When preparing for assessments in the field of end-of-life support, it is crucial to focus on the various principles, techniques, and ethical considerations involved in this specialized area. The process involves understanding the complex needs of individuals facing serious illnesses and providing holistic solutions that address both physical and emotional challenges.
In this section, we will explore essential topics that often appear in evaluations for professionals working in this area. From pain management strategies to effective communication with families, each topic plays a significant role in shaping the quality of assistance provided to patients. Mastery of these subjects will not only enhance your knowledge but also ensure a deeper understanding of how to meet the diverse needs of those in critical health situations.
Comprehensive preparation involves reviewing common case scenarios, ethical dilemmas, and the latest approaches to improving the overall well-being of patients. It is important to recognize that each situation requires a tailored response, guided by empathy, medical expertise, and a thorough understanding of available support tools.
Palliative Care Exam Questions and Answers
In this section, we delve into essential topics commonly tested in assessments related to end-of-life support. Understanding these areas is vital for professionals working with individuals facing terminal conditions, as they help ensure high-quality, compassionate assistance in difficult circumstances. The ability to respond effectively to various scenarios requires both theoretical knowledge and practical application of supportive techniques.
Key themes often covered include pain management, ethical considerations, emotional support for patients and families, and the role of healthcare teams. Mastery of these subjects enables professionals to address the physical, psychological, and social needs of those in critical health stages, fostering a holistic approach to treatment and comfort. Preparing thoroughly for these assessments equips individuals with the confidence to navigate complex challenges in this field.
Familiarity with case studies and practical examples enhances your readiness for real-world situations. By reviewing common scenarios, individuals can develop the necessary problem-solving skills to make informed decisions under pressure, improving patient outcomes and family support during challenging times.
Understanding Palliative Care Principles
At the heart of providing support to individuals facing serious illness lies a set of core principles that guide professionals in delivering compassionate, holistic assistance. These principles emphasize the importance of treating the whole person, not just addressing the medical symptoms but also focusing on emotional, social, and psychological well-being. It is essential to ensure that each patient is seen in their unique context, where dignity, comfort, and respect are paramount.
These fundamental concepts play a crucial role in shaping how healthcare providers interact with patients and families. They serve as a framework for building trust, enhancing communication, and making informed decisions that align with the patient’s values and needs. Below is a table summarizing the key principles that form the foundation of effective support in this field:
| Principle | Description |
|---|---|
| Holistic Approach | Addressing the physical, emotional, social, and spiritual needs of the individual. |
| Dignity | Ensuring that the patient feels valued and respected throughout their journey. |
| Patient-Centered Care | Involving patients in decisions about their own treatment, ensuring their preferences are considered. |
| Symptom Management | Focusing on relieving pain, discomfort, and other symptoms to improve the patient’s quality of life. |
| Communication | Maintaining open, honest, and empathetic communication with both patients and families. |
| Support for Families | Providing emotional, social, and practical support to families during difficult times. |
By integrating these guiding principles, professionals can ensure that their approach is not only medically effective but also compassionate, fostering an environment of trust and comfort for those in need of assistance.
Common Palliative Care Exam Topics
In any assessment focused on end-of-life support, there are several critical areas that consistently appear. These topics are essential for understanding the complexities involved in providing holistic assistance to individuals facing serious health conditions. Mastering these subjects helps ensure professionals can effectively respond to the challenges that arise in various clinical and emotional contexts.
Symptom management is one of the primary subjects, focusing on techniques for relieving pain, nausea, breathlessness, and other discomforts. Equally important is patient-centered communication, which emphasizes the need for clear, empathetic, and honest dialogue with patients and families. Another common area of focus is the ethical considerations related to life-ending decisions, such as advance directives and the role of family members in decision-making.
Understanding the role of healthcare teams is also frequently tested, as collaboration among doctors, nurses, social workers, and chaplains is essential to delivering comprehensive support. Additionally, cultural competency plays a significant role in ensuring that diverse patient needs are met with sensitivity and respect. Finally, emotional and psychological support for both patients and their families is critical in navigating the emotional challenges of terminal illness.
