When evaluating an individual’s ability to walk, healthcare professionals focus on various factors that contribute to mobility. These include the coordination of movement, posture, balance, and the ability to adjust walking patterns based on different situations. Understanding these elements is crucial in diagnosing various conditions that affect movement and posture.
For those preparing to assess or interpret walking abilities, it’s essential to be familiar with common physical signs that indicate underlying issues. This section explores a range of potential challenges faced during walking assessments, offering insights into the most frequently observed difficulties and how they are addressed during clinical evaluations.
By reviewing typical problems and the strategies used to assess them, individuals can gain a deeper understanding of movement-related conditions. This knowledge is key for both medical professionals and those studying to improve their diagnostic skills in physical health.
Evaluation of Walking Abilities
Understanding how movement patterns are assessed is essential for identifying issues that affect mobility. Medical professionals often rely on structured methods to examine how individuals move, identifying specific challenges that may indicate neurological or musculoskeletal disorders. In this section, we explore key aspects of movement evaluation, including typical concerns that arise during assessments and the ways in which clinicians interpret these observations.
Common Issues Identified During Movement Assessments
- Difficulty maintaining balance while walking
- Unusual leg or foot positioning
- Asymmetry in movement between the left and right side of the body
- Slowness or irregularity in the pace of walking
- Compensatory postures to prevent falling
Typical Scenarios in Movement Analysis
- Posture and Balance: Identifying abnormalities in posture that may suggest neurological or muscular disorders.
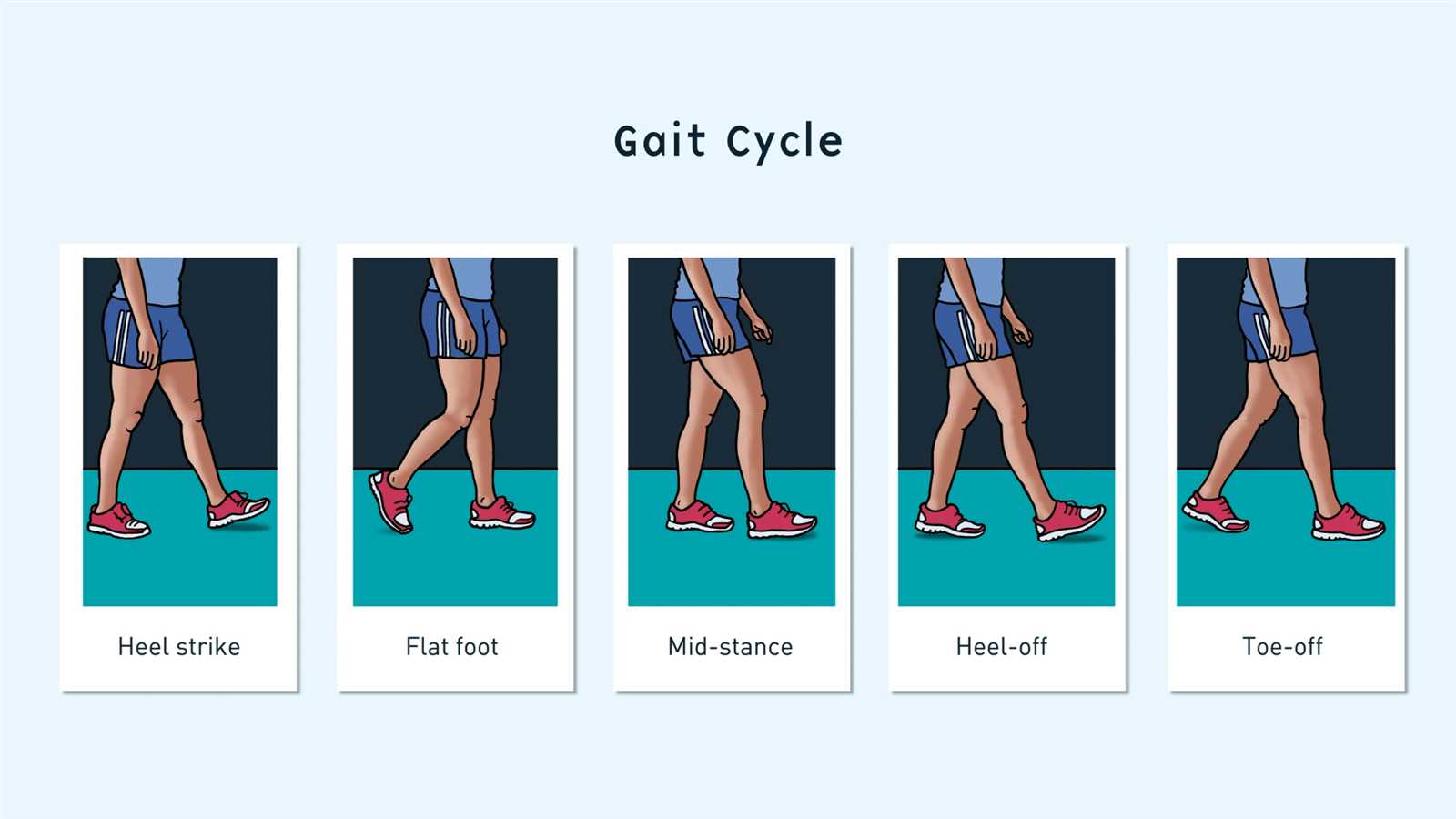
- Foot Placement: Recognizing changes in how the feet are placed during walking, which can indicate problems in the lower limbs or the nervous system.
- Coordinated Movement: Evaluating how well the individual coordinates leg and arm movements, which is crucial for assessing motor control.
By thoroughly understanding these common challenges, healthcare professionals are better equipped to provide effective diagnosis and treatment plans for patients with movement-related difficulties.
Understanding the Movement Evaluation Process
The process of evaluating an individual’s walking patterns involves several stages aimed at identifying physical or neurological issues that may affect mobility. This assessment typically begins with a visual inspection to detect any immediate irregularities in posture, movement, or coordination. After the initial observation, more specific tests are performed to examine the range of motion, strength, and balance. These methods help clinicians understand the underlying causes of mobility challenges and guide the development of an appropriate treatment plan.
