Preparing for certification in advanced life-saving techniques is crucial for healthcare professionals. Understanding key protocols, procedures, and assessments ensures the best possible patient outcomes in critical situations. This section provides in-depth guidance on how to effectively navigate the certification process, focusing on essential concepts and common scenarios.
Thorough preparation is necessary to master the skills required for emergency response. Focusing on critical decision-making, timely interventions, and correct administration of medications is key to passing the assessment with confidence. This guide outlines the main areas of focus that are essential to success in these certification challenges.
Every healthcare professional must be equipped with the knowledge to respond rapidly and efficiently in life-threatening situations. By following the structured approach in this article, you can gain the necessary skills and improve your performance, ensuring readiness for high-pressure scenarios.
Comprehensive Guide to Advanced Life Support Certification
For healthcare professionals aiming to enhance their expertise in emergency medical procedures, understanding the comprehensive structure and key components of advanced life support certification is essential. This guide provides an overview of the critical knowledge areas required to navigate the certification process successfully. It focuses on core concepts, decision-making protocols, and practical skills necessary for high-pressure situations where immediate intervention is crucial.
Key Concepts and Procedures
Certification programs in life-saving techniques cover a wide range of topics, from basic life support to advanced pharmacology and rhythm management. A strong grasp of these concepts is fundamental to performing effective interventions during cardiac emergencies. Key procedures include airway management, defibrillation, and medication administration–each of which is essential in stabilizing a patient and improving survival rates.
Practical Application and Testing
The practical application of skills learned during training is evaluated through simulated scenarios. Understanding the step-by-step approach to managing critical situations will ensure that candidates can apply their knowledge confidently. Additionally, knowledge of key algorithms and how to make quick, life-saving decisions plays a pivotal role in passing the assessment.
Key Topics in Advanced Life Support Certification
Understanding the critical areas of focus is essential for those preparing for advanced life-saving certification. These key topics cover a wide range of emergency procedures, from assessing and stabilizing patients to managing complex medical conditions in life-threatening situations. Mastering these concepts ensures healthcare professionals can act swiftly and effectively in high-stress environments.
Cardiac Arrest Management
One of the most vital components of the certification is mastering the protocols for handling cardiac arrest. This includes proper identification of the arrest type, early defibrillation, and administering the appropriate medications. Quick recognition and correct response can significantly improve patient survival rates during critical events.
Pharmacology and Medication Administration
Another key area is the use of drugs in emergency care. Medications such as epinephrine, amiodarone, and atropine play a crucial role in stabilizing patients in various critical situations. Understanding the proper dosages, timing, and indications for these drugs is essential for effective treatment during medical emergencies.
Understanding Advanced Life Support Certification Structure
Knowing the structure of the certification process is crucial for successful preparation. This process is designed to evaluate a healthcare professional’s ability to perform life-saving interventions effectively and efficiently under pressure. It typically involves both theoretical knowledge and practical skills assessment, ensuring that candidates are well-prepared for real-world medical emergencies.
The structure generally includes the following components:
- Theoretical Knowledge: Candidates must demonstrate an understanding of critical concepts, protocols, and procedures related to emergency care.
- Practical Skills Testing: Hands-on scenarios are used to assess the ability to apply knowledge in real-time situations.
- Scoring and Evaluation: A combination of written tests and performance evaluations determines overall competency.
The test also typically includes various sections, each focusing on different aspects of advanced care:
- Assessment of patient condition and diagnosis
- Management of airway and ventilation
- Emergency pharmacology and medication protocols
- Defibrillation and pacing techniques
- Teamwork and communication during critical situations
Success in this structure requires both knowledge and the ability to apply it under stress, ensuring the healthcare professional is capable of handling emergency medical situations effectively.
Essential Concepts for Advanced Life Support Certification
In order to excel in advanced life support certification, it is essential to grasp the foundational concepts that guide emergency response and patient stabilization. These principles serve as the backbone of any life-saving procedure, ensuring healthcare professionals are equipped to make rapid, informed decisions during high-pressure situations. A strong understanding of these core topics is crucial for both theoretical and practical assessment success.