Key Concepts in Symptom Management
Effective management of symptoms is a fundamental aspect of supporting individuals with serious illnesses. This process involves addressing a variety of physical and emotional discomforts that can significantly impact a patient’s quality of life. Understanding the most common symptoms, as well as the best approaches to relieve them, is essential for ensuring that patients remain as comfortable as possible throughout their journey.
Pain relief is perhaps the most widely recognized aspect of symptom management. Strategies for reducing pain include both pharmacological and non-pharmacological methods, ranging from medications to alternative therapies like massage or relaxation techniques. Similarly, breathlessness and difficulty breathing are frequent concerns that require specialized approaches to ease discomfort and improve breathing patterns, such as the use of supplemental oxygen or positioning techniques.
Additionally, nausea and vomiting are common symptoms that must be addressed with careful medication management, dietary changes, and other supportive interventions. Another crucial area is emotional distress, as anxiety, depression, and fear can exacerbate physical symptoms and should be managed through counseling, medications, or spiritual support. A thorough understanding of these key concepts enables healthcare providers to implement tailored interventions that address the unique needs of each patient.
Approaches to Pain Relief in Palliative Care
Managing pain effectively is a central aspect of supporting individuals facing serious health challenges. Adequate pain relief can significantly improve a patient’s quality of life, helping them remain more comfortable and engaged with their surroundings. Different strategies and techniques are employed to address pain, ranging from medication to complementary therapies, depending on the intensity and type of discomfort experienced.
Pharmacological Interventions
The most common method of pain management involves the use of medications. These can range from over-the-counter analgesics to more advanced options such as opioids. The choice of medication is influenced by factors such as the severity of the pain, the patient’s medical history, and their response to previous treatments. It is essential to tailor these treatments to the individual, starting with lower doses and gradually increasing if necessary, to minimize side effects while achieving optimal pain relief.
Non-Pharmacological Approaches
In addition to medications, non-pharmacological techniques are often employed to alleviate pain. These may include physical therapies like massage, acupuncture, or heat and cold applications. Psychological strategies such as relaxation techniques, guided imagery, and cognitive behavioral therapy (CBT) also play a key role in helping patients manage pain. These complementary approaches can be particularly effective when combined with medical treatments, addressing both the physical and emotional components of pain.
Palliative Care for End-of-Life Patients
Providing appropriate support for individuals nearing the end of life requires a compassionate, comprehensive approach that focuses on comfort, dignity, and quality of life. The aim is not to cure, but to manage symptoms effectively and ensure that patients experience as little discomfort as possible during their final stages. This type of support involves addressing both physical and emotional needs while respecting the wishes of the patient and their loved ones.
One of the main objectives is to relieve pain and other distressing symptoms, such as nausea, shortness of breath, and fatigue. In addition to managing physical discomfort, it is equally important to provide emotional and psychological support. This may include helping patients come to terms with their condition, offering counseling services, and facilitating conversations between the patient and their family members about end-of-life decisions. Involving the patient in decisions about their treatment options is a key element of this process, ensuring that their preferences are honored and that they feel in control during a challenging time.
Ethical Dilemmas in Palliative Care
End-of-life support often involves complex ethical decisions that require careful consideration of both medical principles and the patient’s personal values. These dilemmas can arise when determining the best course of action, especially when treatment options conflict with the patient’s wishes or when the line between prolonging life and ensuring comfort becomes unclear. The decisions made in these situations can have a profound impact on the patient, their family, and the healthcare team.
Respecting Patient Autonomy
One of the most critical ethical principles in this context is respecting the autonomy of the patient. This involves honoring their right to make decisions about their own treatment, including the decision to refuse or discontinue life-sustaining interventions. However, challenges can arise when patients may not be able to communicate their wishes clearly, or when family members or medical staff have differing opinions on what is in the patient’s best interest. In such cases, it is important to involve a multidisciplinary team and consider legal and ethical frameworks to ensure that the patient’s autonomy is respected.
Balancing Beneficence and Non-Maleficence
Another key issue is balancing beneficence (doing what is best for the patient) with non-maleficence (avoiding harm). Healthcare providers may struggle with whether to continue aggressive treatments that could prolong life, even if the patient is experiencing significant suffering, or whether to shift focus entirely to comfort measures. These decisions are often difficult because they involve weighing the potential benefits of further medical interventions against the risk of increasing discomfort or reducing the quality of life. Ethical guidelines, along with open communication with the patient and their family, can help guide these difficult decisions.
