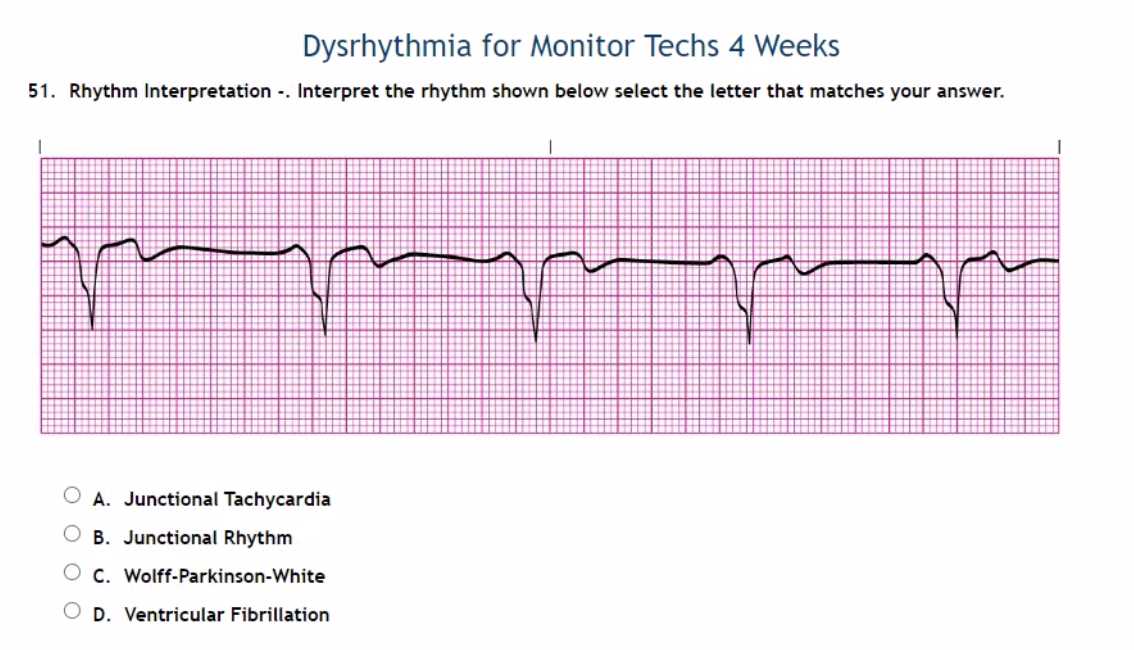
Common Heart Activity Patterns You Should Know
Being able to recognize common heart activity patterns is essential for effective diagnosis and treatment. These patterns provide valuable insights into the heart’s electrical behavior, allowing healthcare providers to identify normal and abnormal conditions. Familiarity with these patterns is the first step in mastering the process of heart signal analysis.
Below are some of the most common patterns observed during cardiac monitoring:
- Normal Sinus Rhythm: This is the typical heart activity pattern, with regular intervals and a consistent rate. It indicates a healthy heart functioning correctly.
- Atrial Fibrillation: Characterized by an irregular, often rapid heart rate, this pattern signals disorganized electrical impulses in the atria, leading to ineffective heart contractions.
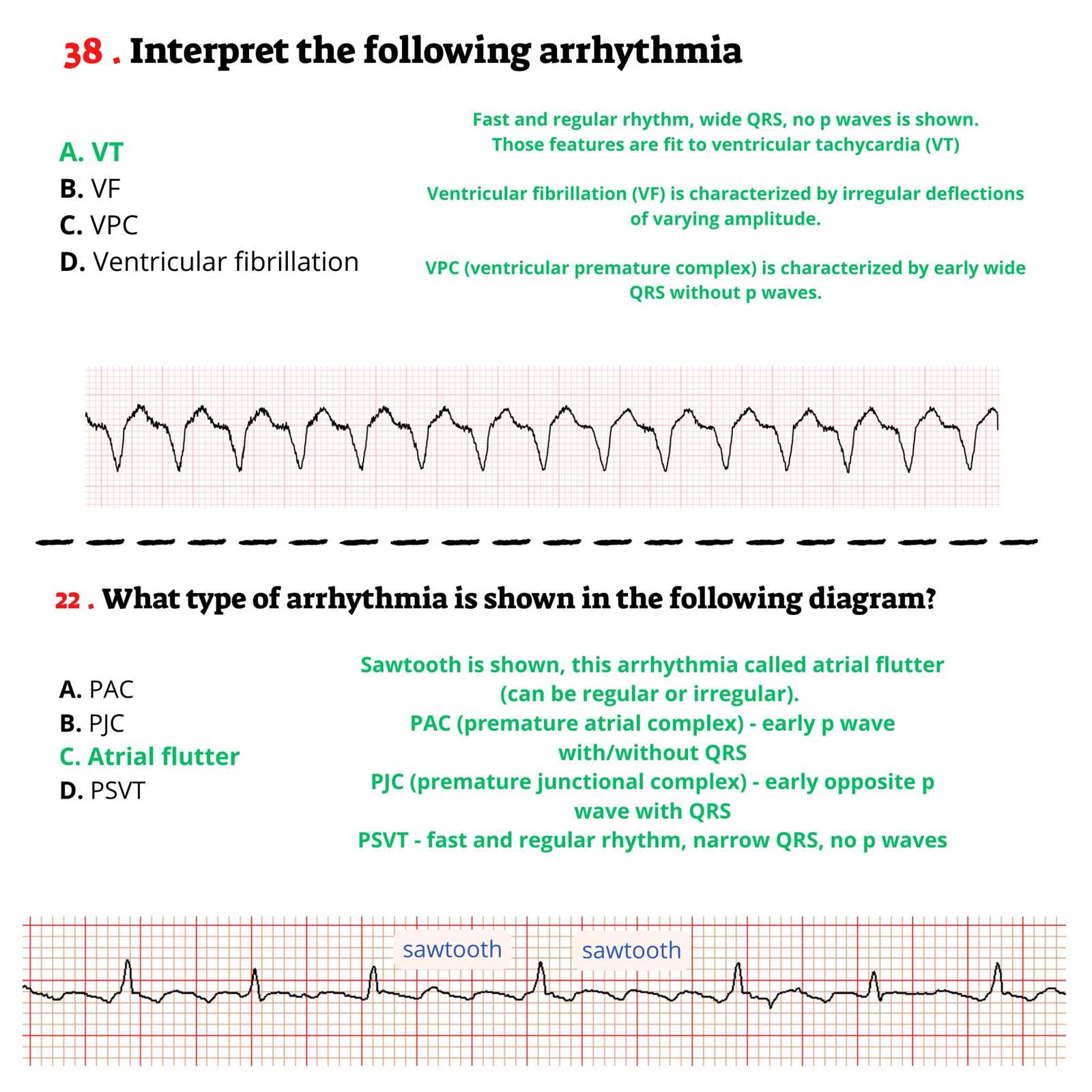
- Ventricular Tachycardia: This rapid rhythm originates in the ventricles and can be life-threatening if not addressed promptly.
- Bradycardia: A slower-than-normal heart rate, which can sometimes be a sign of an underlying health issue, particularly in older adults.
- Premature Ventricular Contractions (PVCs): These extra heartbeats originate in the ventricles and can cause irregular heartbeats, though they are often benign.
Each of these patterns provides critical information about the heart’s electrical system and should be recognized quickly during patient assessments. Understanding their key features helps healthcare professionals make timely and informed decisions.
