Providing immediate assistance to young individuals in critical situations requires a combination of knowledge, quick thinking, and the ability to follow established protocols. Understanding the necessary steps to handle emergencies effectively can make a significant difference in outcomes.
This guide offers a comprehensive overview of key practices and strategies for those preparing to evaluate their readiness in this area. By exploring essential techniques and reviewing real-world applications, caregivers and professionals can enhance their skills and confidence.
From addressing respiratory challenges to managing circulatory issues, the following sections cover the fundamental principles of care. Through careful preparation and study, individuals can ensure they are well-equipped to handle the most pressing needs of young patients.
Understanding Pediatric Emergency Care Protocols
Providing critical assistance to young individuals during urgent medical situations requires a thorough understanding of structured approaches. These guidelines ensure timely and effective actions to stabilize the patient and prevent further complications.
Key Elements of Emergency Protocols
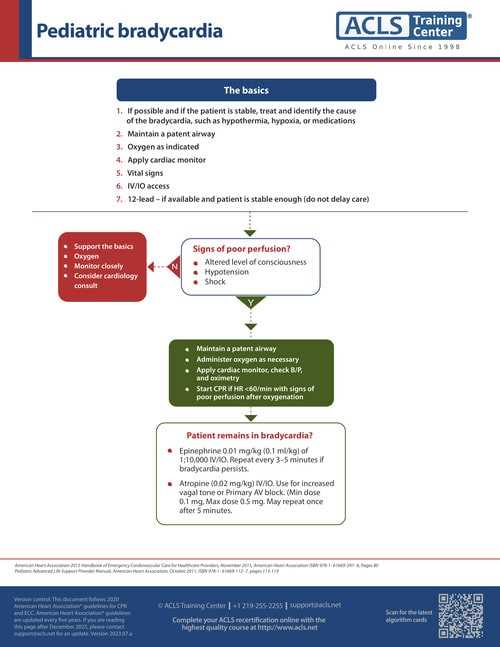
Emergency protocols are built around a series of prioritized steps that address the most immediate threats to health. These include maintaining proper airflow, monitoring circulation, and quickly identifying signs of distress. Each step is designed to ensure a seamless response that minimizes risks.
The Importance of Preparedness and Training
Effective execution of these procedures relies heavily on proper training and readiness. Caregivers and responders must not only familiarize themselves with theoretical knowledge but also engage in practical exercises to reinforce their ability to act under pressure. This combination of preparation and practice is crucial for ensuring successful outcomes in urgent scenarios.
Key Principles of Advanced Pediatric Support
Managing critical situations involving young individuals requires a structured approach centered on maintaining vital functions and addressing urgent health concerns effectively. These core principles guide responders in delivering timely and coordinated care.
- Immediate Assessment: Quickly evaluating the condition to identify priority actions, such as ensuring breathing and circulation, is fundamental to effective intervention.
- Systematic Approach: Following a step-by-step method helps minimize errors and ensures no critical aspect is overlooked during care.
- Communication and Coordination: Clear interaction among team members ensures smooth execution of procedures and enhances overall efficiency.
- Continuous Monitoring: Regularly observing changes in condition allows for prompt adjustments to the treatment plan.
These principles are complemented by proper training and an understanding of the unique physiological needs of younger individuals. Practicing these methods builds confidence and prepares caregivers for effective real-world application.