Here are some of the most critical concepts to focus on:
| Concept | Description |
|---|---|
| Cardiac Rhythm Recognition | Recognizing various cardiac arrhythmias and understanding the appropriate interventions for each. |
| Airway Management | Techniques to secure and maintain a clear airway during respiratory distress or failure. |
| Defibrillation Protocols | Using electrical shock devices effectively to restore normal heart rhythm in emergencies. |
| Medications and Dosages | Knowing which medications to administer and at what dosages for different emergency situations. |
| Team Communication | Coordinating with other healthcare providers during emergencies to ensure efficient care delivery. |
Focusing on these key concepts will help candidates prepare effectively for certification, ensuring they can perform competently in real-world medical emergencies where every second counts.
How to Approach Advanced Life Support Scenarios
In high-pressure medical situations, the ability to approach and manage critical scenarios effectively is key to patient survival. Whether responding to a cardiac emergency or handling respiratory failure, knowing how to apply the right protocols swiftly and correctly can make all the difference. This section outlines the essential steps to take when faced with emergency situations that require immediate intervention.
The following table outlines a structured approach to handling various critical situations:
| Scenario | Key Steps |
|---|---|
| Cardiac Arrest | Immediately assess the patient’s responsiveness, initiate chest compressions, and prepare for defibrillation or medication administration as required. |
| Airway Obstruction | Assess the airway, clear obstructions using the appropriate technique, and ensure the patient is breathing adequately before proceeding with ventilation if needed. |
| Severe Bradycardia | Identify the cause, administer atropine or prepare for pacing, and monitor the patient’s response to interventions. |
| Respiratory Failure | Ensure oxygenation through intubation or non-invasive methods, and provide ventilation support to stabilize the patient. |
Each scenario requires a systematic approach, combining knowledge, skill, and quick decision-making. Practice in simulated environments will enhance confidence and efficiency, helping healthcare professionals handle real-life situations with calm and precision.
Critical Protocols You Must Know
When dealing with life-threatening medical situations, understanding and applying the correct protocols is essential for saving lives. These guidelines provide healthcare professionals with the necessary steps to take during emergencies, ensuring timely and effective interventions. Mastering these protocols not only improves patient outcomes but also enhances the overall response to critical events.
The following are the most important protocols to familiarize yourself with:
- Cardiac Arrest Management: Involves early recognition, initiation of high-quality chest compressions, and timely defibrillation when indicated. Immediate action is key to survival.
- Advanced Airway Management: Securing the airway and ensuring adequate ventilation, whether through intubation or advanced non-invasive techniques, is critical in respiratory emergencies.
- Arrhythmia Management: Understanding the proper intervention for abnormal heart rhythms, including medication administration and electrical therapies like pacing or defibrillation, is vital.
- Pharmacology Guidelines: Knowing which medications to administer, their dosages, and timing is crucial in managing cardiovascular, respiratory, and other critical conditions.
- Post-Cardiac Arrest Care: Ensuring optimal care after the return of spontaneous circulation to improve patient outcomes and reduce neurological damage.
Being well-versed in these protocols is essential for healthcare providers who must act swiftly and decisively in emergencies. Practice, review, and a solid understanding of these guidelines will prepare you for handling any critical situation efficiently.
Common Mistakes in Advanced Life Support Testing
During the certification process for advanced life-saving techniques, it is easy to make errors that can negatively impact both performance and results. Many of these mistakes stem from not adhering strictly to protocols or failing to maintain focus under pressure. Recognizing and avoiding these common pitfalls can help ensure a more successful outcome when completing the assessment.
Below are some of the most frequent mistakes made during testing:
- Delayed Recognition of Cardiac Arrest: Failing to immediately recognize the signs of cardiac arrest and delay in starting chest compressions can significantly impact patient survival chances.
- Incorrect Medication Administration: Administering the wrong drug or incorrect dosage due to confusion or lack of familiarity with protocols can lead to ineffective treatment.
