For healthcare professionals involved in the care of newborns, understanding the core principles of life-saving techniques is crucial. This section provides a structured approach to mastering the necessary skills for handling critical situations in neonates. The information here focuses on key concepts, methodologies, and practical tips that are vital in emergency scenarios.
Proper training and immediate response are essential when dealing with compromised newborns. Whether you’re preparing for certification or refining your knowledge, having a clear grasp of each step in resuscitation can significantly impact outcomes. The guidance offered here helps clarify complex procedures and enhances the overall understanding of the process.
With real-life scenarios in mind, this section presents key challenges that professionals often face during urgent interventions. By exploring common obstacles and the best practices for overcoming them, individuals can gain confidence in their ability to deliver timely and effective care in critical moments.
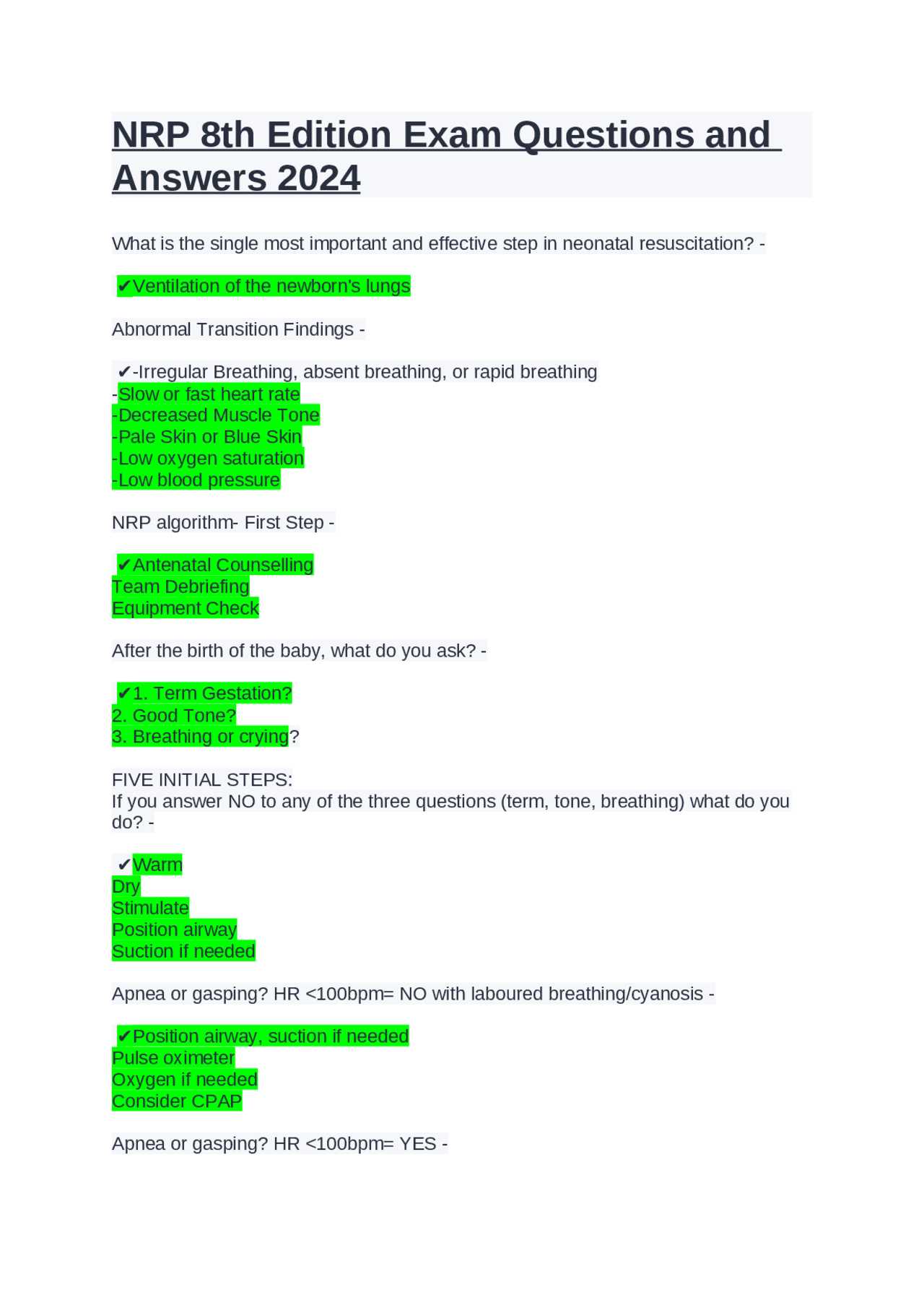
NRP Certification Exam Overview
For healthcare providers involved in neonatal care, obtaining certification in life-saving practices is essential. This examination evaluates one’s ability to perform crucial techniques required for assisting newborns in distress. The test ensures that professionals are well-prepared to handle emergency situations with the appropriate knowledge and skills.