Communication Skills in End-of-Life Care
Effective communication is essential when supporting individuals in their final stages of life. It plays a critical role in ensuring that patients’ needs and preferences are understood and respected. Skilled communication fosters trust, reduces anxiety, and helps both patients and their families navigate challenging decisions. Healthcare professionals must be prepared to engage in sensitive conversations, addressing not only the physical aspects of the illness but also the emotional, psychological, and spiritual concerns that may arise.
Key communication skills that are essential for professionals working with individuals nearing the end of life include:
- Active Listening: Paying close attention to what the patient and family members are saying, and offering empathetic responses that demonstrate understanding.
- Clarity and Transparency: Communicating complex information in simple, clear terms, while ensuring that patients and families understand the options available to them.
- Emotional Support: Acknowledging and validating the feelings of patients and their families, providing reassurance during difficult moments.
- Respect for Patient Autonomy: Encouraging patients to share their thoughts, desires, and decisions regarding their treatment and end-of-life wishes.
- Cultural Sensitivity: Being aware of cultural differences and how these may influence communication styles and decision-making processes.
In addition, healthcare professionals should be prepared to navigate challenging conversations around sensitive topics such as prognosis, life-sustaining treatments, and end-of-life planning. These discussions should be conducted with compassion, patience, and respect, always aiming to support the patient’s values and preferences. Effective communication not only enhances the experience for the patient but also provides vital support for family members during a challenging and emotional time.
Assessing Quality of Life in Patients
Measuring the overall well-being of individuals facing serious health conditions is an essential part of managing their treatment and support. The process of evaluating how an illness affects a patient’s physical, emotional, and social life provides crucial insights into their needs and preferences. This assessment is not only about tracking symptoms but also understanding how the patient perceives their life, their satisfaction with the support they receive, and their ability to maintain a sense of dignity and purpose.
Holistic Approach to Assessment
Assessing quality of life involves a holistic view, taking into account various factors that influence a patient’s experience. This includes evaluating their physical comfort, emotional state, ability to perform daily activities, and social interactions. A comprehensive evaluation can identify areas where support can be improved, ensuring that the treatment plan aligns with the patient’s values and wishes. Physical symptoms such as pain, fatigue, and difficulty breathing are often central to the assessment, but emotional well-being and social engagement are equally important in understanding a person’s overall quality of life.
Tools for Evaluation
Several tools are used to assess quality of life, ranging from standardized questionnaires to informal discussions. These instruments allow healthcare providers to gather detailed feedback from patients and their families, capturing the impact of the illness on various aspects of life. Some commonly used tools include quality of life scales that measure factors such as pain levels, emotional well-being, and social functioning. These tools help tailor interventions to meet the specific needs of the patient, ensuring that their comfort and emotional support are prioritized as part of their overall treatment plan.
