Accurate medical billing plays a crucial role in the delivery of healthcare services. As health professionals strive to provide comprehensive care, proper categorization of procedures ensures that patients receive the appropriate services while also enabling healthcare providers to maintain smooth financial operations. Understanding the latest updates in medical billing procedures is vital for all parties involved in healthcare delivery.
Preventive healthcare services, particularly those focused on regular check-ups and screenings, are an essential aspect of maintaining long-term health. These appointments are designed to monitor health, detect potential risks, and ensure that any necessary treatments are initiated early. Correctly identifying the associated procedures and classifying them under the right categories ensures that both patients and healthcare systems benefit.
With the evolving landscape of healthcare regulations and guidelines, the process of billing for preventive care has become increasingly sophisticated. Understanding how the latest updates to healthcare classification systems affect these services can help practitioners avoid common errors and improve overall patient care. Keeping up with these changes is essential for maximizing reimbursements while ensuring accurate records are maintained for all preventive visits.
CPT Code for Preventive Healthcare Visit 2025
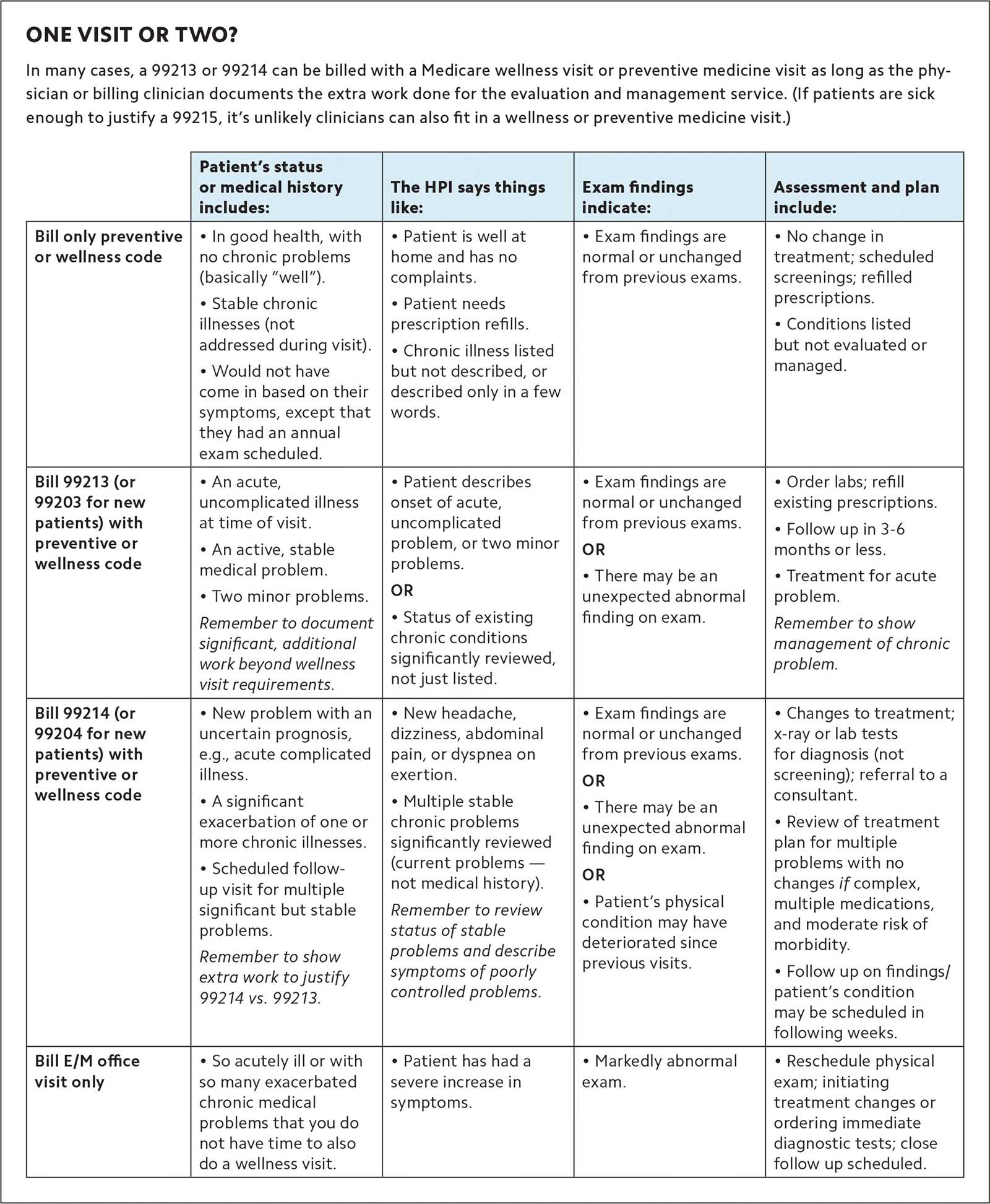
The process of classifying healthcare visits plays a significant role in ensuring proper billing and reimbursement. With regular health check-ups designed to detect early signs of disease or other health concerns, it is essential to understand how these services are documented. A clear understanding of the classification system helps both healthcare providers and insurance companies streamline operations while maintaining accuracy.
Preventive visits often include a range of services, such as screenings, immunizations, and health risk assessments. These services are considered essential for maintaining long-term health and detecting potential issues early. Accurate classification ensures that patients have access to necessary care, while also enabling providers to receive appropriate compensation for the services rendered.
In 2025, there are specific updates regarding the classification of preventive healthcare services. Changes may involve modifications to the way certain procedures are listed or adjustments to reimbursement rates. Understanding these shifts can help healthcare professionals avoid errors and ensure proper documentation is in place.
- Routine physical exams
- Screenings for chronic conditions
