
When it comes to evaluating potential health risks, specialized screenings play a crucial role in detecting various harmful agents in the body. These evaluations help healthcare providers identify possible infections or conditions that might not be visible through physical symptoms alone. Understanding how these screenings work and what the results mean is essential for effective treatment and prevention.
Many individuals may feel uncertain about the outcomes of such assessments, wondering what the findings imply for their health. This section aims to clarify the process, explain common findings, and provide guidance on what steps to take next. Gaining clarity on the meaning behind these results can help you make informed decisions regarding your healthcare and any necessary treatments.
Blood Pathogens Test Answers
Understanding the results of diagnostic screenings that detect harmful microorganisms in the bloodstream can be complex. These screenings are designed to identify any potential threats that could affect your overall health, often before symptoms are visible. The results can vary depending on the type of infection or condition being investigated.
Once the results are in, it’s important to interpret them carefully. Positive findings indicate the presence of specific agents that may require immediate attention, while negative results typically suggest no harmful presence. However, even negative outcomes do not always guarantee complete safety, as some infections might not show up on the screening.
Knowing how to act on these results is crucial. If the findings indicate an infection, healthcare providers usually recommend a course of treatment. In some cases, further tests may be required to confirm or clarify the results. Understanding the next steps and how they impact your health is essential for effective management and prevention.
Understanding Blood Pathogen Testing
Screenings designed to detect harmful microorganisms in the circulatory system are crucial for identifying infections that may not yet show symptoms. These evaluations are typically used when a healthcare provider suspects that an individual may have been exposed to infectious agents that could compromise their health. The procedure is often quick and minimally invasive, providing valuable insights into the presence of unwanted organisms.
How the Screening Works
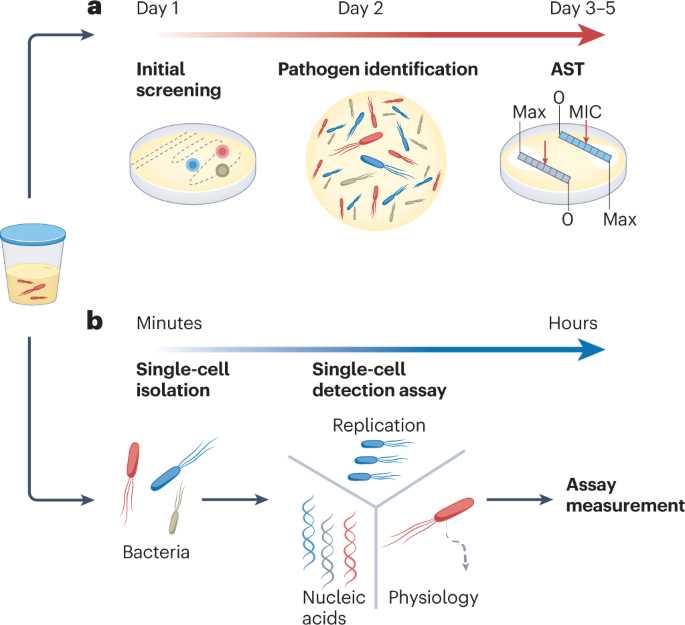
During the process, a small sample of blood is collected and analyzed for signs of harmful bacteria, viruses, or other microorganisms. Depending on the type of infection being investigated, different methods may be used to identify the specific agents. Results are typically available within a few days, and they can help healthcare providers determine the next steps in treatment or further investigation.
Why It’s Important
These screenings play a vital role in early detection. By identifying infections in their earliest stages, individuals are better equipped to receive the appropriate treatment before complications arise. Additionally, knowing the presence of certain organisms can help prevent the spread of infections to others. Early intervention is key in managing health risks and ensuring long-term wellness.
Common Blood Pathogens Detected in Tests
Various harmful microorganisms can circulate in the body, often without showing immediate symptoms. Infections caused by these agents are typically identified through specialized screenings, which help pinpoint the specific organisms responsible for health concerns. Understanding which types of infections are commonly detected in these evaluations is essential for both prevention and treatment.