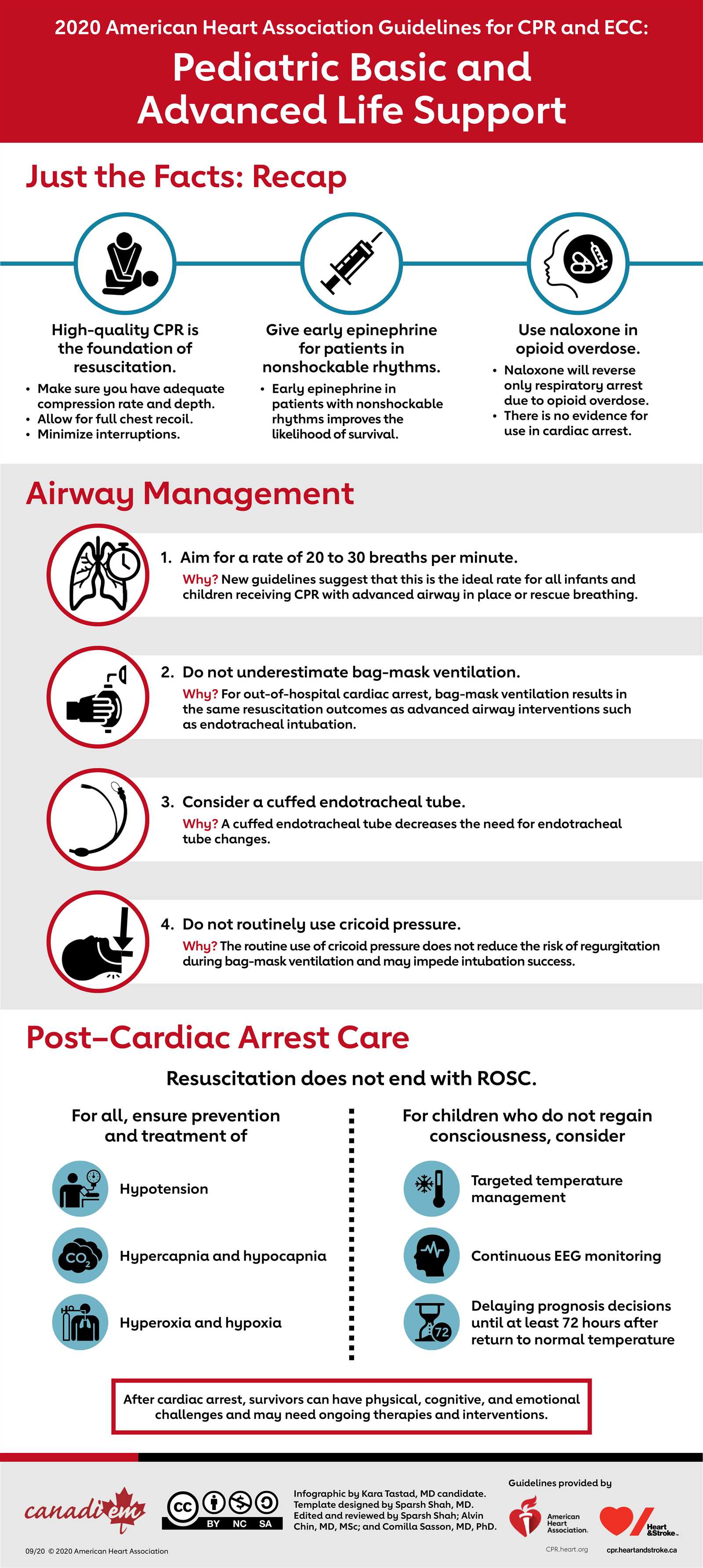
Effective Techniques for Pediatric Resuscitation
Reviving young individuals during critical health episodes requires a precise approach focused on restoring essential functions. Employing proven methods ensures the best chance of stabilization and recovery in urgent situations.
- Airway Management: Ensuring the passage for airflow is open and unobstructed is the first step in restoring normal breathing. Techniques include careful positioning and, if necessary, the use of tools like masks or tubes.
- Chest Compressions: Delivering rhythmic pressure to the chest helps maintain blood flow to vital organs when the heart’s activity is compromised.
- Ventilation Assistance: Providing oxygen manually or through devices supports individuals who cannot breathe effectively on their own.
- Use of Specialized Equipment: Devices like defibrillators may be employed to address irregular heart rhythms, following recommended protocols.
Mastery of these techniques comes from a combination of study, hands-on practice, and staying updated with the latest guidelines. Responders trained in these methods can act decisively and improve outcomes significantly during emergencies.