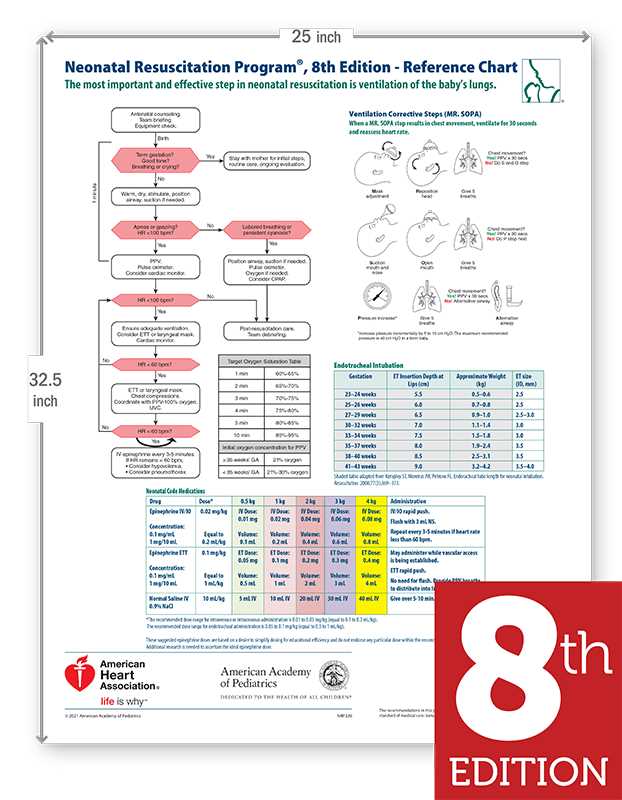
The certification process consists of a series of practical and theoretical assessments. Candidates must demonstrate proficiency in various procedures such as airway management, ventilation, and chest compressions. Additionally, understanding vital signs, medication administration, and effective teamwork during resuscitation scenarios is also examined.
To succeed, it’s important to familiarize oneself with the core concepts and clinical guidelines. Regular practice and review of common interventions ensure that candidates are confident and capable under pressure. Certification not only reinforces technical expertise but also emphasizes critical thinking and decision-making in high-stress environments.
Key Concepts in Neonatal Resuscitation
When assisting a newborn in distress, a solid understanding of essential principles is critical for ensuring effective care. Mastering the basic steps involved in stabilizing a neonate can make a significant difference in outcomes. From initial assessment to ongoing support, each phase requires careful attention to detail and proper technique.