Various factors are considered during the evaluation to ensure that the assessment is thorough. The following table highlights key components of a typical movement analysis:
| Component | Description |
|---|---|
| Visual Observation | Clinicians first observe the patient’s posture and movement for any obvious abnormalities or asymmetries. |
| Range of Motion | Testing how far the joints and muscles can move helps identify restrictions or stiffness that may impact mobility. |
| Strength Assessment | Evaluating the strength of key muscles in the lower body and core to ensure proper support during walking. |
| Balance Tests | Checking how well the individual can maintain balance while performing tasks like standing or walking in place. |
| Coordination Evaluation | Assessing how well the arms and legs work together, which is crucial for maintaining fluid and coordinated movement. |
Each of these elements plays a critical role in the overall assessment, helping clinicians to identify potential causes of walking difficulties. By combining these different aspects, a clear picture of an individual’s mobility is formed, enabling the development of a targeted treatment strategy.
Key Walking Patterns to Recognize
Recognizing common movement patterns is essential for identifying underlying health conditions. Distinctive patterns can indicate a variety of issues, ranging from neurological disorders to musculoskeletal problems. By carefully observing how an individual moves, healthcare professionals can detect signs of imbalance, weakness, or abnormal posture that may suggest the need for further investigation or intervention.
Several characteristic patterns are commonly seen during movement assessments, each associated with specific conditions or impairments. These include:
- Antalgic Walking: This pattern involves a limp or uneven stride, often due to pain in one leg. The affected side is typically avoided to minimize discomfort.
- Ataxic Walking: Individuals with this pattern have difficulty maintaining balance, often swaying or staggering as they walk. This is commonly seen in patients with cerebellar disorders.
- Festinating Walking: Characterized by a shuffling motion, this pattern is often associated with Parkinson’s disease. Individuals may appear to take small, rapid steps, sometimes accompanied by difficulty stopping.
- Trendelenburg Gait: This pattern is marked by a dropping of the pelvis on the opposite side when the affected leg is raised. It is usually caused by weakness in the hip abductor muscles.
- Hemiplegic Walking: Often seen after a stroke, this pattern involves a stiff, dragging leg, with the person swinging it outward in a circular motion while walking.