Critical Interventions for Respiratory Emergencies
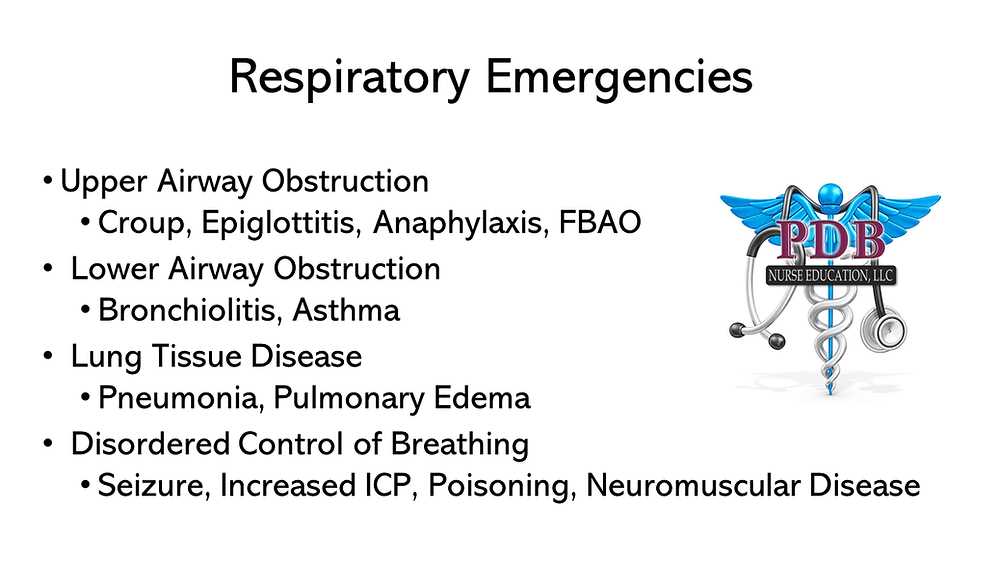
Addressing breathing difficulties in young individuals demands prompt and effective measures to restore adequate oxygen levels and prevent further complications. Recognizing the signs and applying targeted techniques are vital in managing these urgent situations.
Immediate Steps to Stabilize Breathing
The first priority is to ensure the airway is unobstructed. Gently adjusting the head and neck can help open the passage, while suction may be used to clear any blockages. Supplemental oxygen delivery is often required to improve oxygenation levels.
Tools and Techniques for Severe Cases
For more critical scenarios, advanced methods may be necessary. These include the use of ventilation devices like bag-valve masks to assist with breathing. In extreme cases, inserting airway tubes ensures continuous airflow, while monitoring devices track oxygen levels and guide interventions.
Proficiency in these techniques, combined with the ability to assess the severity of the situation quickly, enables caregivers to act decisively and improve outcomes for individuals facing respiratory challenges.
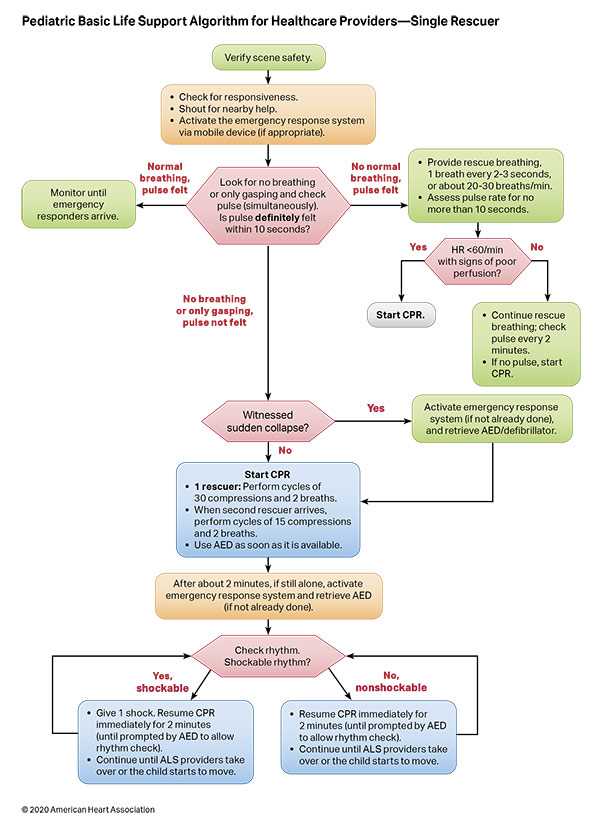
Step-by-Step Guide to Cardiopulmonary Support
Restoring heart and lung function during emergencies involves a structured process designed to address immediate threats while stabilizing vital systems. Following a clear sequence of actions ensures efficient and effective intervention.