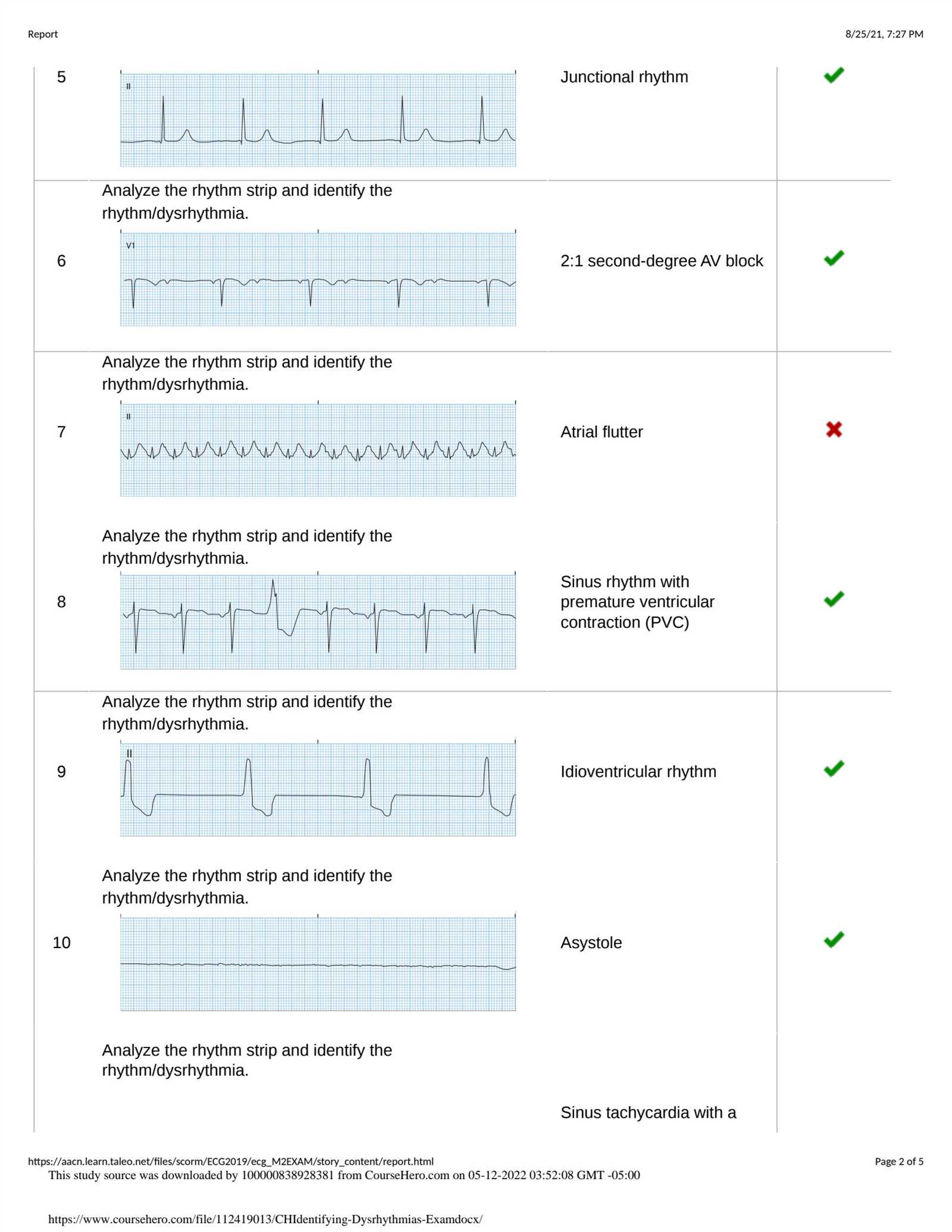
How to Identify Arrhythmias on Heart Monitoring

Recognizing abnormal heart rhythms is crucial for diagnosing cardiovascular conditions. Arrhythmias, or irregular heartbeats, can be life-threatening if left untreated. Identifying these disturbances through monitoring allows healthcare providers to take timely action and provide appropriate treatment. Early detection of arrhythmias improves patient outcomes and prevents complications.
Here are key steps to help identify arrhythmias effectively:
- Examine the heart rate: A significantly fast or slow heart rate may indicate an arrhythmia. A normal rate typically falls between 60 and 100 beats per minute in a healthy adult.
- Analyze the regularity: Look for consistency in the intervals between heartbeats. Irregular timing, especially with uneven spacing, is often a sign of an arrhythmia.
- Assess the waveform shape: Abnormalities in the waveform, such as a distorted P wave or a wide QRS complex, may signal issues with the heart’s electrical conduction system.
- Observe for missing beats: A skipped or extra beat can be a sign of premature contractions, which may suggest the presence of certain arrhythmias like PVCs (premature ventricular contractions).
Common arrhythmias to watch for include:
- Atrial Fibrillation: An irregular and often rapid heart rate caused by chaotic electrical impulses in the atria.
- Ventricular Tachycardia: A fast and dangerous rhythm originating from the ventricles, which can lead to cardiac arrest if not treated immediately.
- Bradycardia: A slower-than-normal heart rate, which can result from several underlying conditions, such as heart block.
- Premature Beats: These occur when the heart beats earlier than expected, often causing an irregular or skipped beat sensation.
Accurate identification of these irregularities is critical for appropriate treatment and management. Regular practice and familiarity with heart signals will enhance your ability to detect arrhythmias efficiently.
Key Concepts in Cardiac Electrical Activity
Understanding the heart’s electrical system is fundamental to diagnosing and treating various cardiac conditions. The heart generates electrical impulses that regulate its contractions, ensuring a coordinated and efficient pumping action. By learning the basic principles behind these electrical signals, healthcare professionals can accurately assess heart function and detect abnormalities.
The Electrical Conduction Pathway
The heart’s electrical activity begins with the sinoatrial (SA) node, which initiates the electrical impulse. This impulse travels through the atria, causing them to contract. It then reaches the atrioventricular (AV) node, where the signal is briefly delayed before passing through the bundle of His and Purkinje fibers to stimulate the ventricles. This sequence ensures that the heart beats in a regular and synchronized manner.