Initial Assessment and Stabilization
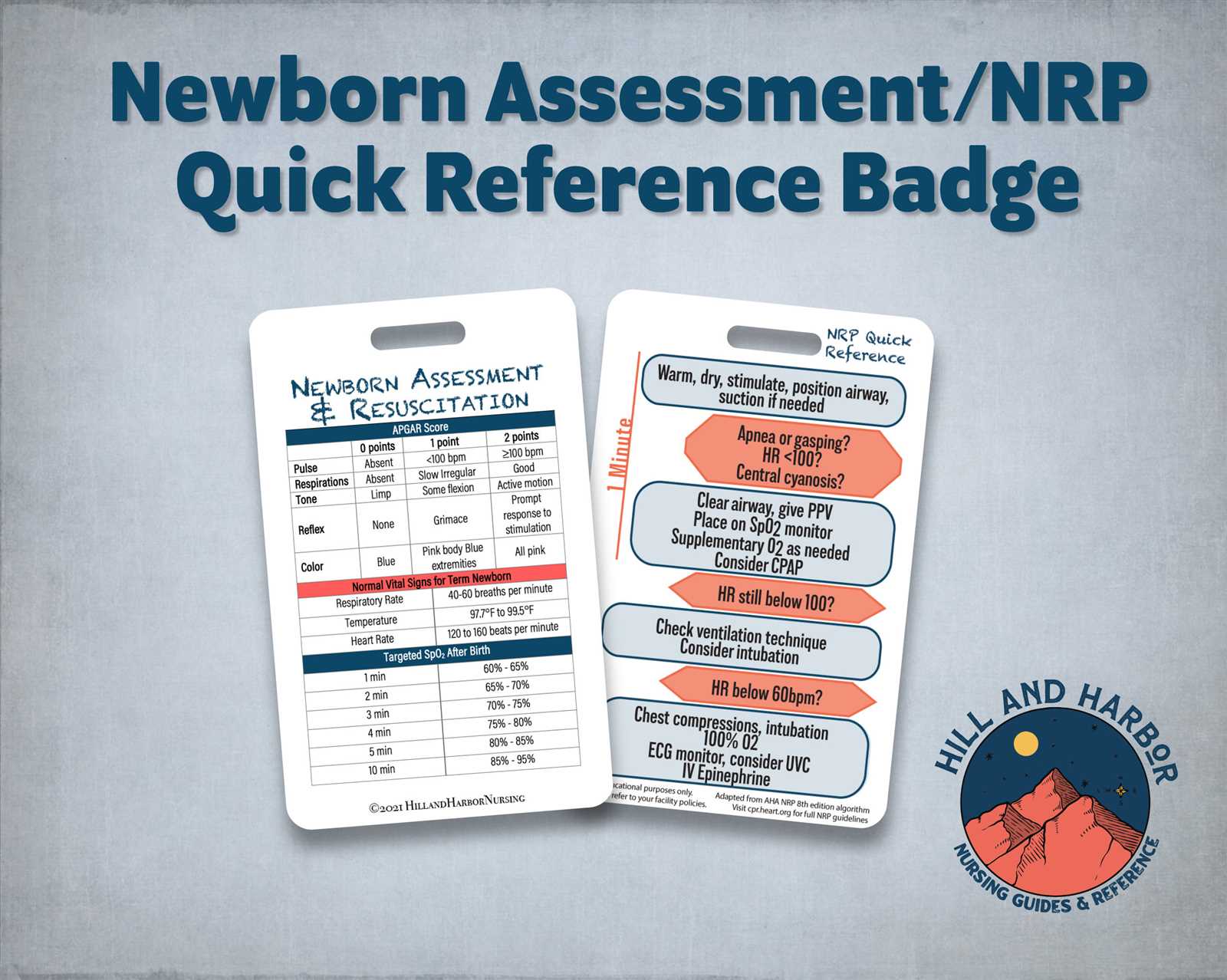
The first moments after birth are crucial. Ensuring that the baby is breathing and has an adequate heart rate is the foundation of any resuscitation effort. Immediate evaluation of the infant’s airway, breathing, and circulation sets the stage for intervention. If any issues are identified, timely actions such as clearing the airway or initiating ventilation are necessary.