- Improper Airway Management: Neglecting to secure the airway properly or failing to assess the need for advanced airway interventions can lead to respiratory failure.
- Inadequate Chest Compressions: Not performing chest compressions at the correct depth or rate, or pausing too long between compressions, reduces their effectiveness.
- Failure to Follow Rhythm Protocols: Not recognizing the correct rhythm or applying the wrong defibrillation protocol can hinder patient stabilization during arrhythmic events.
Avoiding these mistakes requires thorough preparation, practice, and focus. By reviewing protocols and honing practical skills, healthcare professionals can ensure they are ready to perform competently under test conditions and in real-life emergencies.
Advanced Life Support Certification Preparation Tips
Preparing for advanced life support certification involves more than just memorizing protocols. It requires a deep understanding of life-saving techniques and the ability to apply them under pressure. Effective preparation can boost your confidence and improve your performance when it matters most. Focused study, practice, and a strategic approach are essential for mastering the required skills and knowledge.
Here are some preparation tips to help you succeed:
| Preparation Tip | Description |
|---|---|
| Study the Guidelines Thoroughly | Ensure you have a strong understanding of all protocols and treatment algorithms. Familiarity with the most recent guidelines is critical. |
| Practice Mock Scenarios | Simulate emergency situations to get used to applying your knowledge in real-time. Practice both individually and as part of a team. |
| Review Medication Dosages | Know the correct drugs and dosages for different emergencies. Understanding pharmacology is vital for effective patient management. |
| Focus on Key Skills | Concentrate on hands-on skills like chest compressions, airway management, and defibrillation. Mastering these basics is essential. |
| Stay Calm Under Pressure | Develop strategies to stay composed during high-stress situations. Calmness and clear thinking are crucial for success. |
By following these tips and dedicating time to practice, you’ll be better prepared to handle the challenges of certification and real-life emergencies effectively.
Mastering Cardiac Arrest Algorithms
Effective management of cardiac arrest relies heavily on a clear, step-by-step approach. These treatment algorithms provide the structured response needed during such high-stakes emergencies. A deep understanding of these protocols and the ability to apply them quickly and accurately can greatly enhance patient survival rates. Familiarity with the correct sequence of actions, including chest compressions, defibrillation, and medication administration, is crucial to ensure the best possible outcome.
Key Steps in Cardiac Arrest Algorithms
The following are the essential steps to follow during a cardiac arrest situation:
- Immediate Recognition: Quickly assess the patient to confirm cardiac arrest and initiate chest compressions.
- High-Quality Chest Compressions: Perform compressions at the correct rate and depth, ensuring minimal interruptions.
- Defibrillation: Apply defibrillation as soon as possible if indicated, using an automated external defibrillator (AED) or manual defibrillator.
- Advanced Airway Management: Secure the airway and provide adequate ventilation, if necessary, to support breathing.
- Medication Administration: Administer appropriate drugs such as epinephrine, amiodarone, or lidocaine based on the rhythm and clinical status.
Practicing the Algorithm
Regular practice and simulated scenarios are vital to mastering these life-saving algorithms. During practice sessions, focus on speed, accuracy, and teamwork to ensure a coordinated and effective response. Regular review of the protocols helps to reinforce the sequence of actions and builds muscle memory, ensuring that you can respond instinctively when every second counts.
By committing these steps to memory and practicing frequently, healthcare professionals can confidently manage cardiac arrest situations with greater efficiency and better outcomes for patients.
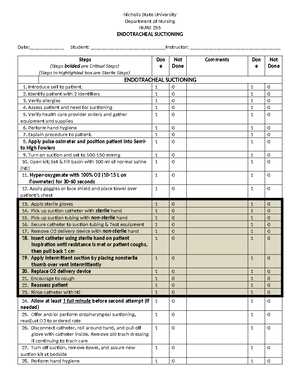
Reviewing Advanced Airway Management
Airway management is a critical skill in emergency medicine, particularly when a patient is unable to maintain their own airway. Proper techniques ensure that oxygen is delivered effectively to vital organs, preventing brain injury and other complications. Advanced airway management involves the use of specialized tools and methods to secure the airway in patients experiencing respiratory failure, obstruction, or arrest. Mastery of these techniques is essential for healthcare providers in critical care settings.