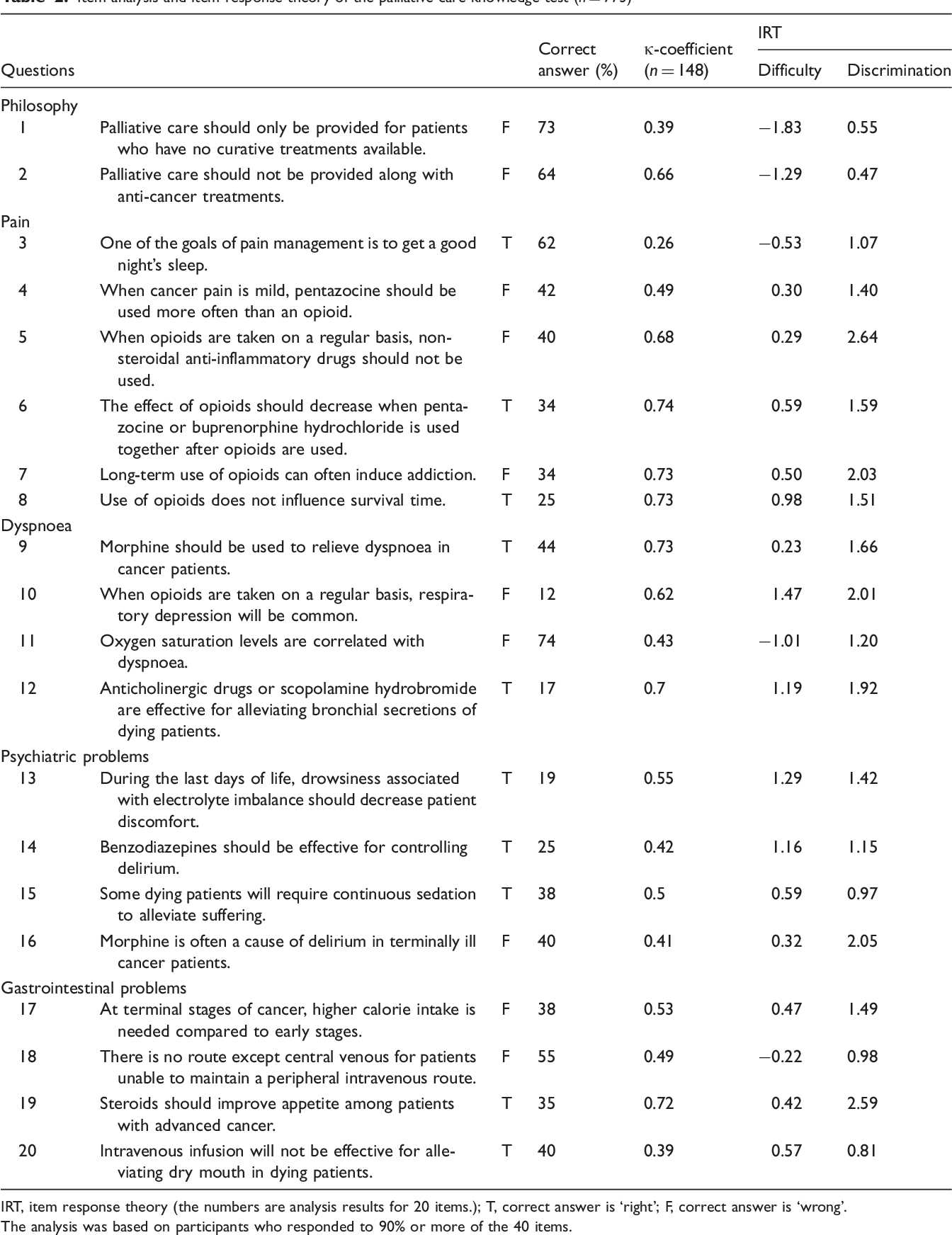
Pharmacological Interventions in Palliative Care
Medications play a critical role in managing the symptoms and improving the quality of life for individuals with serious illnesses. These treatments aim to reduce suffering, control pain, and address other distressing symptoms such as nausea, anxiety, or difficulty breathing. Pharmacological interventions are often tailored to the specific needs of the patient, taking into account the severity of symptoms, the underlying condition, and the patient’s overall prognosis. The goal is to provide relief while minimizing side effects and improving the patient’s comfort during the later stages of life.
Commonly Used Medications
The following table highlights some of the most commonly used medications in symptom management for individuals facing serious illness:
| Medication | Purpose | Common Side Effects |
|---|---|---|
| Opioids | Pain relief, particularly for severe pain | Constipation, sedation, nausea |
| Antidepressants | Managing depression and anxiety | Dry mouth, drowsiness, weight gain |
| Antiemetics | Relieving nausea and vomiting | Drowsiness, dizziness, constipation |
| Benzodiazepines | Reducing anxiety and promoting relaxation | Drowsiness, confusion, memory issues |
| Corticosteroids | Reducing inflammation and improving appetite | Weight gain, insomnia, fluid retention |
Tailoring Treatment to Individual Needs
Each patient’s response to medication can vary, so it is important for healthcare providers to closely monitor the effectiveness and adjust dosages accordingly. By regularly reassessing symptom relief and side effects, adjustments can be made to ensure that the patient’s comfort is maximized. Personalized treatment plans that incorporate both pharmacological and non-pharmacological interventions help address the unique needs of each individual. The focus remains on improving the patient’s overall well-being and dignity during this challenging time.