Key Phases of the Process
The approach to managing these critical situations includes assessing the individual’s condition, initiating circulation and breathing support, and using equipment as needed to sustain essential functions.
Essential Techniques and Timing
| Step | Action | Purpose |
|---|---|---|
| 1 | Check responsiveness and breathing | Determine if immediate intervention is needed |
| 2 | Start chest compressions | Maintain blood flow to vital organs |
| 3 | Deliver rescue breaths | Provide oxygen to the lungs |
| 4 | Use defibrillator if required | Restore normal heart rhythm |
Adhering to this sequence and ensuring consistent application of these techniques can significantly improve outcomes during critical situations involving heart and lung function challenges.
Essential Medications for Pediatric Life Support
When managing critical situations involving young patients, medications play a key role in stabilizing vital functions and preventing further complications. The correct drugs, administered promptly, can significantly impact outcomes in emergencies.
Commonly Used Medications

The following medications are frequently used in emergencies to address specific concerns such as heart function, respiratory distress, or other urgent conditions:
- Adrenaline: Used to stimulate the heart and improve circulation during cardiac arrest or severe hypotension.
- Aminophylline: Helps open airways in cases of severe asthma or wheezing, improving breathing.
- Lidocaine: A local anesthetic and antiarrhythmic, used in situations of irregular heart rhythms.
- Dextrose: Administered in cases of hypoglycemia to raise blood sugar levels quickly.
Important Considerations for Medication Administration
It’s crucial to administer the right dose based on the individual’s age, weight, and medical history. Additionally, ensuring timely delivery of medications can greatly enhance recovery chances and reduce the risks of further complications.
Best Practices for Airway Management in Children
Ensuring that a young patient’s airway is clear and unobstructed is crucial in emergency situations. Effective management requires a blend of techniques that focus on maintaining open airways, promoting adequate oxygen flow, and minimizing complications.
Initial Assessment and Interventions
The first step in managing an airway is a thorough assessment of the child’s breathing status. If the child is not breathing or has a compromised airway, immediate action is required. The following methods can help establish a clear path for air:
- Head-Tilt Chin-Lift: A simple maneuver to open the airway in an unconscious child by tilting the head back and lifting the chin.
- Jaw-Thrust Maneuver: Used when a neck injury is suspected to avoid further spinal damage, this technique lifts the jaw without moving the head.
- Suction: If there is visible obstruction, suctioning the airway can clear mucus, vomit, or foreign objects, allowing for better airflow.
Advanced Airway Techniques
If basic methods are insufficient or if the situation worsens, more advanced techniques may be necessary. These methods ensure that the airway remains open and functional for sustained breathing:
- Endotracheal Intubation: Insertion of a tube into the trachea to ensure continuous airflow, especially in cases of severe respiratory distress.
- Oropharyngeal and Nasopharyngeal Airways: These devices can be inserted to keep the airway open if the child is unconscious but has no risk of injury to the mouth or nose.
Proper training and timely intervention are vital to prevent airway compromise and ensure the child’s oxygen supply is maintained during critical moments.
Recognizing Early Signs of Pediatric Distress
Identifying the early signs of distress in children is critical for effective intervention and ensuring their well-being. Recognizing subtle changes in behavior, appearance, and physiological responses can help caregivers and medical professionals act promptly and prevent more severe complications.
Some of the initial indicators of distress in children may include changes in their breathing patterns, such as rapid or labored respiration, as well as alterations in skin color, like paleness or a bluish tint around the lips or extremities. It is also important to observe their level of alertness, as confusion, drowsiness, or irritability may indicate underlying issues.
Additional signs to look out for are sudden weakness or difficulty in movement, particularly when the child is unable to sit up or stand without assistance. Behavioral shifts, such as crying more than usual or becoming unusually quiet, can also suggest that the child is in discomfort or pain. Early detection of these symptoms allows for more effective treatment and reduces the risk of severe health crises.