Key Techniques in Advanced Airway Management
There are several methods and devices that healthcare professionals use to secure a patient’s airway during emergencies:
- Endotracheal Intubation: A tube is inserted into the trachea to maintain an open airway and ensure proper ventilation. This method requires skill and accuracy to avoid complications like esophageal intubation.
- Supraglottic Airway Devices: These devices, such as the laryngeal mask airway (LMA), are inserted into the throat to provide a clear passage for airflow, particularly when intubation is difficult.
- Bag-Valve Mask (BVM) Ventilation: A manual method used to provide positive pressure ventilation to patients who are not breathing or have inadequate respiration. Proper seal and technique are vital for effective use.
- Cricoid Pressure: Applied to prevent regurgitation during intubation, cricoid pressure helps reduce the risk of aspiration, particularly in unconscious patients.
Best Practices and Considerations
When performing advanced airway management, it is crucial to follow established protocols to ensure the patient’s safety and improve outcomes. Here are some best practices:
- Assess the Patient’s Condition: Quickly determine the patient’s airway status and identify if advanced intervention is necessary. Always evaluate the risks and benefits of each approach.
- Minimize Interruptions: Avoid long delays when securing the airway. The quicker the intervention, the better the patient outcome, particularly in cases of respiratory distress.
- Monitor and Confirm Placement: After airway placement, confirm its proper position using clinical signs, capnography, or auscultation to ensure the device is functioning as intended.
- Practice Team Communication: Clear communication among team members during airway management is crucial for success, especially when using advanced techniques in high-pressure situations.
By mastering these advanced airway management techniques and consistently practicing, healthcare providers can ensure they are prepared to respond to respiratory emergencies with confidence and expertise.
Pharmacology in Advanced Life Support
Pharmacology plays a vital role in the management of critical conditions, particularly during cardiac arrest and other life-threatening emergencies. The appropriate use of medications can significantly influence patient outcomes by stabilizing heart rhythms, improving circulation, and preventing further complications. Understanding the pharmacological agents commonly used in advanced life support protocols is essential for healthcare professionals to ensure effective and timely treatment during emergencies.
Several classes of drugs are frequently used in critical care situations. These medications help manage arrhythmias, improve blood flow, and support the body’s vital functions. Healthcare providers must not only know the indications and dosages for these drugs but also their potential side effects, interactions, and timing in relation to other interventions.
Commonly used medications include vasopressors, antiarrhythmic agents, and sedation drugs. Each of these plays a unique role in maintaining or restoring normal physiological functions during acute events. Understanding their mechanism of action, proper administration routes, and contraindications is essential for providing optimal care in emergencies.
Test Questions on Arrhythmias
Understanding arrhythmias is crucial in managing critical cardiac conditions. These abnormal heart rhythms can significantly affect a patient’s circulation and oxygen delivery, making rapid diagnosis and treatment essential. In clinical scenarios, healthcare professionals must be able to identify different types of arrhythmias, understand their potential causes, and apply the appropriate treatment strategies. Below are key questions that can help reinforce knowledge and guide decision-making in managing arrhythmias.
Key Questions for Diagnosing Arrhythmias
These questions are designed to assess the ability to recognize and manage various arrhythmias:
- What are the characteristics of a normal sinus rhythm?
- How would you differentiate between atrial fibrillation and atrial flutter?
- What is the first-line treatment for ventricular tachycardia with a pulse?
- What pharmacological agents are used to manage supraventricular tachycardia (SVT)?
- When is defibrillation indicated in cases of ventricular fibrillation?
Understanding Treatment Approaches
After identifying the arrhythmia, it’s essential to understand the correct treatment protocols. The following questions focus on appropriate interventions for various arrhythmic conditions:
- What is the role of amiodarone in the treatment of life-threatening arrhythmias?