Ongoing Support and Monitoring
Once initial stabilization has been achieved, continuous monitoring of the neonate’s vital signs is essential. Adjusting techniques based on the baby’s response ensures that the most appropriate care is provided. Team coordination plays a significant role in maintaining a structured and efficient approach throughout the procedure, with each member performing their role effectively.
Common NRP Exam Questions Explained
Preparing for certification often involves understanding the most frequent scenarios that may arise during the assessment. These scenarios test your ability to apply essential techniques in real-world situations. By exploring the types of challenges typically presented, candidates can build confidence and improve their response times in critical situations.
One of the most common scenarios revolves around managing airway obstruction in a newborn. Understanding the proper steps to clear the airway and initiate ventilation is crucial. Additionally, recognizing when to escalate intervention, such as the administration of medications or chest compressions, is often tested.
Another frequent topic involves assessing a neonate’s heart rate. Being able to interpret heart rate patterns and knowing when to intervene with effective methods, such as administering positive pressure ventilation, is a key component of the evaluation process.
Understanding Neonatal Heart Rate Assessment
Monitoring the heart rate of a newborn is a critical aspect of resuscitation and ongoing care. The heart rate provides important insights into the infant’s cardiovascular status and guides the next steps in treatment. Accurate assessment of this vital sign helps determine the need for interventions such as ventilation or chest compressions.
Normal and Abnormal Heart Rate Ranges
A healthy heart rate is essential for proper circulation and oxygen delivery to tissues. The typical range for a neonate’s heart rate is:
- Normal range: 120–160 beats per minute (bpm)
- Bradycardia (slow heart rate): Below 100 bpm
- Tachycardia (fast heart rate): Above 180 bpm
Any deviation from these ranges, particularly bradycardia, may require immediate intervention to prevent further complications.
Assessing Heart Rate in Critical Situations
In situations where resuscitation is necessary, a rapid assessment of the heart rate helps determine the urgency of the intervention. If the heart rate drops below 60 bpm despite adequate ventilation, chest compressions should be initiated. Additionally, if the rate is above 180 bpm, it may indicate a need to evaluate underlying causes, such as hypoxia or over-stimulation.
Continuous monitoring of heart rate throughout the resuscitation process is essential to guide healthcare providers in adjusting their techniques and ensuring optimal outcomes for the newborn.
What to Expect in NRP Skills Tests
Skills assessments play a critical role in evaluating a healthcare provider’s ability to perform essential life-saving procedures in neonates. These practical evaluations are designed to simulate real-life scenarios where quick, decisive action is required. Candidates will be tested on their ability to effectively manage critical situations and provide appropriate care under pressure.
During the assessment, you will be expected to demonstrate proficiency in a variety of hands-on techniques, such as:
- Clearing the airway and providing adequate ventilation
- Performing chest compressions and proper timing
- Administering medications when indicated
- Monitoring vital signs and making necessary adjustments
- Working in collaboration with a team to ensure coordinated efforts
Each scenario is carefully crafted to assess how well you respond to changes in the condition of the neonate. You will need to show that you can assess, act, and reassess quickly, ensuring that interventions are appropriate and timely. Effective communication with team members is also a key component of these tests.
Successful completion of the skills evaluation requires both technical knowledge and the ability to apply it in high-stress situations. Preparing thoroughly for each aspect of the practical exam will help ensure you are ready to face these challenges confidently.
Effective Airway Management Techniques
Ensuring proper airway management is vital when resuscitating a newborn. Clearing and securing the airway allows for adequate ventilation and oxygenation, which are critical to stabilizing the infant. Different techniques are employed depending on the severity of the obstruction and the neonate’s condition.
The first step in managing the airway is to assess whether the infant is breathing. If the baby is not breathing or has inadequate respiration, immediate intervention is required. Clearing the airway using gentle suction is often necessary to remove any obstructions such as mucus or amniotic fluid.
When ventilation is needed, the preferred method is typically positive pressure ventilation (PPV) using a bag-valve-mask device. It’s important to maintain a proper seal and adjust the pressure to avoid excessive force, which could damage the neonate’s fragile lungs.