Psychosocial Support for Patients and Families
Providing emotional and psychological assistance is vital for individuals facing serious health challenges and their families. This support addresses not only the mental well-being of the patient but also helps families cope with stress, uncertainty, and the emotional burden of caregiving. Offering psychosocial support fosters resilience, strengthens coping mechanisms, and promotes a sense of hope and control in a difficult situation. It is important to ensure that patients and their loved ones feel heard, understood, and respected throughout the entire process.
Key Areas of Psychosocial Support
Support can be provided in various forms, targeting different emotional, social, and spiritual aspects of a person’s experience. The following areas are particularly important when providing comprehensive psychosocial support:
- Emotional Support: Helping patients and families process feelings of sadness, fear, or anxiety through active listening and validation of their emotions.
- Spiritual Care: Addressing existential questions, offering comfort in faith-based practices, or exploring personal beliefs to help patients and families find meaning in challenging times.
- Social Connections: Encouraging interactions with loved ones, ensuring that patients remain connected to their social networks and community.
- Grief Counseling: Assisting families in managing anticipatory grief and preparing for the eventual loss of a loved one.
- Information and Guidance: Providing clear information about the illness, treatment options, and available support services to empower patients and families in making informed decisions.
Approaches to Providing Support
There are several methods through which healthcare professionals can offer psychosocial assistance. These approaches are designed to cater to the emotional and practical needs of patients and their families:
- Individual Counseling: One-on-one sessions to help patients or family members process their emotions and develop coping strategies.
- Support Groups: Group settings where individuals with similar experiences can share, provide mutual support, and reduce feelings of isolation.
- Family Therapy: Facilitating communication among family members to address collective emotional challenges and foster a unified approach to caregiving.
- Respite Services: Offering temporary relief to family caregivers, giving them a break from caregiving responsibilities to reduce burnout.
By addressing the psychosocial needs of both patients and families, healthcare providers help alleviate some of the emotional and mental burdens associated with life-limiting illnesses. This support ensures that individuals maintain dignity, comfort, and quality of life, both in their remaining time and throughout the caregiving process.
Managing Family Dynamics in Palliative Care
When individuals face life-limiting illnesses, the family becomes an essential part of the care team. Navigating family relationships during this time can be complex, as emotions, expectations, and roles evolve rapidly. Each family member may have different coping mechanisms, communication styles, and beliefs about treatment, all of which can influence how they interact with the patient and with each other. Effective management of these dynamics is crucial to ensuring that the patient’s needs are met while maintaining family cohesion and well-being.
Challenges in Family Dynamics
Managing family dynamics requires understanding and addressing the unique challenges each family faces. Some common issues include:
- Conflicting Roles: Family members may struggle with balancing caregiving responsibilities, emotional support, and decision-making roles.
- Communication Barriers: Misunderstandings or lack of open communication can lead to frustration, misinterpretation of intentions, and increased tension.
- Family Conflict: Differing views on the patient’s treatment or care plan may cause disagreements among family members, leading to division and emotional stress.
- Anticipatory Grief: Family members may experience sorrow before the actual loss, which can affect their ability to support the patient or each other effectively.
Strategies for Managing Family Dynamics
There are several strategies healthcare professionals can use to help manage family relationships during this challenging time. These strategies aim to promote open communication, understanding, and shared decision-making:
- Facilitating Communication: Encourage open dialogue among family members. Provide a safe space for everyone to express their feelings and concerns without judgment.
- Clarifying Roles and Expectations: Help family members define their roles clearly to avoid misunderstandings. Set realistic expectations for caregiving responsibilities and emotional support.
- Conflict Resolution: Offer mediation or conflict resolution techniques when disagreements arise. This may involve identifying common goals and finding compromises that respect everyone’s perspective.
- Involving Professional Support: Suggest the involvement of social workers, counselors, or family therapists to address emotional or relational issues. These professionals can offer expert guidance in navigating complex family dynamics.
- Providing Education: Educate the family on the patient’s condition and prognosis, as well as available resources, to help them make informed decisions and manage expectations.