Commonly Identified Microorganisms
There are several types of microorganisms that are frequently found in diagnostic evaluations. These include both bacterial and viral agents, each with different characteristics and potential health risks. The most common types identified include:
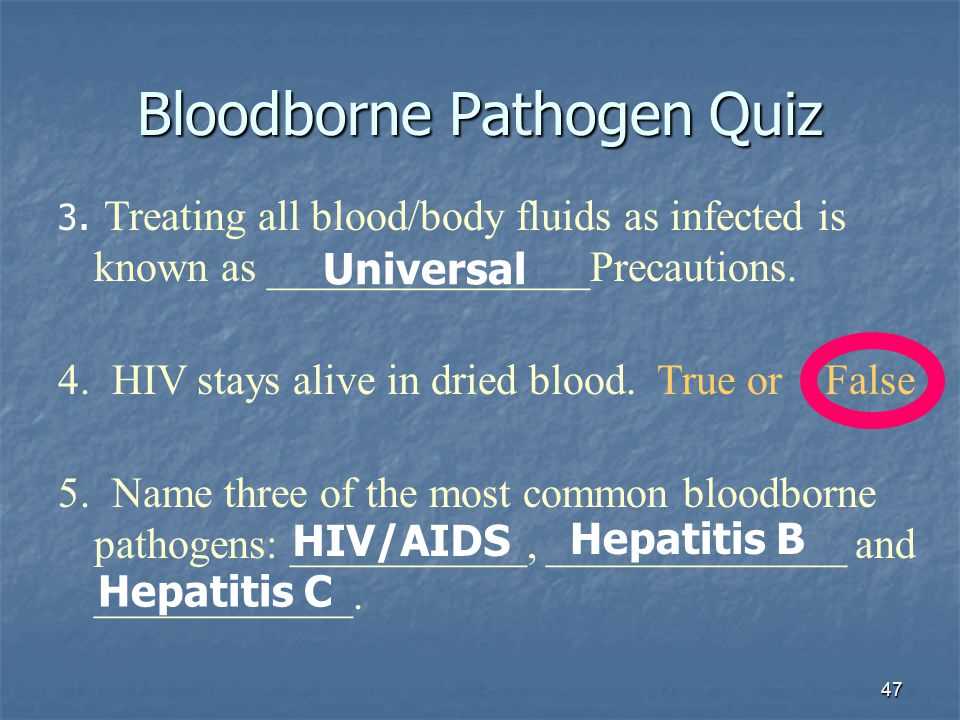
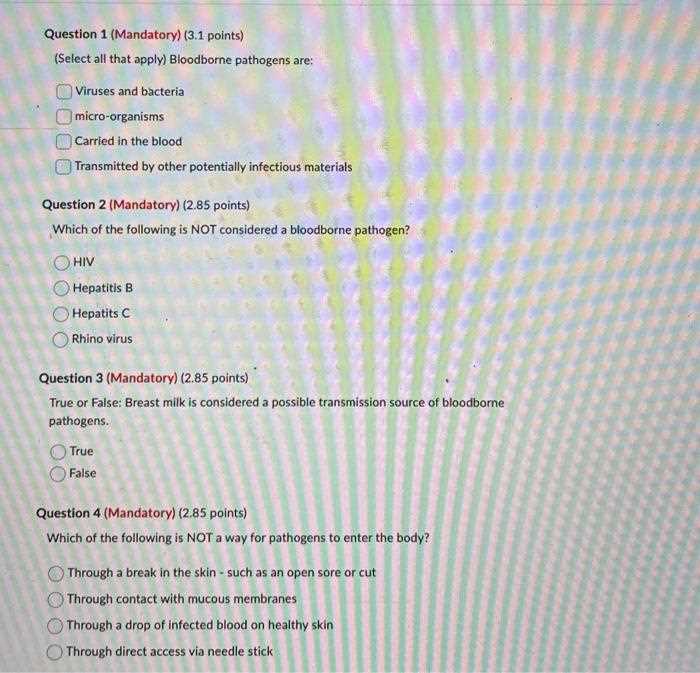
- HIV – A virus that attacks the immune system and can lead to acquired immunodeficiency syndrome (AIDS).