In more severe cases, if PPV is ineffective or difficult, advanced techniques such as intubation may be necessary. Intubation involves inserting a tube into the trachea to ensure a secure airway and facilitate ventilation. It requires skill and precision, especially in neonates, as their airways are narrow and delicate.
Throughout the process, monitoring the infant’s heart rate, oxygen levels, and overall response to interventions helps guide further actions. Effective airway management relies on quick decision-making, coordination, and proper technique to optimize outcomes for the newborn.
Rescue Breathing and Chest Compressions
In critical situations where a newborn’s heart rate is low and breathing is insufficient, two essential techniques are employed to restore normal circulation and oxygenation. These interventions involve the careful application of chest compressions combined with rescue breathing. Proper execution of these methods can significantly improve the chances of survival in neonates during emergencies.
Rescue Breathing
Rescue breathing is initiated when a baby is not breathing or has inadequate ventilation. The goal is to provide oxygen to the lungs and maintain a steady flow of oxygenated blood to vital organs. The following steps are critical in performing effective rescue breathing:
- Ensure the airway is clear and open before initiating breaths.
- Deliver gentle breaths using a bag-valve-mask device, or if trained, use mouth-to-mouth resuscitation.
- Each breath should be enough to make the chest rise but not too forceful to cause lung damage.
- Observe the neonate’s chest to ensure the air is entering the lungs effectively.
Chest Compressions
When a newborn’s heart rate falls below 60 beats per minute despite adequate ventilation, chest compressions become necessary. These compressions help circulate oxygenated blood to the brain and other vital organs. The key steps for effective chest compressions are:
- Place two fingers or thumbs (depending on the size of the infant) on the lower half of the breastbone.
- Apply firm pressure to compress the chest by about one-third of its depth.
- Perform compressions at a rate of 100–120 per minute, ensuring proper depth and recoil after each compression.
- Continue the cycle of compressions and breaths until the neonate shows signs of improvement or advanced help arrives.
These techniques, when performed correctly and in the right sequence, are vital for sustaining life and improving outcomes in critical neonatal resuscitation cases. Proper training and practice are essential to ensure that each step is executed effectively under pressure.
Neonatal Resuscitation Medications and Dosages
In certain neonatal emergencies, medications are essential to stabilize the infant and support vital functions such as circulation and respiration. Administering the correct medications in precise doses is critical to the success of resuscitation efforts. Each drug used during the process has a specific role in addressing underlying issues like hypoxia, low blood pressure, or abnormal heart rhythms.
Common Medications Used in Neonatal Resuscitation
Several medications are commonly utilized during resuscitation, depending on the newborn’s condition. Some of the most frequently administered include:
- Epinephrine: Used in cases of bradycardia or absent heart rate. It stimulates the heart and improves blood flow.
- Normal saline: Administered to increase blood volume in cases of hypovolemia.
- Bicarbonate: Often used when metabolic acidosis is suspected, helping to correct the pH balance in the body.
- Glucose: Given if hypoglycemia is identified to provide the necessary energy for normal body functions.
Proper Dosages and Administration
Each medication must be dosed according to the neonate’s weight and specific needs. Precise administration is vital to avoid adverse effects. The general dosage guidelines include:
- Epinephrine: Administered intravenously or via the umbilical vein at a dose of 0.1–0.3 mL/kg, repeated every 3-5 minutes if necessary.
- Normal saline: Typically administered in boluses of 10 mL/kg, particularly in cases of shock or dehydration.
- Bicarbonate: Given if pH levels are critically low, at a dose of 1–2 mEq/kg.
- Glucose: A bolus of 2–4 mL/kg of a 10% solution is often used to correct low blood sugar.
It is important to note that medications should only be administered after careful assessment of the infant’s condition and when other interventions, such as airway management and ventilation, have been appropriately carried out. Timely and accurate drug administration, combined with the correct dosages, can significantly improve the outcomes of neonatal resuscitation.