- How does synchronized cardioversion differ from defibrillation in the treatment of arrhythmias?
- What are the indications for using adenosine in managing paroxysmal supraventricular tachycardia (PSVT)?
- What are the signs that a patient with a bradycardic arrhythmia may require a pacemaker?
By reviewing these critical questions, healthcare providers can ensure they are prepared to identify, treat, and manage arrhythmias in a variety of clinical settings. Mastery of this knowledge is key to delivering optimal care in emergency and critical care environments.
Effective BLS Integration in Advanced Life Support
Basic life support (BLS) plays a foundational role in the management of patients experiencing cardiac arrest or other critical emergencies. The integration of BLS principles with advanced interventions is crucial for improving patient outcomes. While advanced life-saving techniques are vital, they work most effectively when combined with high-quality basic care, such as chest compressions, airway management, and early defibrillation. This section will explore the importance of seamless integration between these two levels of care to optimize survival rates.
Key Components of BLS in Critical Care
Before advanced measures can be initiated, it is essential to begin with the basics. The first moments of an emergency situation often determine the success of the intervention. The following BLS techniques are critical to supporting the patient during the initial phase:
- Chest Compressions: High-quality, uninterrupted chest compressions are fundamental in maintaining circulation to vital organs, particularly the brain and heart.
- Airway Management: Proper airway positioning and securing are essential to ensure adequate oxygenation during the early stages of resuscitation.
- Early Defibrillation: Defibrillation, when indicated, should be performed as soon as possible to restore normal heart rhythm in cases of shockable rhythms like ventricular fibrillation.
Bridging the Gap Between BLS and Advanced Care
As the resuscitation team transitions from basic to advanced care, it is vital that BLS efforts continue until more advanced interventions are available. For example, while medications and advanced airway devices are being utilized, ongoing chest compressions must be maintained to ensure sufficient perfusion. Coordination between team members is critical to make this transition smooth and effective. The key to success lies in balancing both BLS and advanced techniques, ensuring that no step in the process is neglected.
Integrating high-quality BLS into advanced care protocols is not just a matter of performing individual tasks; it requires a cohesive approach where both sets of interventions support each other. This collaboration improves the chances of a favorable patient outcome during the most critical moments of care.
Effective BLS Integration in Advanced Life Support
Basic life support (BLS) plays a foundational role in the management of patients experiencing cardiac arrest or other critical emergencies. The integration of BLS principles with advanced interventions is crucial for improving patient outcomes. While advanced life-saving techniques are vital, they work most effectively when combined with high-quality basic care, such as chest compressions, airway management, and early defibrillation. This section will explore the importance of seamless integration between these two levels of care to optimize survival rates.
Key Components of BLS in Critical Care
Before advanced measures can be initiated, it is essential to begin with the basics. The first moments of an emergency situation often determine the success of the intervention. The following BLS techniques are critical to supporting the patient during the initial phase:
- Chest Compressions: High-quality, uninterrupted chest compressions are fundamental in maintaining circulation to vital organs, particularly the brain and heart.
- Airway Management: Proper airway positioning and securing are essential to ensure adequate oxygenation during the early stages of resuscitation.
- Early Defibrillation: Defibrillation, when indicated, should be performed as soon as possible to restore normal heart rhythm in cases of shockable rhythms like ventricular fibrillation.
Bridging the Gap Between BLS and Advanced Care
As the resuscitation team transitions from basic to advanced care, it is vital that BLS efforts continue until more advanced interventions are available. For example, while medications and advanced airway devices are being utilized, ongoing chest compressions must be maintained to ensure sufficient perfusion. Coordination between team members is critical to make this transition smooth and effective. The key to success lies in balancing both BLS and advanced techniques, ensuring that no step in the process is neglected.
Integrating high-quality BLS into advanced care protocols is not just a matter of performing individual tasks; it requires a cohesive approach where both sets of interventions support each other. This collaboration improves the chances of a favorable patient outcome during the most critical moments of care.