- Hepatitis B and C – Viruses that cause liver inflammation and can result in long-term damage if left untreated.
- Syphilis – A bacterial infection that progresses in stages if not treated, potentially affecting multiple organs.
- Malaria – A parasitic infection spread by mosquitoes, which can cause severe fever and organ damage.
- Sepsis – A serious condition caused by the body’s response to infection, often resulting in widespread inflammation.
Other Notable Infections
In addition to the most common organisms, certain less common but still significant infections may also be detected. These include:
- Lyme disease – A bacterial infection transmitted by ticks that can cause chronic symptoms if untreated.
- Tuberculosis (TB) – A bacterial infection that primarily affects the lungs but can spread to other organs.
- Chikungunya – A viral infection transmitted by mosquitoes, known for causing debilitating joint pain.
These microorganisms can have varying levels of severity, making early detection crucial for effective treatment and management. Depending on the findings, healthcare providers can recommend targeted therapies or further investigations to ensure the best possible outcomes.
How Blood Pathogen Tests Are Performed
Diagnostic evaluations designed to identify harmful microorganisms in the circulatory system typically involve a simple yet effective process. The main objective is to gather a sample that can be analyzed for the presence of infectious agents. The procedure itself is usually quick and minimally invasive, ensuring that healthcare professionals can obtain reliable results with minimal discomfort to the patient.
Step-by-Step Procedure
To begin, a healthcare provider will clean the skin and prepare the area where the sample will be taken, typically from a vein in the arm. A needle is then inserted to draw a small amount of blood, which is collected in a vial or syringe. In some cases, additional tests may require multiple samples. The procedure is generally brief, and most individuals experience only mild discomfort.
Laboratory Analysis
Once the sample is collected, it is sent to a laboratory where various methods are used to analyze the presence of harmful microorganisms. Depending on the type of infection being investigated, techniques such as PCR (Polymerase Chain Reaction), enzyme-linked immunosorbent assays (ELISA), or cultures may be used to identify specific agents. These methods can detect both the presence and the quantity of microorganisms in the sample.
After the analysis, the results are reviewed by medical professionals who will interpret the findings. Based on the outcome, the appropriate steps for treatment or further investigation are recommended. This process helps healthcare providers understand the underlying causes of symptoms and determine the most effective course of action for the patient.
What to Expect From Blood Test Results
After undergoing a diagnostic procedure to detect potential infections or harmful organisms in the body, it is natural to wonder what the results will indicate and how they will affect your health. Understanding the types of results you may receive can help ease any concerns and guide you in making informed decisions about your next steps. The outcomes typically fall into two categories: negative and positive, each carrying its own implications.
Negative Results
A negative result generally means that no harmful agents were detected in the sample. This outcome is often reassuring, indicating that you are not currently infected with the organisms being tested for. However, it’s important to note that a negative result does not always rule out the possibility of infection, as some microorganisms may not be detectable at certain stages or using specific methods.
Positive Results
If harmful agents are detected, a positive result will indicate the presence of specific microorganisms or infections. While this can be concerning, it provides essential information that can guide treatment. Depending on the type of infection identified, your healthcare provider will discuss available options for managing or eliminating the infection. Further tests may also be necessary to confirm the diagnosis or assess the extent of the infection.
Ultimately, understanding your results allows you and your healthcare provider to take the necessary steps toward better health, whether it involves immediate treatment or continued monitoring. Regular follow-ups may also be advised to ensure effective management of any detected conditions.