- Immunization updates
- Health risk assessments
- Counseling for healthy lifestyle choices
It is important for healthcare providers to familiarize themselves with the latest guidelines and updates to avoid mistakes in the billing process. This can lead to smoother financial transactions and more efficient care delivery, benefiting both patients and healthcare systems alike.
Understanding the Importance of Healthcare Classifications
Accurate classification of medical services is a critical aspect of healthcare management. It ensures that each service provided is properly documented, facilitating seamless reimbursement processes and maintaining the financial health of healthcare institutions. A clear and standardized system allows providers to be compensated fairly for the care they deliver, while also helping insurance companies to process claims efficiently.
Classification systems serve as a universal language between healthcare providers, insurance companies, and patients. These classifications provide clarity on the services rendered, ensuring that patients receive the necessary care and healthcare professionals are reimbursed appropriately. It also plays a role in tracking health trends, evaluating the quality of care, and monitoring the utilization of healthcare services.
Proper use of these systems is essential to minimize errors, reduce delays in payments, and avoid potential legal issues. Healthcare providers must be diligent in understanding the categories assigned to various services to ensure they align with regulatory standards. This is especially important as rules and regulations continue to evolve in response to changes in the healthcare landscape.
How Medical Classifications Affect Billing
In healthcare, the proper identification of services directly influences the billing process. Each service rendered must be classified under specific categories to ensure accurate compensation and reimbursement. These classifications provide a standardized way for insurance companies to assess the medical care provided and determine the appropriate payment for each service. Without accurate classification, healthcare providers could face delays or errors in receiving payments.
Billing accuracy is essential for maintaining smooth financial operations within healthcare institutions. The use of precise classifications helps minimize the risk of claim denials and ensures that the healthcare provider receives fair compensation for their services. It also reduces the administrative burden by streamlining the claims process, allowing staff to focus on patient care rather than dealing with billing discrepancies.