Identifying these patterns early can be crucial in diagnosing the root cause of movement difficulties and guiding appropriate treatment plans. Recognizing these signs can assist healthcare providers in offering timely interventions to improve mobility and overall quality of life.
Common Disorders Detected in Movement Assessments
During mobility assessments, certain physical and neurological disorders are often identified based on abnormal walking patterns or difficulty with movement. These conditions can range from musculoskeletal injuries to complex neurological diseases. Identifying these issues early is crucial in determining the appropriate treatment and rehabilitation options.
Musculoskeletal Conditions
- Osteoarthritis: A degenerative joint disease that causes pain, stiffness, and swelling, leading to difficulty with walking and limited range of motion.
- Hip Impingement: Abnormal contact between the ball and socket of the hip joint can cause pain and limping, particularly during walking or other weight-bearing activities.
- Plantar Fasciitis: Inflammation of the tissue on the bottom of the foot, often causing pain with each step, which can alter the walking pattern.
- Foot Drop: A condition where the foot drags or does not lift properly, often due to nerve damage affecting the muscles responsible for foot movement.
Neurological Conditions
- Parkinson’s Disease: A progressive neurological disorder that often causes slow, shuffling steps, difficulty starting or stopping movement, and poor posture while walking.
- Multiple Sclerosis: A disease that affects the central nervous system, leading to weakness, poor coordination, and unsteady walking patterns.
- Cerebellar Ataxia: Caused by damage to the cerebellum, this condition results in uncoordinated, staggering movement and difficulty maintaining balance.
- Stroke: A stroke can cause hemiplegia or paralysis on one side of the body, leading to abnormal walking patterns as the individual compensates for weakness.
Recognizing these disorders early during a movement assessment allows for timely diagnosis and intervention, helping to improve the individual’s mobility and prevent further complications.
How to Prepare for a Mobility Assessment
Preparing for a movement evaluation involves both physical and mental readiness. It is important to ensure that the body is in a state conducive to performing the necessary tasks during the assessment, as well as understanding the process itself. This will help you to perform your best and provide accurate information for the healthcare provider conducting the evaluation.
Physical Preparation
- Wear Comfortable Clothing: Choose loose-fitting clothes that allow freedom of movement, especially around the legs and hips.
- Footwear: Wear supportive shoes that are appropriate for walking. Avoid high heels or sandals that lack support.
- Avoid Intense Physical Activity: It is helpful to refrain from strenuous activity or exercise right before the assessment to prevent fatigue that may affect movement.
- Rest Well: Ensure that you are well-rested, as fatigue can impact your ability to walk or balance properly during the assessment.
Mental Preparation
- Understand the Process: Familiarize yourself with the types of movements that may be tested, such as walking, standing, or turning, to feel more confident during the assessment.
- Focus on Natural Movements: Try to perform tasks as naturally as possible, as this will provide the most accurate results for your healthcare provider.
- Prepare for Questions: Be ready to answer questions regarding any previous injuries, surgeries, or conditions that might affect your movement.
By preparing both physically and mentally, you can ensure that the evaluation is as smooth and informative as possible. This will enable the healthcare professional to make the most accurate assessment and provide the best recommendations for your care.
Clinical Signs of Abnormal Walking Patterns
Abnormalities in movement often reveal underlying health conditions. Recognizing these signs early is crucial for diagnosing potential issues related to the nervous system, muscles, or joints. Healthcare professionals can identify various clinical signs during an assessment that indicate a need for further investigation and treatment. These signs are typically reflected in how a person moves, the symmetry of their movements, and the ease with which they maintain balance.
Signs of Postural Imbalance
- Uneven Shoulders or Pelvis: A noticeable tilt or drop in the shoulders or pelvis while walking may indicate muscle weakness or neurological conditions.
- Forward Leaning: If the individual leans forward while walking, it may suggest issues with balance or postural control, often seen in conditions like Parkinson’s disease.
- Unstable Stance: Difficulty maintaining balance while standing, or swaying from side to side, can indicate poor coordination or muscle weakness.
Irregular Movement Patterns
- Shuffling Steps: A slow, small-step pattern with little lift of the feet can be seen in individuals with Parkinson’s disease or other motor impairments.