Preparing for Pediatric Emergency Scenarios
Effective preparation for critical situations involving children requires a well-thought-out approach to both knowledge and action. Understanding the potential challenges and acquiring the necessary skills can make all the difference in managing an emergency. It’s important to familiarize oneself with specific protocols and practice responding quickly and efficiently to various medical emergencies that children may experience.
Preparation involves not only having the right tools and equipment ready but also ensuring that all involved parties, from caregivers to healthcare providers, are well-versed in essential techniques and procedures. Simulation exercises and regular training can help reinforce the critical steps needed to address a child’s health crisis promptly and with confidence.
Building a Strong Foundation of Knowledge
Having a solid understanding of common emergency scenarios, such as choking, respiratory distress, or severe allergic reactions, is key to handling these situations with clarity. Knowing when and how to intervene can prevent complications and provide immediate relief until further medical assistance arrives.
Creating an Organized Response Plan
An organized response plan is vital in ensuring the quick mobilization of resources. This plan should outline key steps, such as assessing the situation, administering first aid, and coordinating with emergency services. Ensuring that all caregivers and professionals are aware of these steps will help streamline the process and reduce the chances of delays during critical moments.
Life-Saving Tips for Cardiac Arrest in Kids
When a child experiences cardiac arrest, swift and efficient action is crucial for survival. The immediate response from caregivers and healthcare providers can significantly increase the chances of a positive outcome. Knowing what steps to take during such an emergency is essential to minimize the time the child spends without a pulse, which can greatly reduce the risk of permanent damage.
The first step in managing a cardiac arrest situation is recognizing the signs and acting without hesitation. Children may suddenly lose consciousness, stop breathing, or exhibit abnormal heart rhythms. Recognizing these symptoms early allows for timely interventions, which are essential for improving outcomes.
Immediate Actions for Resuscitation
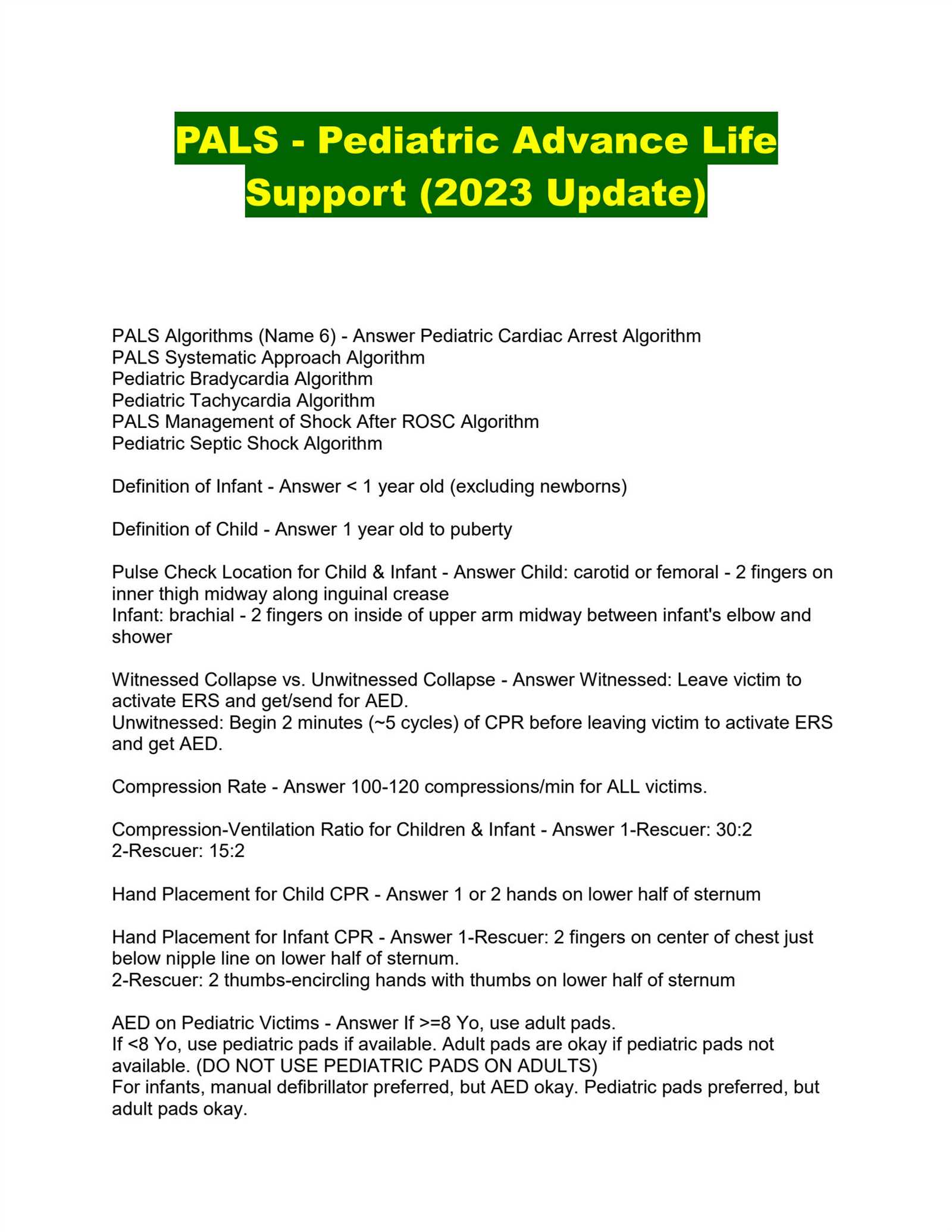
When cardiac arrest is suspected, performing chest compressions and starting CPR as quickly as possible is the most critical intervention. Place the heel of one hand on the child’s chest, just below the nipple line, and use the other hand to compress the chest at least one-third of the chest depth. Compressions should be given at a rate of 100-120 per minute, with minimal interruptions.
Using Defibrillation if Available