Understanding Key Electrical Waveforms
The heart’s electrical impulses are captured as waveforms on diagnostic monitors. These waveforms represent different phases of the cardiac cycle and are essential for understanding the heart’s function. The main components of these signals include:
- P wave: Represents atrial depolarization, the initial electrical activity of the atria.
- QRS complex: Indicates ventricular depolarization, the electrical activity that triggers the ventricles to contract.
- T wave: Reflects ventricular repolarization, the recovery phase of the ventricles after contraction.
Familiarity with these waveforms and their relationships is crucial for identifying normal and abnormal heart activity.
Steps for Accurate Heart Signal Analysis
Accurately analyzing heart activity is essential for identifying both normal and abnormal conditions. Following a structured approach ensures consistency and precision in interpreting complex cardiac patterns. By adhering to a set of key steps, healthcare professionals can enhance their ability to diagnose and manage heart-related issues effectively.
Step 1: Assess the Heart Rate
The first step in any analysis is to evaluate the heart rate. A normal heart rate in a resting adult is typically between 60 and 100 beats per minute. If the rate is outside of this range, further investigation is needed to determine if the rhythm is too fast (tachycardia) or too slow (bradycardia). It is crucial to calculate the number of beats over a set period to establish whether the rate is within a healthy range.
Step 2: Analyze the Regularity
After assessing the heart rate, the next step is to check the regularity of the heartbeats. This involves measuring the intervals between consecutive heartbeats. Healthy heart activity is usually regular, with consistent intervals. Irregular intervals may indicate arrhythmias or other electrical disturbances. Identifying patterns of irregularity can help in diagnosing the underlying condition.
Incorporating these steps into the analysis process provides a clear and organized method for identifying heart abnormalities. By practicing and refining these techniques, practitioners can improve their diagnostic accuracy and responsiveness to patient needs.
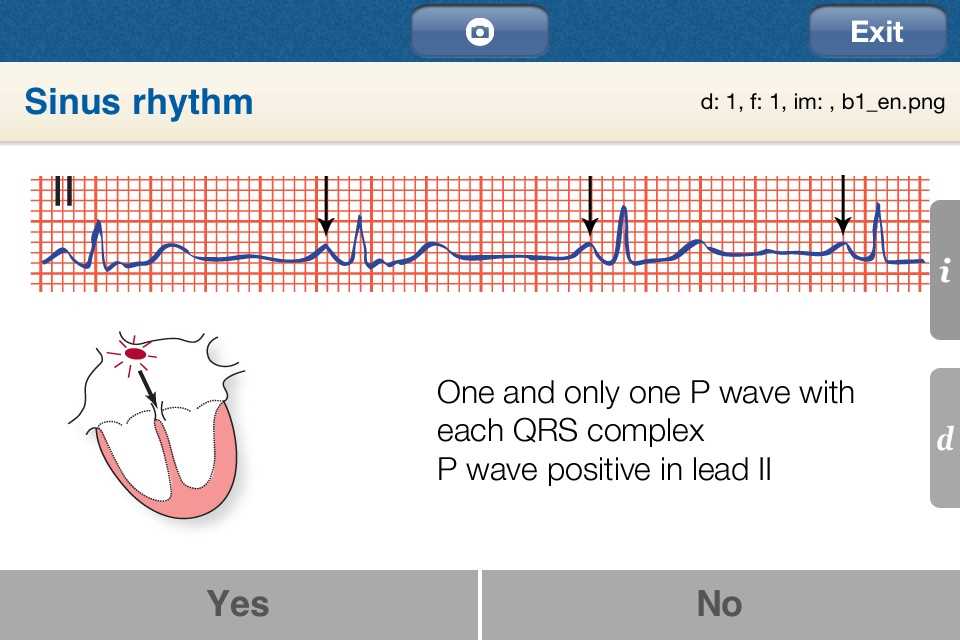
Decoding Sinus Rhythms on Heart Monitoring
Understanding normal heart activity is essential for identifying healthy cardiac function. The sinus rhythm is the typical electrical pattern generated by the heart, originating from the sinus node. This pattern ensures the heart beats in a coordinated and consistent manner, providing the foundation for accurate diagnosis and treatment. Recognizing this normal rhythm is the first step in evaluating the heart’s electrical activity.
Identifying Key Characteristics of Sinus Rhythm
A healthy sinus rhythm has several defining features that distinguish it from abnormal heart patterns. These include:
- Consistent heart rate: The heart rate typically ranges from 60 to 100 beats per minute, with regular intervals between beats.