- Stiff or Rigidity in Movement: When the arms do not swing naturally or the legs appear stiff, it may point to neurological disorders such as Parkinson’s or multiple sclerosis.
- Foot Dragging: Dragging a foot while walking may suggest nerve damage, such as foot drop, or weakness in the muscles controlling foot movement.
Identifying these clinical signs is essential for early intervention and treatment, as abnormal walking patterns often serve as early indicators of more serious health conditions.
Questions on Postural Stability During Movement
Postural stability is a critical component of walking and overall mobility. When an individual moves, maintaining a stable posture ensures balance and reduces the risk of falls. Healthcare professionals often focus on this aspect during mobility assessments to evaluate how well a person controls their body position, particularly when performing dynamic tasks such as walking or changing direction. Understanding the factors that affect balance and posture is key to diagnosing and treating any underlying issues that may compromise stability.
Factors Affecting Postural Stability
- Strength of Core Muscles: Weak abdominal and back muscles can impair the body’s ability to stay upright and balanced during movement, leading to instability.
- Neurological Health: Conditions like stroke, multiple sclerosis, or Parkinson’s disease can disrupt the brain’s ability to coordinate posture and movement, resulting in poor stability.
- Visual and Vestibular Systems: The eyes and inner ear play a vital role in maintaining balance. Issues with vision or the vestibular system can lead to postural instability during movement.
Assessing Postural Control
- Standing Balance: Is the individual able to stand without swaying or using support for long periods of time?
- Ability to Change Directions: How well does the person maintain their balance when turning or changing walking patterns, such as stepping sideways or backward?
- Recovery from Loss of Balance: Can the individual recover quickly from a stumble or shift in weight, or do they require assistance to regain stability?
Understanding these aspects of postural control provides valuable insights into a person’s mobility and helps clinicians develop targeted interventions to improve stability and prevent falls.
Tests for Lower Limb Coordination
Evaluating coordination in the lower limbs is essential for assessing overall mobility and motor function. Proper coordination ensures that movements are smooth and purposeful, helping individuals maintain balance, walk efficiently, and perform daily tasks. Various tests are used to assess lower limb coordination, helping to identify weaknesses, neurological impairments, or other conditions that may interfere with normal movement patterns. These tests often focus on the ability to control movement, maintain stability, and react to changes in posture or movement direction.
Common Coordination Tests
- Heel-to-Shin Test: The individual is asked to run the heel of one foot along the shin of the opposite leg. This test evaluates the precision and smoothness of the movements.
- Romberg Test: The individual is asked to stand with their feet together and eyes closed. This test evaluates balance and the ability to maintain stability without visual input.
- Finger-to-Toe Test: The individual is asked to touch their finger to their toe while standing. This test assesses both coordination and balance.
Test for Muscle Control and Timing
| Test | Purpose | Outcome |
|---|---|---|
| Rapid Alternating Movements | To assess the ability to perform quick, alternating movements with the lower limbs. | Difficulty may indicate coordination issues due to neurological or muscular conditions. |
| Step Test | To evaluate the ability to step in place or in a controlled pattern. | Inability to maintain a smooth, controlled stepping motion may suggest deficits in coordination. |
By performing these tests, healthcare providers can identify potential issues with muscle control, reflexes, or coordination, which are crucial for maintaining functional movement and preventing falls.
Understanding Walking Disturbances in Neurology
Walking disturbances often serve as early indicators of neurological conditions. The ability to walk smoothly and maintain balance relies on complex interactions between the brain, spinal cord, nerves, and muscles. When these systems are disrupted by disease or injury, various movement abnormalities can arise. These disturbances can manifest in different ways, including difficulty with coordination, abnormal posture, or imbalanced movement patterns. Understanding the underlying causes of these issues is crucial for diagnosing neurological conditions and providing effective treatments.
Neurological conditions that affect walking typically involve impairments in the brain’s ability to coordinate motor functions, leading to a range of symptoms. These can include tremors, weakness, stiffness, or even a loss of motor control, all of which impact a person’s ability to move efficiently. Recognizing these patterns is essential for early intervention, as many of these disorders can worsen if left untreated.