If a defibrillator is available, it should be used as soon as possible. Defibrillation can reset the heart’s rhythm and restore normal circulation. When using an automated external defibrillator (AED), it will provide voice prompts to guide you through the process, ensuring it is as simple as possible to follow in an emergency.
Common Challenges in Pediatric Life Support
Providing emergency care for young patients comes with unique challenges that differ from those faced in treating adults. Children’s smaller body sizes, varying anatomy, and the emotional and psychological aspects of treating minors require special attention and adaptability. Medical professionals must navigate these challenges to provide the best care during critical situations.
One of the most significant challenges in these scenarios is the difficulty in assessing the child’s condition accurately. Due to their limited ability to communicate, children may not be able to express symptoms, making it harder to diagnose the underlying problem quickly. This requires healthcare providers to be especially vigilant and rely on physical signs, history, and observation.
Additionally, the proper use of equipment and medications is another common challenge. Many medical devices and drugs are designed for adult bodies, so adjusting them for younger patients requires knowledge of pediatric dosages and sizes. Miscalculations or improper application can lead to serious complications.
Finally, the emotional stress of treating young patients is often compounded by the anxiety of parents or guardians. Managing the emotional needs of the family while ensuring effective care is a delicate balance that requires both technical expertise and strong communication skills.
Insights into Shock Management in Pediatrics
When it comes to managing shock in young patients, timely intervention is critical for ensuring the best possible outcome. Shock, a life-threatening condition where the body’s tissues and organs do not receive enough blood flow, requires immediate recognition and treatment. Children’s unique physiological characteristics make them more vulnerable to this condition, and understanding the nuances of care is essential for healthcare professionals working in emergency settings.
One of the first steps in managing shock in children is recognizing the signs early. Symptoms may vary depending on the type of shock, but general indicators include pale skin, rapid breathing, weak pulse, and altered mental status. It is important to understand that children may not always exhibit these signs as strongly as adults, and even subtle changes in behavior or appearance should be taken seriously.
The management approach includes stabilizing the patient by addressing the underlying cause of shock. Fluid resuscitation, for example, plays a major role in restoring circulatory volume and supporting organ function. However, in certain cases, medications such as inotropes or vasopressors may be necessary to help improve cardiac output and blood pressure. Each treatment plan should be tailored based on the child’s age, weight, and the specific type of shock.