- Clear P wave: Each heartbeat is preceded by a P wave, which represents the depolarization of the atria.
- Regular spacing: The intervals between heartbeats are consistent, with no irregularity in the timing of successive beats.
- Normal QRS complex: The QRS complex, which represents ventricular depolarization, should be narrow and consistent in appearance.
Why Sinus Rhythm Matters
Identifying sinus rhythm is essential for differentiating between normal and abnormal heart conditions. Any deviation from this standard pattern may indicate an underlying issue such as arrhythmia, which requires further investigation. By recognizing the key components of sinus rhythm, healthcare providers can accurately assess cardiac function and take appropriate steps for treatment if necessary.
Recognizing Atrial Fibrillation in Heart Monitoring
Atrial fibrillation (AFib) is one of the most common types of irregular heart activity. It occurs when the electrical impulses in the heart become disorganized, leading to rapid and erratic atrial contractions. This results in an irregular and often fast heartbeat, which can increase the risk of stroke and other complications if not managed properly. Detecting AFib early is crucial for effective treatment and preventing further health issues.
Identifying Key Features of Atrial Fibrillation
There are several characteristic signs that indicate the presence of atrial fibrillation in heart activity:
- Irregularly irregular rhythm: One of the hallmark features of AFib is an unpredictable and irregular interval between heartbeats, with no consistent pattern.
- Absence of P waves: In AFib, the typical P waves, which represent atrial contraction, are absent. Instead, there is a chaotic baseline, often referred to as fibrillatory waves.
- Rapid ventricular response: The ventricles may beat faster than normal, resulting in a heart rate that exceeds 100 beats per minute, although it can be slower in some cases.
Why Early Detection is Important
Early identification of atrial fibrillation allows for prompt intervention and reduces the risk of complications, such as stroke or heart failure. Treatment options may include medications, lifestyle changes, and sometimes procedures to restore normal heart rhythm. By learning how to recognize the distinct features of AFib, healthcare professionals can better assess patient health and take the necessary steps for management and care.
Identifying Ventricular Tachycardia Patterns
Ventricular tachycardia (VT) is a serious and potentially life-threatening condition where the heart’s lower chambers beat too quickly, preventing them from filling properly. This can lead to reduced cardiac output and even cause cardiac arrest if not promptly managed. Recognizing the distinctive patterns associated with VT is crucial for timely diagnosis and intervention.
Key Characteristics of Ventricular Tachycardia
There are several hallmark signs that help identify ventricular tachycardia in heart monitoring:
- Wide QRS complexes: One of the most prominent features of VT is the appearance of wide and bizarre QRS complexes. These occur due to the abnormal conduction of electrical signals through the ventricles.
- Rapid heart rate: VT typically presents with a heart rate of over 100 beats per minute, often reaching 150-250 beats per minute, which is much faster than normal.
- Monomorphic or polymorphic patterns: In some cases, the QRS complexes may appear identical (monomorphic), while in other cases, they may vary in shape (polymorphic), depending on the underlying cause of the tachycardia.
Recognizing VT for Timely Intervention
Promptly identifying ventricular tachycardia can be life-saving. If not treated, VT can progress to more severe arrhythmias such as ventricular fibrillation, which may lead to sudden cardiac arrest. Early recognition through heart monitoring allows healthcare providers to implement interventions such as antiarrhythmic medications, electrical cardioversion, or other life-saving treatments.
Understanding Heartwave Patterns and Intervals
Accurate interpretation of heart activity relies on understanding the various waveforms and intervals that represent the electrical events of the cardiac cycle. These waveforms reflect the depolarization and repolarization of different parts of the heart, and the timing between them provides valuable insights into heart health. A thorough understanding of these components is essential for identifying normal and abnormal heart function.
Key Waveforms in Cardiac Activity
The heart’s electrical activity is represented by several distinct waveforms, each of which corresponds to a specific part of the heart’s electrical cycle:
- P wave: The P wave represents atrial depolarization, the electrical impulse that triggers the contraction of the atria.
- QRS complex: This complex represents the depolarization of the ventricles and is the most prominent feature of the heart’s electrical activity.
- T wave: The T wave reflects ventricular repolarization, the process by which the ventricles reset after contracting.
Intervals and Their Significance
In addition to waveforms, the timing between these waves is crucial for assessing the heart’s function. The intervals between these events are measured to ensure that the heart is functioning efficiently:
- PR interval: The PR interval represents the time between atrial depolarization and ventricular depolarization, and it should typically last between 120 and 200 milliseconds.