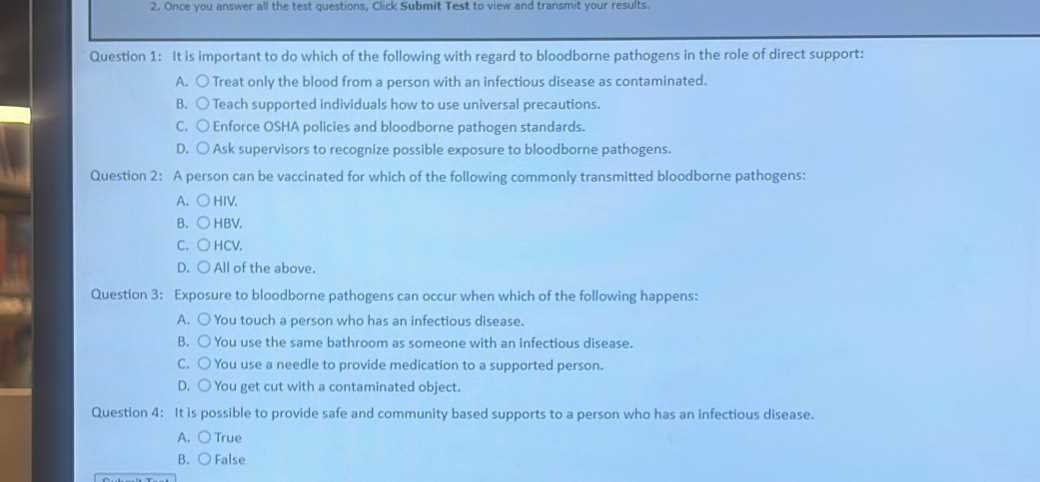
Interpreting Blood Pathogen Test Results
Understanding the results of diagnostic screenings can sometimes be challenging, as the findings can vary depending on the type of infection or condition being investigated. The key to interpreting these results lies in recognizing what each outcome signifies and how it relates to your overall health. A proper understanding of the results helps guide treatment decisions and ensures that you can take the appropriate next steps in managing your health.
Results are typically categorized into two main types: negative and positive. A negative result indicates that no harmful microorganisms were detected in the sample, which often suggests that there is no active infection. However, some infections may not be immediately detectable or could be in early stages, meaning that further tests might still be necessary in some cases.
On the other hand, a positive result means that an infection or harmful organism has been found. This may require further investigation to identify the specific microorganism and determine the most effective treatment options. Your healthcare provider will likely recommend additional steps based on the type of infection, its severity, and any symptoms you may be experiencing.
It is important to remember that the interpretation of results should always be done by a medical professional, as they are able to consider your overall health, medical history, and any potential risk factors when making recommendations for treatment or further tests.
Types of Blood Pathogens Tested For
There are several harmful microorganisms that can be present in the bloodstream, each causing different health concerns. These infections are commonly investigated through diagnostic evaluations to determine their presence and identify the most effective treatment. Below is a table outlining some of the most frequently tested organisms and the associated health risks.
| Infectious Agent | Type of Infection | Health Risks |
|---|---|---|
| HIV | Viral | Weakens the immune system, potentially leading to AIDS if untreated. |
| Hepatitis B | Viral | Causes liver inflammation, which can result in cirrhosis or liver cancer. |
| Hepatitis C | Viral | Damages the liver, often leading to chronic conditions and liver failure. |
| Syphilis | Bacterial | Can cause long-term organ damage if left untreated, including heart and brain problems. |
| Malaria | Parasitic | Severe fever and anemia, potentially leading to organ failure if not treated. |
| Sepsis | Condition | Life-threatening condition caused by the body’s response to an infection. |
These are just a few examples of the infections that can be detected through these evaluations. Each pathogen requires specific diagnostic methods to identify its presence and determine the appropriate course of treatment. The results of these tests are crucial for ensuring that individuals receive the right care as soon as possible.
Why Blood Pathogen Testing Is Important
Identifying harmful microorganisms within the body is essential for safeguarding overall health. Many infections can remain undetected in the early stages, leading to complications that may worsen over time. Diagnostic evaluations help pinpoint these infections, allowing for timely intervention and appropriate treatment. Early detection not only improves outcomes but also prevents the spread of infections to others.
Prevention and Early Detection
One of the primary reasons for conducting such screenings is to detect infections before they cause significant damage. Many microorganisms can remain dormant or produce mild symptoms, making it difficult for individuals to recognize the underlying issue. By identifying these infections early, healthcare providers can initiate treatment, preventing further complications and promoting faster recovery.
Targeted Treatment and Management
Once harmful agents are detected, doctors can tailor treatments to address specific infections, ensuring more effective management. Knowing the exact cause of the infection allows for the selection of the best possible treatment method, whether it’s through medication, lifestyle adjustments, or additional procedures. Without proper diagnosis, treatment may be delayed or misdirected, leading to prolonged illness or complications.