Furthermore, ongoing monitoring and adjustments to the treatment plan are crucial. As the child responds to interventions, healthcare providers must assess the effectiveness of the therapies and be prepared to make necessary changes quickly. The overall goal is to prevent further organ damage and optimize the chances of recovery.
Vital Equipment for Pediatric Emergency Care
In emergency situations involving young patients, having the right tools and devices on hand can make a crucial difference in outcomes. Ensuring that healthcare professionals are equipped with the proper equipment helps facilitate quick and effective treatment, particularly in urgent scenarios. This collection of tools must be specifically tailored to the needs of children, who require different considerations than adults due to their smaller size and unique physiological characteristics.
One of the most essential pieces of equipment is the pediatric-sized airway management tools. These include appropriately sized endotracheal tubes, laryngoscopes, and airway adjuncts. Correct sizing is critical to ensuring effective ventilation and oxygenation, as improperly sized devices can cause harm or fail to function properly.
Another vital tool is the defibrillator with pediatric capability. Devices designed for adults are not suitable for children due to the difference in body size and electrical resistance. Pediatric defibrillators allow for lower energy doses, minimizing the risk of injury while maximizing the chances of restarting the heart in cases of cardiac arrest.
Additionally, equipment for intravenous access and fluid administration is crucial. This includes pediatric IV catheters, syringes, and infusion pumps, which help in the safe and accurate delivery of fluids and medications. It is also important to have specialized monitoring devices, such as pulse oximeters and blood pressure cuffs designed for younger patients, to provide continuous feedback on their vital signs.
Finally, appropriate transport equipment, such as pediatric-sized stretchers, oxygen delivery systems, and immobilization devices, ensures that children can be safely moved between care settings. All of these tools must be regularly maintained, inspected, and stored in an easily accessible manner to ensure rapid response when needed.
How to Assess Pediatric Heart Rhythms
Evaluating heart rhythms in young patients is crucial for detecting underlying conditions that may require immediate intervention. Accurate assessment involves observing both the rate and pattern of heartbeats, which can indicate the presence of abnormalities. It is essential to use age-appropriate methods and tools to properly evaluate the rhythm and identify any irregularities that may need treatment or further investigation.
Step 1: Initial Observation and Palpation
Start by observing the child’s general condition, looking for signs of distress or discomfort, such as difficulty breathing, fainting, or cyanosis. Palpating the pulse is the first step in evaluating the rhythm, especially in children. The radial or brachial pulse should be checked, and the rhythm should be felt for consistency. A normal pulse should have a regular and rhythmic beat. Any irregularity, such as skipped beats or extra beats, should be noted.
Step 2: Electrocardiogram (ECG) Monitoring
If the initial palpation suggests an abnormal rhythm, further assessment through an electrocardiogram (ECG) is essential. An ECG provides a visual representation of the electrical activity of the heart, allowing for detailed analysis of heart rate, rhythm, and any irregularities. Proper electrode placement is crucial to obtain an accurate reading. In children, special care should be taken to ensure the leads are placed in the correct positions, as anatomical differences can affect readings.
Interpretation of the ECG will help identify common arrhythmias such as atrial fibrillation, ventricular tachycardia, or bradycardia. Based on the findings, healthcare providers can take appropriate actions, including medication, electrical interventions, or referral to a pediatric cardiologist for further evaluation.
Importance of Teamwork in Emergency Pediatric Care
In critical situations, the ability to work cohesively as a team can make the difference between a positive or negative outcome. Emergency care for young patients requires clear communication, collaboration, and rapid decision-making. Each team member must contribute their specialized skills and knowledge, working in unison to provide the best possible care under high-pressure circumstances.
Effective teamwork involves coordinated actions where roles and responsibilities are clearly defined, yet flexible enough to adapt to the dynamic nature of emergencies. This collaborative approach reduces the risk of errors and ensures timely intervention, which is especially vital when treating children who may not be able to communicate their symptoms as clearly as adults.