Common Neurological Causes of Walking Disturbances
- Parkinson’s Disease: A degenerative disorder that affects movement, causing stiffness, tremors, and shuffling steps. People with Parkinson’s often have difficulty initiating or stopping movement.
- Multiple Sclerosis: A disease where the immune system attacks the protective covering of nerve fibers, leading to loss of coordination, weakness, and balance issues.
- Stroke: A stroke can damage the brain areas responsible for motor control, leading to partial paralysis or weakness on one side of the body, affecting walking ability.
- Cerebellar Ataxia: A condition that affects the cerebellum, the part of the brain responsible for coordination, leading to unsteady, staggering movements and poor balance.
Recognizing Walking Patterns Indicative of Neurological Disorders
- Shuffling Walk: Often seen in Parkinson’s disease, where steps are small and dragging, with little arm swing.
- Wide-Based Walk: A wider stance is commonly associated with cerebellar ataxia and other disorders affecting balance.
- Unsteady Movements: Stumbling or falling without clear cause, frequently seen after a stroke or in people with neurological impairments.
- Difficulty with Turning: Struggling to make turns or changes in direction, particularly when combined with stiffness or rigidity, is indicative of motor control problems.
Recognizing the signs of walking disturbances early on allows healthcare providers to pinpoint potential neurological conditions and recommend appropriate treatments or therapies to manage symptoms and improve mobility.
Examining Walking Patterns in Elderly Patients
As people age, maintaining a smooth and stable walking pattern becomes more challenging due to a variety of physical and neurological changes. Evaluating movement in elderly individuals is essential for identifying potential issues such as weakness, joint problems, or balance impairments that could increase the risk of falls. Thorough assessment helps healthcare providers understand the underlying causes of mobility problems and develop effective interventions to improve mobility and prevent injury.
For older adults, movement difficulties often arise from a combination of factors, including reduced muscle strength, joint stiffness, decreased flexibility, and neurological conditions such as dementia or stroke. These factors can lead to slower walking speeds, difficulty maintaining balance, or altered posture. Early detection of these issues through careful observation and testing is crucial for maintaining independence and enhancing the quality of life for elderly individuals.
Key Factors to Consider in Elderly Mobility Assessment
- Muscle Strength: Decreased muscle strength, especially in the legs, can lead to difficulties in walking and balancing.
- Joint Health: Arthritis or other joint conditions can affect the range of motion, causing pain or stiffness that disrupts movement.
- Balance and Coordination: Age-related changes in the inner ear and brain can impair balance and coordination, making it harder to walk steadily.
- Vision: Poor eyesight can affect the ability to judge distance and avoid obstacles while walking.
Common Mobility Issues in Older Adults
- Shuffling Walk: A common symptom where the individual takes small, dragging steps, often seen in conditions like Parkinson’s disease.
- Wide-Based Stance: A broader stance is often adopted to compensate for balance issues, making walking appear unsteady.
- Slow Walking Speed: Reduced walking speed is frequently observed due to muscle weakness, joint discomfort, or fear of falling.
- Difficulty with Turns: Older adults may struggle with turning while walking, often hesitating or taking extra steps to change direction.
Evaluating walking patterns in elderly patients helps identify early signs of deterioration and enables healthcare providers to offer targeted interventions such as physical therapy, assistive devices, or lifestyle changes that can improve mobility and reduce the risk of falls.
Impact of Musculoskeletal Conditions on Walking Patterns
Musculoskeletal conditions can significantly alter the way a person moves, often leading to discomfort, instability, and difficulty with daily activities. These conditions affect the bones, joints, muscles, and connective tissues, all of which play crucial roles in maintaining proper movement and balance. When one or more of these systems is impaired, it can result in abnormal movement patterns, causing an individual to adjust their walking style in order to compensate for pain, weakness, or limited mobility.
As musculoskeletal conditions progress, they often lead to changes in posture, walking speed, stride length, and balance. Individuals may develop altered gait mechanics as a way to reduce pain or avoid further injury. Understanding how musculoskeletal issues affect walking is essential for providing appropriate treatment and support to improve mobility and prevent further complications.
Common Musculoskeletal Disorders Affecting Movement

- Osteoarthritis: A degenerative joint disease that causes pain, swelling, and stiffness, especially in weight-bearing joints like the knees and hips. It often leads to a limping gait or reduced walking speed.