In summary, diagnostic screenings are crucial in identifying infections that might otherwise go unnoticed. Early detection and targeted management not only improve health outcomes but also play a key role in preventing the spread of infectious diseases to others.
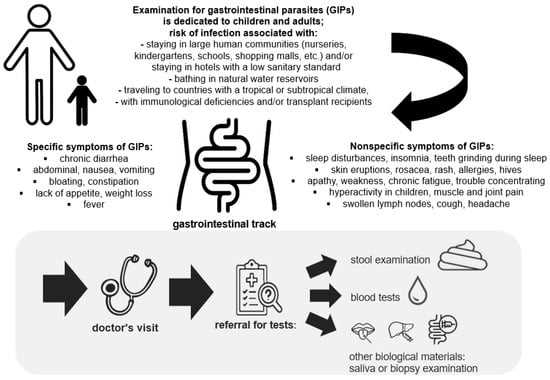
Symptoms Indicating the Need for Testing
Recognizing certain symptoms can help determine when it’s time to seek a diagnostic evaluation for potential infections. Many harmful microorganisms can cause a range of signs that are often mistaken for other conditions. When specific symptoms occur, it is essential to consult a healthcare provider to assess whether further investigation is needed. Here are some common indicators that suggest you may need to be tested for infections.
- Unexplained Fever: A persistent fever that doesn’t seem to have an obvious cause could indicate an underlying infection.
- Fatigue and Weakness: Feeling unusually tired or weak for an extended period may signal an infection that is affecting your body.
- Unusual Pain or Discomfort: Persistent pain, especially in joints, muscles, or the abdomen, could be a sign of an active infection.
- Skin Rashes or Sores: The appearance of unexplained rashes, sores, or open wounds may suggest the presence of an infectious organism.
- Shortness of Breath: Difficulty breathing or feeling out of breath without exertion could be a serious symptom linked to infections.
- Swollen Lymph Nodes: Swollen lymph nodes often indicate that the body is fighting off an infection.
- Night Sweats: Excessive sweating at night without physical exertion is another common symptom of infections.
- Chronic Cough or Sore Throat: A persistent cough or sore throat that lasts more than a few days may require further investigation.
If you experience any combination of these symptoms, it’s essential to consult a healthcare provider to determine if diagnostic screening is necessary. Early intervention can significantly improve health outcomes by addressing infections before they escalate into more serious health problems.
How Accurate Are Blood Pathogen Tests
The accuracy of diagnostic screenings is a crucial factor in ensuring proper diagnosis and treatment. While modern medical tests are highly reliable, no test is perfect, and several factors can influence the results. Understanding the potential limitations and strengths of these screenings can help individuals and healthcare providers make more informed decisions about next steps and treatment options.
- Sensitivity: This refers to a test’s ability to correctly identify individuals with an infection. A highly sensitive test minimizes false negatives, meaning it will more likely detect the presence of harmful organisms when they are indeed present.
- Specificity: Specificity refers to a test’s ability to correctly identify individuals who do not have an infection. A test with high specificity reduces the chances of false positives, ensuring that individuals without the infection are not misdiagnosed.
- Sample Collection: The accuracy of results can be influenced by how the sample is collected. Improper sample handling or contamination during collection may lead to inaccurate results, which is why it’s essential to follow proper protocols.
- Timing: The timing of the test also plays a critical role. Some infections may not be detectable immediately after exposure. In such cases, testing at the right time is essential to achieve an accurate result.
- Laboratory Quality: The capabilities and technology available at the testing facility can impact the accuracy of results. High-quality laboratories with advanced equipment tend to produce more reliable results.
Despite the strengths of these diagnostic tools, false positives and false negatives can occur. If there is any doubt about the results, healthcare providers may recommend additional tests or repeat evaluations to confirm the diagnosis. Ultimately, accurate interpretation of results, considering all factors, is essential to making the best decisions for treatment and care.