Furthermore, when healthcare professionals correctly apply these categories, they contribute to the overall transparency and efficiency of the healthcare system. Both providers and insurers can track healthcare spending and make informed decisions about care delivery and policy adjustments. An understanding of how these classifications affect billing is crucial for all parties involved, from the healthcare provider to the patient.
Overview of Preventive Health Check-up Requirements

A routine health check-up is essential for monitoring overall well-being and identifying potential health issues early. These visits are generally designed to assess a person’s health status, detect any underlying conditions, and provide preventive care. While the specifics of each appointment may vary depending on individual health needs, several key components are consistently included in these preventive visits to ensure a thorough evaluation.
Common elements of a comprehensive health assessment include physical examinations, screenings for various diseases, and advice on lifestyle modifications. During these visits, healthcare providers may also discuss the importance of vaccinations, reproductive health, and mental well-being. These assessments aim to catch potential problems before they develop into more serious conditions, allowing for timely intervention.
Additionally, the frequency and type of services offered during these visits can differ based on factors such as age, family history, and risk factors. It is crucial for healthcare providers to stay up to date with the latest guidelines and ensure that all necessary services are covered during these preventive visits. Proper documentation and classification of the services rendered are also important for maintaining accurate records and facilitating reimbursement processes.
What to Expect During a Preventive Health Check-up
A preventive health check-up is a key component of maintaining good health and preventing future medical issues. During these visits, healthcare professionals will assess your overall health, review your medical history, and address any concerns or symptoms you may have. These appointments are an opportunity to discuss various aspects of your health and receive guidance on how to stay healthy and prevent illness.
Physical Examination and Screenings
During the visit, your healthcare provider will conduct a physical examination to evaluate your general health and check for any signs of potential health issues. This may include measuring your height, weight, blood pressure, and heart rate. In addition to the physical examination, screenings for conditions such as diabetes, cholesterol levels, and certain cancers may be performed based on your age, risk factors, and medical history.
Health Education and Lifestyle Counseling

A key aspect of preventive visits is health education. Your provider will likely offer advice on maintaining a healthy lifestyle, including tips on nutrition, exercise, stress management, and sleep. They may also discuss important topics such as family planning, reproductive health, and mental health. These visits are an opportunity to ask questions, clarify concerns, and receive tailored recommendations to improve or maintain your health.
Changes to Healthcare Classification System for 2025
As healthcare regulations evolve, updates to the system used to categorize medical services are implemented regularly. These changes can have a significant impact on the way healthcare providers document, bill, and receive reimbursement for services rendered. In 2025, several updates will affect the classification of preventive services, particularly those related to routine check-ups and screenings. It is important for healthcare professionals to stay informed about these adjustments to ensure compliance and accurate billing practices.
Key Modifications in Service Classifications
The new guidelines introduced in 2025 aim to streamline the classification process, making it easier for both providers and insurers to manage claims. Some of the key changes include:
- New categories for preventive screenings based on age and risk factors
- Revised definitions for routine health assessments
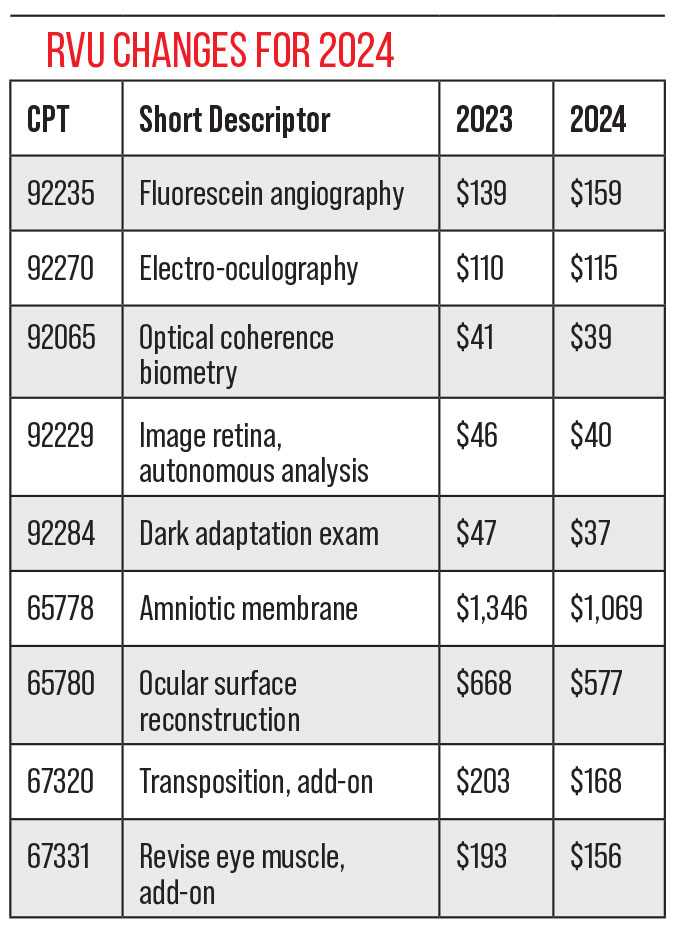
- Updated reimbursement rates for certain services
- Introduction of new billing protocols for telehealth services
Impact on Healthcare Providers and Insurance Companies
These updates are designed to improve accuracy in billing and ensure that patients receive the right care at the right time. Healthcare providers must carefully review the new classification system to ensure that all preventive services are properly documented and billed. Insurance companies will also need to update their reimbursement processes to reflect the new changes, which may result in more efficient claims processing and reduced administrative delays.
Staying informed about these modifications will help healthcare professionals avoid common mistakes and ensure they are reimbursed accurately for the services they provide. It also highlights the importance of ongoing education and training for medical staff to maintain compliance with evolving healthcare standards.
How to Find the Correct Healthcare Classification
Identifying the appropriate classification for a medical service is crucial to ensure proper billing and reimbursement. A precise and accurate classification ensures that healthcare providers are compensated for their work and that patients receive the correct services as intended. With so many services and treatments available, it is important to have a reliable method for finding the correct classification for each procedure.
To find the right classification, healthcare providers can use a variety of resources. The most common approach is to consult the updated medical classification manual or database. These resources are organized to help professionals locate the appropriate categories based on the type of service provided, patient demographics, and the specific healthcare needs addressed during the visit.
Additionally, healthcare providers can rely on online tools and software that allow for easy search and selection of the proper categories. Many of these tools provide detailed descriptions of each service, helping to ensure that all relevant factors are considered when assigning a classification. Keeping up with the latest updates in the system is essential for avoiding errors and ensuring smooth billing processes.
Coding for Preventive Healthcare Services
Accurate documentation of preventive healthcare services is essential for both effective care delivery and proper reimbursement. These services, which aim to detect health issues early and promote overall well-being, must be classified correctly to ensure healthcare providers are paid for their efforts. The process involves selecting the right categories from a comprehensive classification system that reflects the nature of the service provided.
Preventive services often include routine health assessments, screenings for various conditions, immunizations, and counseling on lifestyle factors. To properly classify these services, healthcare providers must understand the specific criteria and requirements for each type of care offered. This ensures that each procedure is accurately reflected in the system, reducing the chances of errors or claim denials.
In addition to ensuring proper compensation, coding also supports data collection for health trends and outcomes. By using a standardized system, it is easier for healthcare organizations to track the delivery of preventive services and assess their effectiveness. This helps improve healthcare quality and identify areas where more attention may be needed to improve patient health.
The Role of Insurance in Preventive Health Check-ups
Insurance plays a vital role in ensuring that individuals have access to essential health services, including preventive care. These policies are designed to cover a range of services aimed at maintaining good health and detecting potential issues early. By covering preventive care, insurance plans make it more affordable for individuals to access regular check-ups, screenings, and other necessary services.