- Rheumatoid Arthritis: An autoimmune disorder that results in inflammation and pain in the joints. This condition can cause joint deformities and reduced range of motion, leading to an altered walking pattern.
- Fractures: Broken bones, especially in the lower limbs, can lead to a limp or difficulty in bearing weight on the affected leg, causing asymmetry in walking.
- Muscle Weakness: Conditions like muscular dystrophy or generalized muscle atrophy can reduce strength in the legs and core, leading to instability and an unsteady walking pattern.
How Musculoskeletal Conditions Impact Movement
- Reduced Range of Motion: Stiff joints or muscles with limited flexibility can cause a person to take shorter, slower steps, reducing walking efficiency.
- Pain-Driven Compensation: Individuals may change their walking pattern to avoid pain in specific joints or muscles, which may result in a limp or an uneven gait.
- Instability: Joint instability, especially in the knees or hips, can cause a person to have difficulty maintaining balance, leading to slower walking or a wide-based stance.
- Fatigue: Chronic musculoskeletal conditions often result in fatigue, making it harder for individuals to walk for extended periods or with proper form.
Effective management of musculoskeletal conditions involves a combination of medical treatment, physical therapy, and lifestyle adjustments to help improve walking patterns, reduce pain, and enhance mobility. Early detection and intervention can help mitigate the impact of these conditions on an individual’s overall movement and quality of life.
Neurological Causes of Walking Abnormalities
Neurological conditions can significantly affect the way a person walks by impairing the brain’s ability to properly coordinate movement. These disorders often disrupt the communication between the brain, spinal cord, and muscles, leading to instability, weakness, or abnormal movement patterns. Conditions such as stroke, Parkinson’s disease, and multiple sclerosis can cause a range of symptoms that impact an individual’s ability to maintain a steady, efficient walking pattern. Identifying these issues early on is crucial for providing effective treatment and preventing further complications.
When neurological dysfunction is present, walking may appear slow, uncoordinated, or even rigid, depending on the severity of the condition. These abnormalities can make even simple tasks, like standing up or navigating through a room, more challenging. Understanding the neurological causes of movement disorders helps clinicians tailor rehabilitation and therapeutic approaches to improve the patient’s mobility and quality of life.
Common Neurological Conditions Affecting Walking
- Parkinson’s Disease: A progressive neurological disorder that leads to rigidity, tremors, and bradykinesia (slowness of movement). A person with Parkinson’s disease may exhibit a shuffling walk, difficulty initiating movement, and balance issues.
- Stroke: A stroke can cause paralysis or weakness on one side of the body, making walking uneven or difficult. A person may drag one foot or lean to one side, impairing their ability to walk normally.
- Multiple Sclerosis: This autoimmune disease attacks the central nervous system, leading to muscle weakness, coordination problems, and spasticity. It can result in an unsteady walk or difficulty maintaining balance.
- Cerebral Palsy: A group of disorders that affect muscle coordination and movement control, often present from birth. It can cause a stiff, uneven walking pattern due to muscle tightness and poor coordination.
Neurological Symptoms Impacting Walking
- Muscle Weakness: Weakness in the legs or core muscles due to neurological impairment can result in difficulty lifting the feet or maintaining balance.
- Spasticity: Increased muscle tone can lead to stiffness in the limbs, causing jerky movements or difficulty swinging the arms while walking.
- Impaired Coordination: Neurological disorders can impair the brain’s ability to coordinate movements, resulting in an uncoordinated or ataxic walk, with poor foot placement and stumbling.
- Balance Problems: Many neurological conditions affect the vestibular system or the cerebellum, leading to problems with postural stability and increased risk of falls.
Addressing the neurological causes of movement abnormalities often involves a multidisciplinary approach, including medications, physical therapy, and in some cases, surgical interventions. Early diagnosis and intervention are essential to improving walking abilities and overall function in individuals affected by neurological disorders.
Evaluating the Role of Foot Position
Foot positioning plays a critical role in maintaining stability and balance during walking. The way the feet are placed, whether they are aligned properly or turned in certain directions, directly influences the efficiency of movement and the risk of falls. Even subtle abnormalities in foot placement can cause or exacerbate walking difficulties, affecting overall mobility. In clinical assessments, evaluating the position of the feet can provide valuable insights into potential musculoskeletal or neurological conditions.