- QT interval: The QT interval measures the time it takes for the ventricles to depolarize and repolarize. Prolonged or shortened QT intervals can be a sign of underlying issues such as arrhythmias or electrolyte imbalances.
- RR interval: The RR interval measures the time between successive R waves and is important for determining heart rate.
By analyzing the relationship between waveforms and their respective intervals, healthcare professionals can evaluate the regularity and efficiency of heart activity, identify abnormalities, and make informed decisions about patient care.
How to Spot Heart Block on EKG
Heart block occurs when there is a delay or complete block in the conduction of electrical impulses between the heart’s chambers. This disruption can lead to abnormal heart rhythms and affect the heart’s ability to pump blood efficiently. Detecting heart block early through heart monitoring is crucial for determining the severity of the condition and implementing appropriate treatments.
To identify heart block, healthcare providers look for specific patterns on heart activity recordings that indicate a delay or failure in the conduction of electrical signals. The primary feature to watch for is an abnormal PR interval, which can be prolonged in varying degrees, depending on the severity of the block. Other indicators may include missing or dropped beats, where a P wave does not lead to a QRS complex.
Heart block is categorized into three degrees:
- First-degree heart block: The PR interval is longer than usual, but every atrial impulse still leads to a ventricular contraction.
- Second-degree heart block: Some atrial impulses fail to reach the ventricles, resulting in dropped beats. This type is further divided into Mobitz type I (Wenckebach) and Mobitz type II, with different patterns of dropped beats.
- Third-degree heart block: Also known as complete block, no electrical signals reach the ventricles from the atria, resulting in complete dissociation between atrial and ventricular activity.
Recognizing these patterns on heart monitoring allows clinicians to make informed decisions about treatment, which may include medication, pacemaker insertion, or other interventions to restore normal heart function.
Common Heart Activity Analysis Mistakes
When reviewing heart activity recordings, even experienced healthcare professionals can make errors in their assessments. These mistakes can lead to incorrect diagnoses or delayed treatments, which may negatively impact patient outcomes. Understanding the most common errors can help improve accuracy and ensure timely and effective care.
Some of the most frequent mistakes in analyzing heart activity involve misidentifying waveforms, incorrectly measuring intervals, or overlooking subtle signs of abnormalities. These errors are often the result of rushing through the analysis or misinterpreting normal variations as pathological conditions. Below is a table that highlights some of the most common mistakes and how to avoid them:
| Common Mistake | Explanation | How to Avoid |
|---|---|---|
| Misidentifying P waves | In some cases, the P wave may be hard to distinguish due to artifacts or irregularities. This can lead to incorrect assumptions about atrial activity. | Ensure proper calibration and take time to carefully observe the waveform morphology. Look for consistent patterns across several cycles. |
| Overlooking abnormal intervals | Failing to identify prolonged PR or QT intervals can lead to missing serious conditions such as heart block or arrhythmias. | Systematically measure and compare intervals. A detailed analysis of each interval is crucial for an accurate assessment. |
| Confusing normal variants with abnormalities | Normal variations, such as sinus arrhythmia, can be misinterpreted as pathological irregularities. | Be familiar with common variations and ensure that abnormal patterns are consistently recurring and not simply due to normal fluctuations. |
| Underestimating the importance of rate | Not calculating the heart rate correctly can lead to missing signs of tachycardia or bradycardia, which are essential in diagnosis. | Carefully calculate the heart rate using the correct method, paying attention to the time intervals between key points such as R waves. |
By understanding and avoiding these common mistakes, clinicians can improve their accuracy when analyzing heart activity and provide better care for patients with potential cardiac issues.
Reviewing Diagnostic Criteria for Heart Activity Patterns
Accurate diagnosis of heart conditions relies heavily on a detailed assessment of electrical activity patterns. Understanding the key diagnostic criteria for identifying various heart conditions is essential for healthcare professionals to provide effective treatment. This section will guide you through the main characteristics and key markers to look for when analyzing these patterns.
Essential Diagnostic Features
When reviewing heart activity, certain features must be considered to ensure an accurate diagnosis. Here are the main aspects to focus on:
- Wave Morphology: Analyzing the shape and structure of waves, such as the P wave, QRS complex, and T wave, helps determine the origin and timing of heart signals.
- Interval Measurement: Correctly measuring intervals, such as the PR interval or QT interval, provides critical information about conduction time and potential delays in the electrical pathway.
- Heart Rate: Calculating the heart rate is vital for identifying arrhythmias like tachycardia or bradycardia, as well as irregular heartbeats.