Signs of Effective Neonatal Ventilation
Proper ventilation is essential for stabilizing a newborn in respiratory distress. Ensuring that the airways are clear and that adequate oxygen is delivered can make a significant difference in the infant’s condition. However, it’s crucial to monitor for signs that indicate whether the ventilation is being carried out effectively.
Effective respiratory support is typically characterized by visible improvements in the neonate’s appearance and physiological response. Key indicators that ventilation is successful include:
- Chest Rise: The infant’s chest should rise with each breath, demonstrating that air is being delivered to the lungs.
- Improved Heart Rate: A noticeable increase in heart rate indicates that the baby’s cardiovascular system is responding positively to the improved oxygenation.
- Normalization of Skin Color: A shift from cyanosis (bluish discoloration) to a healthy pink or red tone signals that the oxygen levels in the blood are rising.
- Enhanced Muscle Tone: As oxygenation improves, the infant’s muscle tone should become more active, and the baby may start moving more freely.
- Stable Oxygen Saturation: The oxygen saturation levels in the blood should reach normal values, indicating that tissues are receiving adequate oxygen.
It’s important to continuously assess these signs during resuscitation efforts, as they can help guide the healthcare team in adjusting ventilation techniques and ensuring optimal care for the newborn. If these indicators are not observed, further adjustments to the ventilation strategy may be needed.
Choosing the Right Equipment for Neonatal Resuscitation
In critical situations where immediate action is needed to support a newborn’s breathing and circulation, the right tools play a crucial role in ensuring effective intervention. Selecting the appropriate equipment is vital for delivering the correct amount of support in a timely and safe manner. From airway management devices to monitoring equipment, each tool has a specific function that helps healthcare providers stabilize the infant.
Several key pieces of equipment are essential for neonatal resuscitation, and understanding their proper use can make a significant difference in the outcome. The main considerations when choosing the right tools include:
- Airway Devices: A clear airway is essential. Tools like neonatal-sized endotracheal tubes, laryngeal mask airways, and bag-valve-mask devices should be available and sized appropriately for the infant’s age and weight.
- Rescue Breathing Equipment: A self-expanding bag with a mask is often used to deliver breaths. Ensuring the bag is the right size and the mask forms a proper seal around the infant’s face is important for effective ventilation.
- Monitoring Tools: Tools like pulse oximeters, stethoscopes, and electrocardiograms are crucial for assessing the infant’s heart rate, oxygen levels, and overall response to treatment.
- Medication Administration Supplies: Proper intravenous or intraosseous access is required for medication delivery. Syringes, umbilical catheters, and intravenous fluids should be available to handle emergency needs.
Having the correct equipment on hand, as well as understanding how to use it, ensures that healthcare providers are fully prepared to manage a newborn in distress. Regular training and equipment checks are necessary to guarantee that all tools are functioning correctly when needed most.
Teamwork and Communication in Resuscitation
Effective collaboration and clear communication are essential elements in any emergency situation, particularly when it comes to providing life-saving interventions. In critical moments, the ability of a team to work seamlessly together can significantly impact the success of the procedure. Each team member plays a specific role, and strong coordination ensures that tasks are completed efficiently and safely.
Successful resuscitation relies on a well-organized team where each member understands their responsibilities and communicates effectively. This can include tasks such as airway management, monitoring vital signs, administering medications, and ensuring proper documentation. Clear, concise communication helps prevent errors and ensures that everyone is aware of the ongoing progress and adjustments needed.
- Role Clarity: Defining specific roles for each team member helps ensure that no critical task is overlooked. When everyone knows their responsibilities, it allows for more efficient action and better overall outcomes.
- Effective Communication: Clear, direct communication between team members, especially in high-pressure situations, is key. This includes giving and receiving updates on the patient’s status and coordinating the next steps in real-time.
- Leadership and Delegation: Strong leadership is essential for guiding the team through high-stress scenarios. A leader should be able to delegate tasks based on the strengths and skills of team members, keeping everyone focused and effective.