Insurance coverage for preventive services can vary widely depending on the plan, but most major policies are required by law to cover certain screenings and routine assessments at no cost to the patient. This can include screenings for conditions like breast cancer, cervical cancer, and other chronic diseases, as well as immunizations and health counseling. The goal is to reduce long-term healthcare costs by addressing issues before they become serious or costly to treat.
Additionally, insurance providers may have specific guidelines or restrictions about which services are covered under different circumstances, such as age, risk factors, or family history. It is essential for patients to understand their insurance policy details, including the specific benefits for preventive care, to avoid unexpected costs or gaps in coverage. Being well-informed allows individuals to make the most of their health insurance benefits and prioritize their well-being effectively.
Impact of Healthcare Classification on Reimbursement
The classification used to categorize medical services directly influences how healthcare providers are reimbursed by insurance companies. When services are documented and categorized accurately, it ensures that providers receive proper compensation for the care they deliver. Inaccurate or incomplete classifications can lead to delayed payments, claim denials, or even reduced reimbursement rates, creating financial strain on healthcare practices.
The correct categorization is essential for ensuring that insurers understand the specific nature of the service provided. This process affects not only reimbursement rates but also compliance with regulations and insurance contracts. If the service is classified inappropriately, providers may face challenges in getting paid for their work or may have to go through lengthy appeal processes.
In addition, insurance policies often have specific criteria for coverage based on the service type, and using the correct classification helps providers ensure that the care delivered falls within those covered services. This has a significant impact on the efficiency of the claims process and the financial stability of healthcare providers, making it critical for medical practices to stay up to date with classification guidelines and billing practices.
Common Mistakes in Healthcare Classification
Proper classification of medical services is essential for accurate billing and reimbursement, but there are several common errors that healthcare providers often make. These mistakes can lead to delayed payments, claim denials, and even legal complications. Understanding and avoiding these common errors can help ensure smoother operations for medical practices and prevent unnecessary administrative challenges.
Incorrect Service Selection
One of the most frequent mistakes is selecting the wrong classification for the service provided. This can happen when a healthcare provider misinterprets the details of the procedure or uses outdated information. Incorrect service selection can result in improper billing, and insurers may reject the claim, leading to delays in payment.
Missing Documentation
Another common error is failing to document the service properly. Without clear and detailed documentation, it becomes difficult to prove the nature of the service or procedure performed. This oversight can cause claims to be rejected or underpaid, as insurance companies require precise information to process reimbursements accurately.
| Common Mistake | Consequence | Prevention |
|---|---|---|
| Incorrect Service Selection | Claim denials or underpayment | Stay updated with classification guidelines and use accurate resources |
| Missing Documentation | Claim rejection or delayed payment | Ensure complete and clear documentation for all services |
| Use of Outdated Classifications | Claims returned due to incorrect or obsolete information | Regularly review and update classification information |
By recognizing these common mistakes and taking the necessary steps to prevent them, healthcare providers can improve their billing processes, ensure proper reimbursement, and maintain positive relationships with insurers.
How Accurate Classification Improves Patient Care
Accurate classification of healthcare services is essential not only for the administrative side of healthcare but also for ensuring the best possible care for patients. Properly documenting and categorizing medical procedures helps healthcare providers deliver the most appropriate treatment while also ensuring that patients receive timely and effective follow-up care. Accurate records help avoid errors, reduce the chances of misdiagnosis, and ensure that necessary treatments and screenings are not overlooked.
When medical services are correctly classified, it allows healthcare providers to access the relevant patient history and understand the full scope of the patient’s needs. This comprehensive understanding enhances decision-making, allowing providers to offer tailored treatment plans that address both current and potential future health concerns. Furthermore, it helps to avoid unnecessary procedures, reducing the risk of complications, over-treatment, and patient dissatisfaction.
Accurate classifications also improve communication between healthcare providers, insurance companies, and patients, creating a smoother and more transparent process for all parties. This transparency leads to better coordination of care, quicker reimbursements, and more effective management of healthcare services. Ultimately, the result is better patient outcomes and a more efficient healthcare system.