- Encouraging Self-Care: Remind family members to prioritize their own well-being. Caregiver burnout can negatively impact the entire family system, so encourage rest, relaxation, and support outside of the caregiving role.
By addressing these challenges with empathy, clear communication, and effective strategies, families can navigate the complexities of caregiving more effectively. This support not only benefits the patient but also strengthens the family unit, ensuring that everyone feels heard, supported, and empowered during this difficult time.
Legal Aspects of Palliative Care
When addressing the needs of individuals with serious and life-limiting conditions, it is essential to consider the legal framework surrounding treatment decisions, patient rights, and responsibilities. Healthcare professionals must navigate a range of ethical, legal, and regulatory guidelines to ensure that the patient’s dignity is upheld while meeting the legal obligations involved in providing appropriate support. Understanding these legal aspects ensures that care is delivered in accordance with both the law and the patient’s wishes.
Key Legal Considerations
There are several crucial legal issues that impact the approach to supporting patients with serious illnesses. Below are the key considerations that healthcare professionals must be aware of:
| Legal Aspect | Description |
|---|---|
| Patient Autonomy | Respecting the right of individuals to make their own decisions about treatment, including the right to refuse treatment or withdraw consent. |
| Advance Directives | Documents such as living wills or healthcare proxies that specify a patient’s wishes in case they are unable to communicate them later. |
| Informed Consent | The process by which a patient is fully informed of the risks, benefits, and alternatives of proposed treatments before making a decision. |
| Confidentiality | Ensuring that patient information is kept private, with information only disclosed to relevant parties as permitted by law or with patient consent. |
| End-of-Life Decisions | Legal implications of decisions regarding the discontinuation of life-sustaining treatments, including issues surrounding euthanasia and assisted suicide, where permissible by law. |
Managing Legal Risk
In a setting where end-of-life decisions are often made, healthcare providers must be diligent in managing legal risks while providing compassionate care. Key strategies to reduce legal risk include:
- Documentation: Carefully document all decisions, patient preferences, discussions, and actions taken. Accurate records help to protect both the healthcare team and the patient’s wishes.
- Patient Advocacy: Actively support the patient’s rights and preferences, ensuring that their wishes are respected, even when faced with difficult decisions.
- Consultation with Legal Experts: When faced with complex legal questions or concerns, consulting legal counsel can help healthcare providers navigate potential pitfalls and clarify ambiguities.
- Regular Review of Policies: Ensure that care practices and organizational policies are in alignment with current legal requirements and best practices in the field.
By considering the legal implications of treatment and decisions at every stage, healthcare providers can mitigate legal risks while fostering an environment that prioritizes patient well-being and autonomy. This approach helps maintain trust between the healthcare team, the patient, and their family, while ensuring compliance with legal standards and ethical guidelines.
Cultural Sensitivity in End-of-Life Care
When supporting individuals at the end of their lives, it is essential to recognize and respect cultural differences that influence their beliefs, values, and practices. Understanding these cultural factors enables healthcare providers to deliver compassionate, individualized care that aligns with the patient’s and family’s needs. Fostering cultural awareness helps build trust and ensures that treatment plans are both effective and respectful of diverse backgrounds.
Healthcare professionals must be aware that cultural beliefs can significantly impact how patients and their families perceive illness, death, and treatment options. Sensitivity to these differences is not only ethical but can also improve the quality of care and overall patient satisfaction. Being attuned to cultural preferences ensures that patients receive the support they need in a manner that is respectful of their heritage and personal beliefs.
Key Areas of Cultural Sensitivity
Here are several critical aspects to consider when providing care in a culturally sensitive manner:
- Understanding Beliefs About Death: Different cultures have unique views on death, the afterlife, and the rituals that accompany the dying process. Acknowledging and respecting these beliefs helps create a supportive environment for both the patient and their family.
- Communication Preferences: Some cultures may have specific ways of expressing or receiving information, particularly about sensitive topics like death or prognosis. Ensuring clear, respectful communication is crucial to providing effective support.
- Family Roles: In many cultures, family plays a central role in decision-making, especially when it comes to health-related matters. Understanding the family dynamics and who has the authority to make decisions can help ensure that the patient’s wishes are honored.