- Regularity: Observing the regularity of beats is crucial for diagnosing conditions such as atrial fibrillation or other irregularities.
Key Markers for Specific Conditions
Each heart condition exhibits distinct markers that can aid in diagnosis. Here are some important features associated with common heart disorders:
- Atrial Fibrillation: Irregular and often rapid electrical activity with no distinct P waves.
- Ventricular Tachycardia: Broad, abnormal QRS complexes with a fast heart rate.
- Heart Block: Prolonged PR intervals with delayed or absent conduction through the AV node.
- Sinus Arrhythmia: Varying intervals between heartbeats, typically related to respiration.
By focusing on these critical criteria, clinicians can ensure a more accurate diagnosis of heart conditions, leading to better patient outcomes. Identifying these characteristics accurately helps in distinguishing between normal and pathological patterns, allowing for timely intervention.
Practical Tips for EKG Exam Success
Achieving success in understanding heart activity assessments requires not only knowledge but also effective strategies for mastering the material. Whether you are preparing for a certification or just improving your diagnostic skills, employing a few practical techniques can significantly enhance your performance. This section offers tips to help you focus on key areas and prepare efficiently for any related tests.
Focus on Core Concepts
To excel in any test, it’s essential to understand the fundamental concepts. When studying heart activity patterns, make sure to grasp the following key areas:
- Understanding Waveforms: Learn to identify and differentiate between various waveforms, including P waves, QRS complexes, and T waves.
- Measuring Intervals: Practice calculating intervals such as PR, QRS, and QT, as they provide critical information about heart conduction.
- Recognizing Patterns: Familiarize yourself with common patterns like normal sinus rhythm, arrhythmias, and other abnormalities.
Study Smart: Techniques and Strategies
How you study can make all the difference. Consider using the following methods to boost your understanding and recall during testing:
- Practice with Real-World Examples: Use case studies or sample recordings to familiarize yourself with real-life scenarios.
- Create Flashcards: Flashcards are great for memorizing key features of heart activity, such as normal versus abnormal intervals and wave characteristics.
- Group Study Sessions: Studying with peers allows for discussions that can help reinforce your knowledge and clarify difficult concepts.
- Take Timed Quizzes: Practice under time constraints to simulate test conditions and improve speed and accuracy.
By focusing on these areas and employing effective study methods, you will be better prepared for the challenges ahead. Consistent practice, attention to detail, and strategic studying can significantly improve your performance and increase your chances of success in any assessment of heart activity analysis.
Interpreting EKGs in Real-World Cases
In clinical practice, the ability to analyze heart activity data and recognize key patterns is critical for diagnosing patients accurately. While theoretical knowledge forms the foundation, the application of that knowledge in real-world cases is where true diagnostic expertise is developed. This section focuses on how to approach and interpret heart activity recordings in practical, everyday clinical scenarios.
Real-World Challenges in Heart Activity Analysis
Unlike textbook examples, real-life cases often present with more complexity. Factors such as patient age, comorbidities, and medication use can all influence the heart’s electrical behavior, making interpretation more challenging. Some of the key challenges you might encounter include:
- Unclear Waveforms: Patient variability may lead to unusual or distorted waveforms, which can be harder to read and interpret accurately.
- Multiple Abnormalities: Patients may have more than one irregularity, such as concurrent arrhythmias or conduction blocks, making diagnosis more complex.
- Interference or Artifacts: Electrical interference or physical movement during testing may affect the clarity of the results, requiring a careful review to avoid false interpretations.
Steps for Effective Analysis in Clinical Settings
When interpreting heart activity in real-world scenarios, consider these practical steps to ensure accuracy and reliability:
- Always Review Patient History: A thorough understanding of the patient’s medical background, including any preexisting conditions or medications, is essential for making informed decisions.
- Confirm Proper Equipment Setup: Ensure that all leads are placed correctly and that there is no interference from external sources that could distort the data.
- Analyze Each Waveform Systematically: Take the time to examine each wave, interval, and segment. Look for irregularities in the P wave, QRS complex, and T wave, paying attention to the relationship between these components.
- Consult with Colleagues: When in doubt, collaboration with other healthcare professionals can provide valuable insights, especially when complex cases arise.
Mastering the art of heart activity analysis in real-world cases requires both knowledge and experience. By practicing systematic review, addressing common challenges, and learning from each case, you can enhance your ability to interpret and diagnose accurately under diverse clinical conditions.