The Role of Providers in Correct Classification
Healthcare providers play a critical role in ensuring that medical services are properly categorized and documented. The accuracy of service classifications directly impacts the efficiency of healthcare operations, patient care, and reimbursement processes. Providers are responsible for selecting the right categories based on the services rendered and providing clear, complete documentation to support these choices.
Providers’ attention to detail when documenting patient encounters is essential for minimizing errors. When healthcare professionals correctly identify and classify services, it leads to a smoother billing process, more accurate patient records, and better communication with insurance companies. This accuracy helps prevent delays in reimbursement and reduces the likelihood of claims being denied.
- Accurate Diagnosis: Providers must ensure that diagnoses are correctly recorded and linked to the appropriate services.
- Clear Documentation: Comprehensive and detailed records are crucial to supporting service classifications and preventing misunderstandings or errors.
- Up-to-Date Knowledge: Staying current with healthcare classification standards and guidelines is vital for providers to avoid outdated practices.
- Collaborative Communication: Effective communication between providers and administrative staff ensures accurate service categorization.
By fulfilling these responsibilities, healthcare providers not only ensure financial stability for their practice but also contribute to improved patient care and outcomes. Their role in accurate documentation and service classification is vital to the healthcare system’s overall efficiency and effectiveness.
Exploring Modifiers for 2025
Modifiers are essential tools in medical classification that provide additional context or clarification regarding the services provided. They help adjust the classification of healthcare services to ensure that billing reflects the specific circumstances surrounding a procedure. By using modifiers appropriately, healthcare providers can communicate more accurately with insurers and improve the overall efficiency of the billing process.
Modifiers help to specify particular details about a service, such as whether it was performed under special circumstances or if it was altered in some way. They ensure that the final classification reflects the true nature of the service, thereby reducing the risk of errors or delays in the reimbursement process. These adjustments are especially important in complex or unique cases where standard classifications may not fully capture the scope of care provided.
Types of Modifiers
There are several categories of modifiers, each designed to address specific needs. Some of the most common include:
- Anesthesia Modifiers: Indicate special considerations during the administration of anesthesia.
- Service Modifiers: Used to report services that were altered in terms of time, intensity, or complexity.
- Procedure Modifiers: Help distinguish between different types of procedures that may appear similar.
- Billing Modifiers: Clarify billing requirements, such as co-payments or shared services.
Why Modifiers Matter

Using the correct modifier ensures that healthcare providers receive the appropriate reimbursement for the services they deliver. Incorrect use of modifiers can lead to denials, delays, or even audits, making it essential for healthcare providers to stay updated on the most recent standards and guidelines. By correctly applying modifiers, providers not only streamline the billing process but also ensure they are compensated fairly for the care they deliver.
How to Handle Billing Disputes
Disputes over healthcare charges can arise for various reasons, from misunderstandings about what services were provided to issues with the classification of procedures. It’s essential to approach these situations systematically to ensure that both parties–providers and patients–reach a fair resolution. By understanding the root cause of the dispute and following a structured approach, healthcare providers can manage billing disagreements effectively and maintain positive relationships with their patients and insurers.
When a billing issue arises, the first step is to carefully review the claim in question. This helps to identify any discrepancies between what was provided and what was billed. It’s also important to consider the details that may have led to the issue, such as incorrect service classifications, misunderstandings regarding covered services, or errors in the insurance verification process.
Steps to Resolve Billing Issues
There are several steps that healthcare providers and their patients can take to resolve billing disputes:
- Review the Bill Thoroughly: Ensure that the charges align with the services provided. Compare the bill with any records or documentation from the appointment.
- Clarify the Issue: Understand whether the issue is with the classification, insurance coverage, or a billing error. If needed, contact the insurance provider for clarification.