- Spiritual Needs: Spiritual beliefs can be an essential aspect of a patient’s comfort and peace of mind at the end of life. Healthcare providers should be aware of and accommodate spiritual practices, including the need for prayer, religious rituals, or the presence of spiritual leaders.
Best Practices for Cultural Sensitivity
Healthcare providers can adopt several strategies to ensure that their care is culturally sensitive and appropriate:
- Education and Training: Regular cultural competence training for healthcare professionals helps to raise awareness about cultural differences and teaches practical skills for interacting with patients from diverse backgrounds.
- Active Listening: Engage with patients and families by actively listening to their concerns, preferences, and beliefs. This approach fosters mutual respect and ensures that care is tailored to their needs.
- Inclusive Policies: Develop and implement inclusive policies that promote cultural sensitivity across all aspects of care, from communication to spiritual support.
- Personalized Care Plans: Work with the patient and their family to develop care plans that respect their cultural and personal preferences while ensuring that medical needs are met.
Incorporating cultural sensitivity into end-of-life care enhances the patient’s experience and ensures that the treatment process is respectful, compassionate, and effective. By prioritizing cultural awareness, healthcare providers can improve outcomes and help patients and families navigate the challenges of this difficult time with dignity and understanding.
Role of the Palliative Care Team
A multidisciplinary team plays a vital role in providing comprehensive support to patients facing serious illness, ensuring that both physical and emotional needs are addressed. These teams consist of healthcare professionals from various specialties, each bringing their expertise to create a holistic approach to patient well-being. Collaboration within the team enhances the quality of care, helping to improve the patient’s experience during a challenging time.
The team’s role extends beyond managing symptoms; it involves providing emotional, psychological, and spiritual support, offering practical advice, and facilitating clear communication between patients, families, and other healthcare providers. The aim is to offer personalized care that respects the patient’s wishes and helps them live as fully and comfortably as possible.
Key Members of the Team
Each member of the team contributes to different aspects of care, ensuring a well-rounded approach:
- Physicians: Doctors oversee the medical treatment, managing symptoms and adjusting medications as necessary to provide relief.
- Nurses: Nurses play a crucial role in monitoring the patient’s condition, administering treatments, and offering ongoing support to both the patient and family.
- Social Workers: Social workers assist with practical needs, such as navigating healthcare systems, addressing financial concerns, and providing emotional support to families.
- Chaplains or Spiritual Care Providers: These professionals provide spiritual support, helping patients and families cope with existential concerns and offering guidance based on their beliefs and traditions.
- Psychologists or Counselors: Mental health professionals offer counseling and therapeutic support to help patients and families manage stress, anxiety, and depression.
Collaborative Approach to Patient Support
The success of the team lies in its ability to collaborate effectively. Regular meetings and open communication between team members ensure that every aspect of the patient’s well-being is addressed. The team works together to tailor a care plan that aligns with the patient’s goals and values, while also supporting the family through education and resources.
By working as a cohesive unit, the team ensures that all aspects of care–physical, emotional, social, and spiritual–are considered, offering patients a comprehensive and compassionate approach that addresses their unique needs. This collaborative effort fosters an environment of support and respect for the patient’s dignity during one of the most challenging times in life.
Documentation and Record-Keeping in Care
Accurate and thorough documentation is essential in providing high-quality healthcare, especially when managing patients with serious or life-limiting conditions. It serves as a record of the patient’s treatment, progress, and any changes in their condition. Proper record-keeping ensures that all healthcare providers are informed and can make well-informed decisions, fostering continuity and consistency in the patient’s treatment plan.
Effective documentation not only provides a detailed account of interventions, symptoms, and responses, but also ensures compliance with legal, ethical, and organizational standards. It helps to track the effectiveness of treatments, guide decision-making, and communicate important information to the entire healthcare team. Additionally, it is an essential tool for families, providing them with clarity about the care process and the decisions made regarding their loved one’s health.
Clear and comprehensive records are vital for understanding the patient’s needs and for providing the best possible care. This information can be used to adjust treatment plans as necessary and ensures that no crucial detail is overlooked in the provision of services.