- Debriefing: After the procedure, it’s important to hold a debriefing session where team members can discuss what went well and what could be improved. This is an opportunity to reflect on the experience and enhance future performance.
In emergency situations, the team’s ability to work together with clear communication is just as important as the technical skills involved. A well-coordinated team can not only improve the chances of a successful outcome but also provide the necessary support for each member under intense pressure.
Managing Neonatal Asphyxia During Delivery
At the time of delivery, the health and well-being of the newborn depend significantly on the ability to establish normal breathing and circulation immediately after birth. When a newborn experiences difficulties in this process, it can lead to a critical condition where oxygen supply to vital organs is compromised. Managing this situation requires swift and precise interventions to restore normal physiological function and prevent long-term damage.
Effective management begins with recognizing the signs of insufficient oxygenation as early as possible. Key indicators such as poor muscle tone, irregular heart rate, and pale or cyanotic skin coloration can suggest that the infant is struggling to breathe on its own. In these cases, healthcare providers must act quickly to ensure adequate ventilation and oxygenation.
Steps in Managing Neonatal Asphyxia
| Step | Action |
|---|---|
| 1. Initial Assessment | Check for signs of distress such as abnormal breathing or low heart rate. Immediate actions may include clearing the airways if necessary. |
| 2. Provide Ventilation | Use a bag-valve-mask to deliver gentle breaths if the infant is not breathing on their own. Ensure the mask fits securely for effective air delivery. |
| 3. Chest Compressions | If the heart rate remains low despite ventilation, initiate chest compressions according to established guidelines. |
| 4. Medications | If the infant’s condition does not improve with ventilation and compressions, medications such as epinephrine may be required to stimulate the heart. |
| 5. Ongoing Monitoring | Continuously assess heart rate, oxygen saturation, and the infant’s overall condition to ensure progress and guide further interventions. |
It is crucial to act quickly and follow established procedures to improve outcomes in these critical situations. By using a systematic approach and ensuring that the team is well-prepared, healthcare providers can significantly improve the chances of a successful recovery for the newborn.
Understanding the Apgar Score in Resuscitation
The Apgar score is a critical tool used to assess the immediate health and well-being of a newborn following delivery. This score evaluates several vital signs that indicate how well the baby is transitioning from the protected environment of the womb to life outside. By assessing the infant’s overall condition, healthcare providers can make informed decisions about the need for further medical interventions.
It is performed at one minute and five minutes after birth, though additional assessments may be made if the baby’s condition does not improve. The score ranges from 0 to 10, with a higher score indicating better overall health. Each of the five parameters–heart rate, respiratory effort, muscle tone, reflex response, and skin color–contributes a specific score that helps guide the clinician’s next steps in care.
Key Components of the Apgar Score
- Heart Rate: Measures the newborn’s heart rate, with a higher rate indicating better oxygenation. A score of 0, 1, or 2 is assigned based on the heart rate.
- Respiratory Effort: Assesses how well the baby is breathing. A strong, regular breath is scored higher than weak or absent breathing.
- Muscle Tone: Evaluates the newborn’s muscle tone and movement, which can indicate overall strength and health.
- Reflex Response: Tests how the baby responds to stimulation, like a quick tap on the feet, which indicates neurological function.
- Skin Color: Assesses whether the baby’s skin is pink or blue, which helps indicate how well the infant is receiving oxygen.
Interpreting the Apgar Score
The score provides an immediate, though temporary, snapshot of the infant’s condition. A score of 7 or above typically suggests that the baby is in good health and does not require immediate resuscitation. A score between 4 and 6 may indicate that the baby needs some assistance with breathing or oxygenation, while a score of 3 or lower often signals a need for more intensive interventions, such as mechanical ventilation or chest compressions.
While the Apgar score is a valuable tool for assessing newborn health, it is only one part of the picture. Continuous monitoring and further clinical evaluation are essential to ensure the well-being of the infant in the hours following birth.