Resources for Further Study in Cardiac Signal Analysis
For those seeking to deepen their understanding of heart electrical patterns, a variety of educational resources can enhance both theoretical and practical knowledge. From textbooks to online platforms, and mobile apps, there are numerous ways to refine diagnostic skills and gain deeper insights into heart function. Exploring these tools can help learners at all levels strengthen their expertise in identifying and analyzing heart-related abnormalities.
Books for Comprehensive Learning
Books provide a structured approach, allowing learners to explore the science of heart signals and irregularities in detail. Here are a few key titles that offer in-depth knowledge:
| Title | Author(s) | Focus Area |
|---|---|---|
| The Heart’s Electrical Pathways | Dr. Alan Thomas | Introduction to the basic principles of cardiac electrical activity and its clinical significance. |
| Arrhythmia Diagnosis and Management | Dr. Rachel Williams | In-depth coverage of common and complex arrhythmias, along with diagnostic strategies. |
| Clinical Cardiology Essentials | Dr. Samuel Green | A comprehensive guide to understanding the heart’s electrical system and its impact on overall health. |
Online Courses and Platforms
Online courses offer flexible and interactive ways to learn about heart electrical patterns. These platforms provide a combination of videos, quizzes, and practical exercises to help you apply your knowledge:
- Coursera: Offers a variety of courses in cardiovascular health, including heart rhythm analysis and management.
- edX: Features classes from top universities on topics related to heart diseases and diagnostic methods.
- Medmastery: Specializes in interactive clinical courses designed to improve diagnostic skills in real-world settings.
Mobile Apps for Hands-On Practice
Apps provide on-the-go practice, enabling users to enhance their diagnostic abilities through case studies and real-time analysis. These tools are ideal for building confidence and honing skills:
- HeartPro: A comprehensive app for reviewing heart conditions and diagnostics, featuring detailed case studies.
- CardioTutor: This app offers interactive lessons and quizzes to help users understand heart signal patterns and their clinical implications.
- CardioCheck: An app that provides case simulations and diagnostic challenges, helping users recognize and interpret heart abnormalities.
By utilizing these resources, learners can gain the necessary tools to effectively understand and diagnose heart conditions, enhancing both theoretical knowledge and practical application in the field of cardiac diagnostics.
Preparing for the Heart Signal Analysis Assessment
Effective preparation for any certification or assessment in cardiac signal analysis requires a focused approach, with attention to both theoretical knowledge and practical application. By understanding the key components of the test and practicing core skills, learners can approach the evaluation with confidence. This section outlines essential steps for success, highlighting the strategies that will aid in mastering heart signal diagnostics and recognizing irregular patterns.
Study the Core Concepts
Before diving into practice sessions, it’s important to understand the foundational concepts of heart signal analysis. Focus on these key areas:
- Cardiac Anatomy and Physiology: Understand the heart’s structure, its electrical system, and how each part contributes to overall function.
- Signal Identification: Familiarize yourself with different heart waveforms and their meanings, focusing on both normal and abnormal signals.
- Common Heart Abnormalities: Study various conditions such as arrhythmias, blockages, and irregular beats, recognizing their unique signatures on the signal readings.
- Diagnostic Techniques: Master methods for identifying and analyzing patterns, focusing on accurate measurements and effective interpretation strategies.
Practice with Real-World Case Studies
Practical experience is essential for honing skills and gaining confidence. Use case studies to simulate real-world scenarios:
- Review Case Scenarios: Study a variety of case examples, focusing on interpreting different types of cardiac signals and identifying conditions accurately.
- Interactive Simulations: Utilize apps or software that offer interactive exercises to improve speed and accuracy when recognizing abnormal heart patterns.
- Mock Tests: Take mock assessments to practice under exam conditions, helping you improve time management and focus during the real test.
Group Study and Collaboration
Collaborating with peers can be extremely beneficial. Discussing difficult concepts and testing each other’s knowledge will help reinforce your understanding:
- Peer Review: Share your analyses with classmates, getting feedback and insights that may reveal areas for improvement.
- Study Groups: Join or form study groups where you can discuss topics, quiz each other, and tackle challenging problems together.
- Expert Guidance: Seek out experts or mentors in the field who can provide advice and clarify complex topics.
Focus on Time Management
Effective time management is crucial for success. Practicing under timed conditions helps you manage your time efficiently during the assessment:
- Practice Under Pressure: Simulate timed test conditions by completing practice questions within set time limits, helping you stay focused and organized.
- Prioritize Tasks: Identify the areas that you find most challenging and devote extra time to them while keeping your study schedule balanced.
By following these strategies, you will be better prepared to demonstrate your proficiency in heart signal analysis and perform confidently in your upcoming assessment.