In addition, having a well-trained and synchronized team allows for efficient use of resources, reduces stress among healthcare providers, and ultimately improves patient outcomes. Whether it is managing airways, administering medication, or performing life-saving procedures, the collective effort and quick thinking of all involved professionals are critical in optimizing the care provided.
Differences Between Adult and Pediatric Care
When providing medical care, there are significant differences between treating adults and children. These differences stem from variations in anatomy, physiology, and the way children respond to illness or injury. Healthcare professionals must adapt their approach to accommodate the unique needs of younger patients, ensuring the best possible outcome in each situation.
Anatomical and Physiological Variations
One of the key differences lies in the anatomy and physiology of children. For example, children’s airways are smaller and more delicate than those of adults, which can make airway management more challenging. Additionally, a child’s heart rate and respiratory rate are typically higher than those of an adult, requiring different monitoring and intervention techniques. Their body mass, fluid composition, and metabolic rates also differ, influencing how medications are absorbed and processed.
Emotional and Developmental Considerations
Another significant difference is the emotional and developmental aspect of care. Children may not be able to fully comprehend the situation or communicate their discomfort effectively. This requires healthcare providers to be more attuned to non-verbal cues and to use child-friendly communication methods. Establishing trust and comfort is crucial, as fear or anxiety can exacerbate physical symptoms. Family involvement is also often more critical in pediatric care, as parents or caregivers play an essential role in the child’s recovery process.
Reviewing Case Studies in Pediatric Life Support
Analyzing real-world examples is an essential method for understanding the complexities of treating young patients in critical situations. Case studies provide invaluable insights into the challenges and approaches involved in managing emergencies, offering opportunities to reflect on decision-making processes and outcomes. These case studies highlight both successful interventions and areas where improvements can be made, serving as a learning tool for healthcare professionals.
Case Study 1: Respiratory Distress in a Child
This case study focuses on a child presenting with severe respiratory distress. Early signs of distress were noted, and the medical team quickly initiated the appropriate interventions. The analysis of the case highlights the importance of early recognition and the step-by-step management that led to a positive outcome. Key lessons learned from this case include the significance of airway management techniques and timely medication administration.
Case Study 2: Cardiac Arrest in a Young Patient
This scenario involves a sudden cardiac arrest in a young patient. The case study details the critical moments following the event, with the medical team performing immediate chest compressions and administering emergency medications. This case emphasizes the importance of rapid response, effective teamwork, and the use of appropriate resuscitation techniques. The successful recovery of the child underscores the significance of efficient intervention in saving lives.
| Case Study | Key Interventions | Outcome |
|---|---|---|
| Respiratory Distress | Airway management, medication, oxygen therapy | Improved respiratory function, stable condition |
| Cardiac Arrest | Chest compressions, emergency medications, defibrillation | Successful resuscitation, full recovery |
Practical Tips for Passing Pediatric Care Tests

Successfully navigating assessments in the field of child healthcare requires a blend of knowledge, strategy, and preparation. Whether preparing for a written exam or a practical evaluation, there are certain steps that can increase your chances of success. The key lies in understanding the core principles, practicing regularly, and approaching the exam with a calm, focused mindset.
Key Preparation Strategies
- Review Core Concepts: Focus on the fundamental principles of child healthcare. Make sure you understand basic anatomy, emergency procedures, and common medical conditions.
- Practice with Mock Scenarios: Simulating real-life situations through mock scenarios can help you gain confidence and improve your practical skills.
- Study Group Sessions: Collaborating with peers allows for the exchange of knowledge and clarification of difficult topics.
- Stay Organized: Keep notes and study materials well-organized to make it easier to review important concepts efficiently.
Tips for the Exam Day

- Arrive Early: Getting to the exam location with time to spare will help you settle in and reduce anxiety.
- Read Questions Carefully: During the exam, take your time to thoroughly read each question or scenario before responding to ensure you don’t miss important details.
- Prioritize Tasks: If the exam includes practical components, tackle the most critical tasks first, such as airway management or CPR, before moving on to less urgent steps.
- Stay Calm: Remember to breathe and stay composed. Stress can hinder performance, so staying focused and calm is essential for success.