When to Seek Medical Advice After Testing
After undergoing a diagnostic procedure, it is essential to understand when you should follow up with your healthcare provider. Even if initial results seem clear, certain circumstances may require further consultation. Recognizing when to seek professional advice ensures that you receive appropriate care and guidance for managing your health effectively.
When to Follow Up
If you experience any of the following situations, it may be necessary to consult a doctor even after the procedure:
- Unexplained Symptoms: If you continue to experience unusual symptoms such as fatigue, unexplained pain, or fever after the procedure, it’s important to seek advice.
- Positive Results: If your results indicate the presence of an infection or harmful organism, it’s crucial to understand the next steps and get a treatment plan from your healthcare provider.
- False Negative Concerns: If symptoms persist but initial results were negative, you should discuss the possibility of retesting or alternative diagnoses with your doctor.
- Changes in Health: Any new or worsening symptoms, such as difficulty breathing, swelling, or changes in skin condition, require medical evaluation.
How to Prepare for a Follow-Up Appointment
To make the most out of your follow-up visit, it’s helpful to prepare by:
- Noting any new or persistent symptoms since the procedure.
- Bringing your previous test results for reference.
- Asking about possible treatment options or next steps based on the results.
Regular communication with your healthcare provider is essential for proper care, especially when results require clarification or further action. Knowing when to seek advice ensures your health is properly managed and any necessary interventions are made promptly.
What Happens After Positive Test Results
Receiving positive results from a diagnostic screening can be an unsettling experience, but understanding what comes next is essential for managing your health. When harmful microorganisms are detected, it opens the door for a comprehensive plan to address the issue. This section will outline the common steps to take following positive findings and the actions you can expect from healthcare professionals.
- Confirming the Results: In some cases, your healthcare provider may recommend additional screenings to confirm the initial findings. This is done to ensure the accuracy of the diagnosis.
- Understanding the Diagnosis: A healthcare provider will explain the type of infection or harmful organisms identified in the screening. It’s important to fully understand the condition and its implications.
- Developing a Treatment Plan: Based on the diagnosis, your doctor will discuss various treatment options, which may include medication, lifestyle adjustments, or further monitoring. The goal is to address the infection and prevent it from spreading or worsening.
- Monitoring Your Health: Ongoing follow-up may be necessary to assess the effectiveness of treatment and ensure the infection is properly managed. Regular check-ups might be scheduled to track progress.
- Informing Close Contacts: Depending on the type of infection, you may be advised to inform those in close contact, as certain conditions can be contagious. Your provider will guide you on how to handle this.
While a positive result may bring concern, prompt action and professional guidance can help you manage the situation effectively. By following your healthcare provider’s instructions, you can work towards a full recovery and minimize potential risks to your health.
How Blood Pathogen Tests Affect Treatment Plans
Diagnostic screenings play a crucial role in shaping healthcare strategies, especially when identifying harmful microorganisms in the body. The results from these procedures directly influence the course of treatment, ensuring that healthcare providers can tailor interventions to the specific condition. Understanding how these findings impact your care plan helps you make informed decisions about your health.
Once the presence of an infection or harmful agents is detected, treatment options are determined based on the nature of the condition. The more specific the results, the more targeted the approach can be. In some cases, medications may be prescribed to eliminate the cause, while in others, additional monitoring may be necessary to track the progression of the condition.
Here’s how these results typically affect treatment plans:
- Targeted Medications: If a specific infection is identified, doctors can prescribe the most effective drugs, such as antibiotics or antiviral medications, tailored to combat the identified microorganism.
- Preventative Measures: For certain conditions, the findings may prompt recommendations for lifestyle changes or preventative measures to reduce the risk of transmission or recurrence.
- Specialist Referrals: Some conditions may require the expertise of a specialist. Based on the results, your primary healthcare provider may refer you to a specialist for more advanced care.
- Ongoing Monitoring: If the results indicate a chronic or complex infection, regular check-ups may be needed to monitor the effectiveness of treatment and ensure that the condition is well-managed.
Ultimately, the impact of diagnostic results on your treatment plan underscores the importance of timely testing. It allows for a more precise, personalized approach to care, improving the likelihood of successful treatment and better long-term health outcomes.