Key Differences in 2016 Advanced Life Support Guidelines
Understanding the changes in the guidelines for advanced life support is crucial for staying up-to-date with the latest protocols and best practices. In 2016, several important revisions were introduced to enhance the effectiveness of life-saving interventions. These updates reflect the ongoing research and real-world experience in critical care, focusing on improving patient outcomes during emergency situations. This section highlights the key differences in the guidelines that were implemented to align with these advancements in medical care.
New Protocols for Cardiac Arrest Management
One of the most notable changes in 2016 was the update to cardiac arrest management protocols. The emphasis shifted toward enhancing the quality of chest compressions and minimizing interruptions during resuscitation efforts. Key updates included:
- Continuous Chest Compressions: The new guidelines stress the importance of continuous high-quality chest compressions with minimal pauses, aimed at maintaining blood circulation to vital organs.
- Use of Capnography: The 2016 guidelines recommend capnography for confirming effective chest compressions and monitoring endotracheal tube placement, as well as detecting return of spontaneous circulation (ROSC).
- Enhanced Post-Resuscitation Care: The guidelines now place more focus on post-resuscitation care, including the use of targeted temperature management (TTM) to improve outcomes after return of spontaneous circulation.
Updates in Drug Administration and Dosage
Another area of change in the 2016 guidelines was the approach to medication administration. The revised protocols provided more specific recommendations for drug usage during life-threatening situations. Some key updates included:
- Medication Dosage Clarification: The new guidelines clarified dosages for commonly used medications like epinephrine and amiodarone, with an emphasis on administration timing and frequency.
- Use of Vasopressors: The guidelines now offer clearer instructions on the use of vasopressors in cardiac arrest scenarios, with updated recommendations for their role in improving perfusion and blood pressure.
- Role of Antiarrhythmic Drugs: The role of antiarrhythmic medications has been better defined, especially in cases of shockable rhythms, with revised recommendations for their optimal use in resuscitation efforts.
These adjustments ensure that life-saving interventions are as effective as possible, reflecting the latest scientific evidence and clinical practices. By staying current with the revised protocols, healthcare providers can enhance their ability to provide effective and timely care in critical situations.
Certification Renewal Insights
Maintaining certification in advanced life support is essential for healthcare providers who need to stay current with life-saving techniques. The process of certification renewal is designed to ensure that professionals are equipped with the latest skills and knowledge necessary to provide the highest standard of care in emergencies. This section offers an overview of key considerations and steps involved in renewing your certification.
Why Certification Renewal is Important
Renewing your certification ensures that your skills are up-to-date and that you are familiar with the latest guidelines and protocols in emergency care. It helps to:
- Ensure Competency: Regular renewal helps maintain proficiency in critical life-saving skills, improving patient outcomes.
- Stay Updated: With frequent updates to treatment protocols, staying certified ensures you are always working with the most current methods.
- Meet Job Requirements: Many healthcare institutions require certification renewal at specific intervals to remain compliant with regulatory standards.
Steps to Renew Your Certification
Renewal typically involves several straightforward steps. Here’s a breakdown of the process:
- Review Current Guidelines: Before beginning the renewal process, it’s important to review the latest protocols and updates in your field. These might include changes in drug dosages, compression techniques, and other key interventions.
- Complete Required Training: Some programs may require you to take a refresher course or participate in hands-on skills practice to demonstrate your proficiency.
- Pass the Renewal Course: In many cases, you will need to pass a written or practical test that assesses your knowledge and ability to apply life-saving techniques in simulated scenarios.
- Submit Your Application: Once you have successfully completed the required training and assessments, submit your renewal application to the certifying body.
Common Mistakes to Avoid

While the renewal process is straightforward, many individuals make common mistakes that can delay certification. Here are some tips to avoid them:
- Procrastinating: Don’t wait until the last minute to renew your certification. Many programs require advanced registration, and waiting too long can lead to scheduling issues.