Proper alignment ensures that each step is executed with maximum stability and minimal strain on the body. However, improper foot positioning may lead to compensation in other parts of the body, resulting in discomfort, altered walking patterns, and even long-term joint or muscle issues. Clinicians carefully observe foot placement to determine whether there are any contributing factors to abnormal movement or balance problems.
Common Foot Position Abnormalities
- In-Toeing: This occurs when the feet point inward during walking, often due to structural issues in the legs or hips. In-toeing can affect balance and lead to uneven wear on the joints.
- Out-Toeing: The outward rotation of the feet can cause strain on the knees and hips, often leading to an inefficient walking pattern and increased risk of falls.
- Flat Feet: Also known as pes planus, flat feet can cause the arch of the foot to collapse, leading to overpronation, which may alter gait dynamics and contribute to discomfort or pain in the lower limbs.
- High Arches: Excessively high arches (pes cavus) may result in insufficient shock absorption during walking, leading to joint stress and discomfort, especially in the ankles and knees.
Impact of Foot Position on Movement
- Shock Absorption: Proper foot alignment helps in absorbing the impact of each step. Misalignment can disrupt this process, leading to joint strain or discomfort in the legs and lower back.
- Balance and Stability: Foot position directly influences balance. Incorrect foot placement may lead to instability, increasing the risk of falls, particularly in individuals with weakened muscles or coordination problems.
- Energy Efficiency: When the feet are properly aligned, movement is more efficient, requiring less energy to maintain a steady pace. Poor foot position can lead to energy inefficiencies and muscle fatigue.
By observing and correcting foot placement during assessment, healthcare providers can identify contributing factors to movement dysfunctions and work toward improving overall mobility through corrective exercises, footwear modifications, or more advanced interventions when necessary.
Gait Analysis for Parkinson’s Disease
Parkinson’s disease significantly impacts the way individuals walk, leading to various challenges in movement and balance. As the disease progresses, patients often experience changes in their walking patterns, which can affect their ability to move independently and safely. Analyzing these changes is crucial for understanding the severity of the disease and for developing effective treatment strategies. Through careful observation and measurement of walking characteristics, healthcare providers can assess how Parkinson’s disease influences mobility and identify potential interventions to improve patient quality of life.
Key aspects of walking, such as step length, cadence, and posture, can be altered in patients with Parkinson’s disease. These changes often result in a characteristic pattern, including smaller, shuffling steps and reduced arm swing. By evaluating these factors, clinicians can monitor the progression of the disease and tailor treatment plans to address specific movement difficulties, thereby enhancing mobility and reducing the risk of falls.
Common Walking Disturbances in Parkinson’s Disease
| Disturbance | Description |
|---|---|
| Shuffling Steps | Reduced step length and increased contact with the floor, often leading to a slow, dragging walk. |
| Reduced Arm Swing | Loss of natural arm movement during walking, which can lead to a more rigid, less fluid gait. |
| Freezing of Gait | Temporary inability to move, often triggered by obstacles or stressful situations, which can increase the risk of falls. |
| Postural Instability | Difficulty maintaining an upright posture, which increases the risk of falls due to balance problems. |
Methods for Analyzing Movement in Parkinson’s Disease
Several techniques can be employed to analyze movement disturbances in individuals with Parkinson’s disease. These assessments help to identify specific challenges in walking and can guide clinical decisions regarding treatment.
- Clinical Observation: A visual assessment of walking patterns, including the observation of stride length, arm swing, and posture.
- Timed Tests: Timed walking tests, such as the 10-meter walk test, can help measure walking speed and identify impairments in mobility.
- Wearable Sensors: Devices that track movement can provide objective data on walking parameters, such as step frequency and gait variability.
- Video Analysis: Recording and analyzing a patient’s walking patterns in various situations to detect subtle movement abnormalities.
Understanding how Parkinson’s disease affects walking is vital for tailoring individualized treatment plans. With regular gait analysis, healthcare providers can make informed decisions about therapy options, assistive devices, and rehabilitation strategies to enhance mobility and minimize the impact of movement disorders.