Preparing for a Blood Pathogen Test
Proper preparation before undergoing a diagnostic screening is essential to ensure accurate results. By following a few simple steps, you can help your healthcare provider gather the most reliable information. This section provides guidance on how to prepare effectively for your upcoming screening.
Steps to Take Before the Screening

- Follow Pre-Procedure Instructions: Your healthcare provider may give you specific guidelines before the procedure, such as fasting or avoiding certain foods or medications. Be sure to follow these instructions to ensure the best outcome.
- Hydrate: Drinking water can help make the procedure smoother, especially if blood is being drawn. However, follow any restrictions provided by your doctor regarding fluid intake.
- Avoid Certain Substances: Some substances, like alcohol or recreational drugs, can affect the results of the screening. Make sure to avoid these for the recommended period before your visit.
- Notify Your Doctor: If you are taking any medications, supplements, or have any ongoing health conditions, inform your doctor. This information can be crucial in interpreting your results correctly.
What to Expect During the Procedure
- Brief and Simple Process: Typically, the procedure is straightforward and involves minimal discomfort. If blood is drawn, it usually takes only a few minutes.
- Relax and Stay Calm: If you’re nervous about the screening, try to stay calm. Deep breathing can help reduce anxiety and make the experience more comfortable.
By preparing appropriately and understanding what to expect, you can ensure that the procedure is as smooth and effective as possible, leading to accurate results that will guide your healthcare plan.
Risks Involved in Blood Pathogen Testing
While diagnostic screenings are generally safe, there are some risks associated with the process. Understanding these potential complications can help you prepare mentally and physically for the procedure. This section outlines the key risks that may arise during and after diagnostic screenings for infectious agents.
Potential Complications During the Procedure
- Discomfort or Pain: The procedure typically involves collecting a sample, which may cause some discomfort. Most people experience minimal pain, but in rare cases, it can be more intense.
- Bruising or Swelling: After a sample is collected, some individuals may develop mild bruising or swelling at the site. This usually resolves on its own within a few days.
- Infection: Although the risk is very low, there is a small chance of infection at the site where the sample is collected. Proper sterilization and post-procedure care significantly minimize this risk.
Post-Procedure Risks and Considerations
- False Positives or Negatives: No diagnostic procedure is flawless. There is a possibility of receiving a false positive or negative result, which may require follow-up testing for confirmation.
- Anxiety and Emotional Stress: For some, the wait for results can cause anxiety or emotional stress. It is important to manage these feelings and communicate with your healthcare provider if needed.
Despite these potential risks, the benefits of understanding your health status far outweigh the temporary discomforts. By being informed and following any post-procedure instructions, you can minimize these risks and ensure a smoother experience.
Costs of Blood Pathogen Tests
Understanding the costs associated with diagnostic screenings for infectious agents is essential for anyone considering such procedures. The total cost can vary depending on several factors, including the type of screening, the healthcare provider, and your location. This section provides an overview of the different cost components involved in these procedures.
Factors Affecting the Cost
- Type of Screening: The complexity and type of screening can significantly impact the cost. Some screenings may require advanced equipment or additional follow-up tests, increasing the overall price.
- Location: Healthcare costs can vary depending on geographic location. Urban areas or specialized medical centers may have higher fees compared to rural healthcare providers.
- Insurance Coverage: If you have health insurance, coverage for screening services may help reduce out-of-pocket expenses. However, some policies may not fully cover certain screenings.
- Healthcare Provider: Different healthcare providers or labs may have different pricing models. It’s important to compare costs to find the most affordable option.
Average Costs for Screening
The costs of diagnostic screenings for various infectious agents can range widely depending on the aforementioned factors. Below is a general estimate of the costs you may encounter:
| Type of Screening | Estimated Cost |
|---|---|
| Basic Screening | $50 – $150 |
| Comprehensive Screening | $200 – $500 |
| Specialized or Follow-up Tests | $300 – $1,000+ |
It’s important to consult with your healthcare provider and insurance company to get an accurate estimate based on your specific situation. Planning ahead and exploring all payment options can help you manage the costs of these essential procedures.