- Forgetting to Update Contact Information: Ensure that your contact details are up-to-date with the certifying body to receive timely notifications and reminders.
- Missing the Deadline: Failing to renew before your certification expires can result in a lapse in your credentials, requiring additional steps to regain certification.
By understanding the renewal process and preparing in advance, you can ensure your skills remain sharp and your credentials stay current, allowing you to continue providing top-quality emergency care when it’s needed most.
Real-life Case Studies for Practice
Studying real-life case scenarios provides invaluable experience for healthcare professionals looking to enhance their decision-making and critical thinking skills in emergency situations. These case studies help simulate the complexities of real-world medical crises, offering an opportunity to practice the application of knowledge and techniques in a controlled environment. By analyzing and reflecting on these cases, providers can sharpen their ability to act quickly and efficiently when lives are at risk.
Case Study 1: Cardiac Arrest in the ER
A 58-year-old male arrives in the emergency room after collapsing at home. Upon arrival, he is unresponsive, and vital signs indicate severe distress. The healthcare team immediately initiates life-saving measures. Key decisions must be made quickly, including:
- Assessment: Determining the cause of the collapse, evaluating the need for CPR, and confirming the patient’s cardiac rhythm.
- Interventions: Deciding on the appropriate use of defibrillation, medications, and advanced airway management.
- Team Coordination: Effectively communicating and coordinating with team members to ensure timely interventions and optimal outcomes.
Analyzing this case teaches how to prioritize interventions based on patient presentation and available resources, as well as how to manage high-pressure situations efficiently.
Case Study 2: Severe Respiratory Distress in a Pediatric Patient
A 4-year-old child is brought into the hospital with signs of severe respiratory distress. The child’s condition is deteriorating rapidly, and the healthcare team must quickly evaluate and intervene. In this case, critical decisions include:
- Initial Evaluation: Determining the underlying cause of the respiratory distress (e.g., asthma exacerbation, foreign body aspiration).
- Intervention Choices: Deciding on the administration of oxygen, bronchodilators, and possibly advanced airway management techniques.
- Family Communication: Keeping the family informed about the child’s condition and potential treatment options.
This case provides valuable practice in managing pediatric emergencies, requiring not only clinical expertise but also compassion and effective communication with worried families.
By examining these real-world scenarios, healthcare professionals gain deeper insight into the fast-paced and high-stakes nature of emergency care. These case studies help to reinforce the principles of effective diagnosis, teamwork, and timely decision-making, all of which are crucial for optimal patient outcomes.
Post-Exam Steps and Results
After completing the assessment, understanding the subsequent steps is crucial for determining progress and ensuring that all requirements are met for certification. The post-assessment process involves reviewing your performance, receiving results, and taking necessary actions based on your outcomes. It’s important to know how to interpret your results and what to do next to either proceed with certification or retake the assessment if needed.
Steps After Completing the Assessment
Once you have finished the assessment, there are a few key steps to follow:
- Immediate Results: Some assessments provide instant feedback, allowing you to view your performance as soon as you finish. This can be a helpful way to gauge your understanding of the material.
- Review Process: Many institutions or organizations will manually review your answers to ensure accuracy and proper assessment of skills. This step may take longer, depending on the institution’s process.
- Receiving Certification: Upon successful completion, certification will be issued. It often includes a physical certificate and access to an online record of your achievement.
Understanding the Results
Interpreting your results is an essential part of the process. You will typically receive a score or feedback that indicates your performance across different areas. Understanding what the results mean is critical for your next steps:
| Score Range | Action Required |
|---|---|
| Pass | Proceed to certification and receive your credentials. |
| Fail | Review the areas where you need improvement, and plan to retake the assessment after additional study. |
| Conditional Pass | Complete additional requirements or remediation before receiving full certification. |
If you pass, congratulations! You can now move forward with your professional development. If not, the feedback will guide you in focusing your preparation for a future attempt. Continuous improvement is a key part of professional practice, and understanding your results is the first step towards mastering the skills required for certification.