Preparing for the Palliative Care Exam
Preparing for an assessment in this field requires a strategic approach, focusing on both theoretical knowledge and practical skills. Success in the evaluation relies on a deep understanding of patient management in sensitive and complex situations. It is essential to familiarize oneself with the key concepts and frameworks used in providing support to individuals facing life-limiting conditions, as well as the ethical, legal, and emotional aspects of treatment.
Here are some tips to help structure your study approach:
- Understand Core Principles: Study the underlying principles that guide treatment decisions and patient interactions. Be clear about the roles of various team members and the importance of a holistic approach to care.
- Review Medical Interventions: Focus on both pharmacological and non-pharmacological treatments commonly used for symptom management, and their applications in real-world scenarios.
- Study Patient-Centered Care Approaches: Know the strategies for improving the quality of life of patients, including communication techniques, pain relief methods, and psychosocial support.
- Understand Ethical Considerations: Familiarize yourself with ethical dilemmas and the legal frameworks surrounding decision-making in sensitive situations.
- Practice Case Scenarios: Engage in case study analysis, applying your knowledge to hypothetical situations. This will help you think critically and manage real-life scenarios effectively.
- Stay Updated on Guidelines: Ensure you’re familiar with the latest healthcare policies, best practices, and treatment protocols that govern patient care in these contexts.
By approaching your preparation methodically, you will be able to approach the assessment with confidence, demonstrating not only technical expertise but also a compassionate understanding of the human aspect of care.
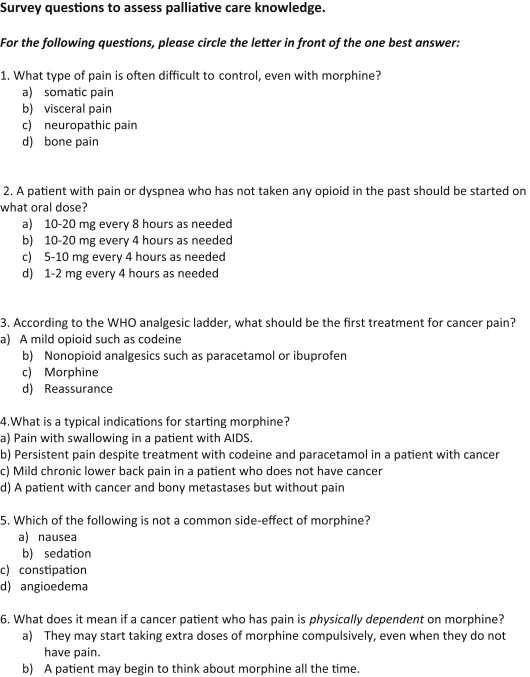
Reviewing Common Exam Questions and Answers
When preparing for assessments in this field, it’s important to become familiar with frequently encountered topics and common challenges that might arise in testing scenarios. Understanding the types of inquiries and how to approach them critically can help reinforce knowledge and improve performance. This section provides an overview of key subjects that are often covered in evaluations, offering insight into what to expect and how to best respond.
Key Topics Often Covered
Some of the most commonly examined areas include:
- Symptom Management Strategies: Understanding the various methods for alleviating common symptoms such as pain, nausea, and breathlessness.
- Ethical Considerations: Questions that address moral dilemmas, such as patient autonomy, end-of-life decisions, and the role of family involvement in treatment planning.
- Multidisciplinary Team Approach: Assessing how to work effectively with a diverse healthcare team and recognizing each member’s role in delivering comprehensive support to patients.
- Communication Skills: Queries about how to handle sensitive conversations with patients and families, ensuring clarity, empathy, and respect.
Effective Response Techniques
To respond to these types of inquiries, it’s important to:
- Be Thorough: Provide detailed responses that showcase both knowledge and understanding of the subject matter.
- Focus on Practical Applications: Relate theoretical concepts to real-world scenarios, demonstrating how they can be effectively implemented in practice.
- Use Structured Formats: When appropriate, organize responses using clear frameworks such as the SOAP (Subjective, Objective, Assessment, Plan) method, ensuring logical progression and clarity in your explanations.
By familiarizing yourself with these common topics and developing strategies to address them effectively, you will be better prepared for the challenges of the evaluation process.