- Contact the Insurance Company: If the dispute involves an insurance claim, reach out to the insurer for an explanation of the charges or denial. Sometimes additional information or documentation can resolve the issue.
- Appeal the Decision: If the dispute remains unresolved, the next step is to file an appeal with the insurance company or billing department. Provide clear, documented evidence to support your case.
- Negotiate Payment Terms: If the issue is related to an outstanding balance, negotiate a payment plan that is manageable for the patient while ensuring fair compensation for services provided.
Preventing Future Disputes

To reduce the likelihood of billing disputes, healthcare providers can take proactive steps, including:
- Clear Communication: Discuss billing procedures and potential costs with patients upfront to avoid misunderstandings later.
- Accurate Documentation: Ensure that all services provided are well-documented and accurately classified to avoid confusion.
- Training and Education: Regularly train staff on the latest billing practices and guidelines to ensure compliance and accuracy.
By following these steps and maintaining open communication, healthcare providers can minimize the impact of billing disputes, ensuring timely payments and positive relationships with both patients and insurers.
Future Trends in Preventive Health Coding
The field of preventive healthcare is undergoing significant transformation as the healthcare system evolves to meet the demands of an aging population, advances in medical technology, and changes in public health priorities. As these shifts occur, the way health services are categorized and billed is also changing. The future of healthcare coding, particularly in the area of preventive care, will likely focus on more accurate, efficient, and patient-centric approaches. This section explores some of the key trends that will shape how preventive health services are documented, classified, and reimbursed in the coming years.
One of the biggest trends is the increased use of data-driven tools and technologies. These tools aim to streamline the documentation process, ensuring that healthcare providers can capture all relevant information efficiently. With advancements in electronic health records (EHR) and other technologies, the use of automated coding systems is expected to grow, helping to reduce errors and improve the accuracy of health service classifications. Additionally, a shift towards value-based care is expected to change the way preventive care services are evaluated and reimbursed, placing a greater emphasis on patient outcomes rather than the volume of services delivered.
Key Trends in Preventive Healthcare Classification
Several key trends are expected to define the future of preventive care documentation:
- Integration of Artificial Intelligence (AI): AI is set to play a major role in healthcare coding, helping to automatically classify services based on patient data. AI-driven solutions will likely improve accuracy and speed, reducing human errors in the documentation process.
- Emphasis on Preventive Care and Wellness: As the healthcare system shifts towards preventative care, there will be more focus on documenting services that focus on health maintenance and disease prevention, ensuring that these services are reimbursed appropriately.
- Patient-Reported Data: The increasing use of patient-reported data, such as information gathered through wearable health devices or patient surveys, will become more integral in preventive health coding. This data may help create a more comprehensive and accurate picture of a patient’s health status.
- Personalized Healthcare: With the rise of precision medicine, coding systems will likely evolve to accommodate individualized health plans, making it easier to capture tailored preventive services that reflect each patient’s unique needs.
The Role of Technology and Automation
Technology and automation will undoubtedly play a central role in the future of preventive health coding. The development of advanced tools will likely make it easier for healthcare providers to manage patient records, track preventive health services, and ensure that all relevant services are accurately documented and billed. Below is a table outlining some of the emerging technologies that are expected to impact the future of preventive care documentation:
| Technology | Impact on Preventive Care Coding |
|---|---|
| Artificial Intelligence (AI) | Improves the accuracy and speed of service classification by automatically analyzing patient data and recommending appropriate codes. |
| Electronic Health Records (EHR) | Streamlines the documentation process, making it easier to capture relevant health data and ensure compliance with coding standards. |
| Patient-Reported Data Systems | Helps providers capture additional information from patients, leading to more accurate health profiles and better documentation of preventive services. |
| Wearable Health Devices | Provides continuous, real-time health data that can inform personalized preventive care plans and improve the accuracy of health service classifications. |
As these technologies become more integrated into healthcare systems, they will drive the evolution of preventive health coding, making it more efficient, accurate, and patient-focused.