Assessing Balance in Walking Patterns
Evaluating how well a person maintains stability during movement is crucial in identifying potential issues that could lead to falls or injury. Walking patterns often provide valuable insights into an individual’s balance and coordination. Disruptions in this delicate process can result in various abnormalities, making it essential to assess stability during walking regularly. The assessment focuses on both static and dynamic balance, helping to identify weaknesses or instabilities that may not be immediately obvious during simple observation.
The role of balance in movement is multifaceted, involving multiple systems within the body. These systems include the musculoskeletal structure, sensory input, and neural control. Disruptions in any of these components can cause an individual to become unstable while walking. Therefore, it is important to consider various factors, such as posture, foot placement, and overall body alignment, when assessing how someone walks.
Key Indicators of Instability
- Postural Sway: Observable movement from side to side or front to back during standing or walking, indicating potential instability.
- Uneven Step Length: Differences in step length between legs may suggest a lack of balance and unequal distribution of weight.
- Loss of Arm Swing: Reduced arm movement can signal a lack of coordination or postural control, which often accompanies instability.
- Difficulty Turning: Trouble changing direction while walking can indicate issues with balance and motor coordination.
Methods for Evaluating Balance During Walking
There are several methods to assess how well an individual maintains balance during walking, which help clinicians develop effective treatment strategies. These methods include:
- Clinical Observation: Directly observing walking patterns in a controlled setting to detect signs of imbalance, such as unsteady steps or difficulty turning.
- Timed Tests: The Timed Up and Go (TUG) test or similar timed mobility tests assess how quickly an individual can get up from a chair, walk a short distance, and return.
- Balance Assessment Tools: Specialized tools like force plates or balance boards that provide data on weight distribution and center of pressure during movement.
- Wearable Technology: Sensors placed on the body or in shoes that track movement, providing real-time data on balance performance and walking efficiency.
By carefully assessing balance, healthcare providers can better understand the causes of instability and implement appropriate interventions to reduce the risk of falls. This might include exercises to strengthen muscles, improve posture, or assistive devices that offer extra support during walking. Early intervention is key to helping individuals maintain independence and improve quality of life.
What to Expect During a Gait Exam
When undergoing an evaluation for walking or movement abnormalities, you will be carefully observed to assess how you walk, stand, and balance. The purpose of this assessment is to identify any irregularities or issues that might affect your ability to move efficiently or safely. This process involves a combination of visual observation, physical tests, and sometimes specialized equipment to gather data about your posture, step patterns, and overall mobility. Depending on your condition, the evaluation may focus on detecting specific impairments or risks associated with walking.
Typically, the assessment will start with an overview of your medical history, including any relevant injuries, conditions, or symptoms that may impact your movement. Your healthcare provider will then observe how you stand, walk, and move during simple activities. This provides insight into your balance, strength, and coordination, and can help determine if there are underlying issues in your muscles, joints, or nervous system.
Initial Observations
- Posture: The clinician will observe your standing posture, checking for any misalignments or signs of weakness.
- Foot Position: They will look at how your feet are placed when standing and walking, noting if there is any abnormal positioning or uneven weight distribution.
- Walking Technique: Your walking pattern will be closely observed to identify any limping, dragging, or difficulty in stepping.
Additional Assessments
- Timed Mobility Tests: You may be asked to walk a short distance or perform certain tasks within a set amount of time, such as the Timed Up and Go test, to evaluate speed and balance.
- Strength and Flexibility: The provider may assess the strength of your legs, hips, and core to determine how they affect your walking ability.
- Balance Testing: Tests may be conducted to see how well you maintain stability while standing or walking, including standing on one foot or walking heel-to-toe.
In some cases, advanced tools such as motion sensors, force plates, or pressure mats may be used to gather more detailed information about your walking patterns. These tools help the provider measure how much force is applied with each step, the distribution of weight, and how efficiently your body moves.
Once the evaluation is complete, your healthcare provider will discuss the findings and recommend appropriate treatment options. These might include physical therapy, exercises to improve strength or flexibility, assistive devices, or referrals to specialists if further investigation is needed. The goal of the evaluation is to help you maintain or improve your mobility and prevent complications such as falls or joint problems.