Common Mistakes in Resuscitation Training
While training for neonatal emergency care, it is essential to avoid common errors that can impact the success of the procedures. Inadequate preparation or misunderstanding key concepts can lead to delays in providing the necessary support to a newborn in distress. By addressing these frequent pitfalls, practitioners can improve their skills and enhance patient outcomes.
Many trainees focus on individual techniques without understanding how they interconnect in real-life situations. In emergency scenarios, the sequence and timing of interventions are as important as the interventions themselves. Missteps, such as incorrect assessment of vital signs or improper use of equipment, can hinder the effectiveness of resuscitation efforts.
Common Mistakes to Avoid
- Delayed Recognition of Respiratory Distress: Failing to identify early signs of inadequate breathing or oxygenation can lead to unnecessary delays in intervention.
- Improper Airway Management: Using the wrong airway tools or techniques, such as incorrect positioning or overuse of suction, can obstruct the airway or cause additional harm.
- Incorrect Chest Compression Technique: Not providing compressions at the right depth or rate can reduce the effectiveness of circulation, preventing vital organs from receiving adequate oxygen.
- Overlooking the Importance of Teamwork: Not communicating clearly with team members or failing to delegate tasks appropriately can slow down the response time, especially in high-pressure situations.
- Misunderstanding Medication Dosages: Administering the wrong dosage or using medications incorrectly can have serious consequences, especially when dealing with newborns who have different physiological responses.
How to Overcome These Challenges
Practitioners should emphasize regular practice and scenario-based simulations during training to help avoid these mistakes. Continual feedback, peer review, and self-assessment are essential for improving performance and ensuring readiness for real-life emergencies. Moreover, understanding the underlying principles of neonatal care, such as the importance of timely intervention and clear communication, can significantly reduce errors in critical moments.
Training should focus on practical application, not just theoretical knowledge. By mastering the correct techniques and understanding how to coordinate with other team members, healthcare providers can respond effectively in neonatal emergencies and provide the best care possible for the newborns in their care.
How to Handle Neonatal Complications
Managing complications during the newborn’s early stages requires swift decision-making, specialized techniques, and a well-coordinated approach. These conditions can range from respiratory distress to more severe issues like infections or cardiac problems, all of which require prompt and effective intervention. Understanding the signs of complications, how to assess them, and the correct procedures to follow can make all the difference in outcomes.
Each complication often demands a tailored response, but certain universal principles guide the management of these critical conditions. Early recognition, proper stabilization, and ongoing monitoring are essential to ensuring that the infant receives appropriate care. The ability to stay calm, work effectively with the team, and follow guidelines can greatly improve survival rates and minimize long-term effects for the newborn.
Common Neonatal Complications
| Complication | Symptoms | Management Techniques |
|---|---|---|
| Respiratory Distress | Rapid or labored breathing, cyanosis, grunting, nasal flaring | Oxygen supplementation, ventilation support, suctioning |
| Hypothermia | Low body temperature, lethargy, poor feeding | Warm blankets, radiant warmer, skin-to-skin contact |
| Neonatal Sepsis | Fever, lethargy, poor feeding, abnormal skin color | Antibiotics, blood cultures, fluid management |
| Cardiac Arrest | Absence of heartbeat, lack of pulse | Chest compressions, medications (e.g., epinephrine), resuscitation |
Approach to Complication Management
The initial step in managing any complication is the quick identification of symptoms, followed by a rapid assessment to determine the severity. Once the condition is diagnosed, the appropriate interventions must be started immediately. In cases such as respiratory distress, the administration of oxygen or initiating ventilation may be the first priority. For infections like neonatal sepsis, prompt antibiotic therapy can be lifesaving.
It is also crucial to provide ongoing monitoring during the treatment process. Continuous observation of vital signs, including heart rate, blood pressure, and oxygen levels, allows the healthcare team to adjust interventions as needed. Communication with team members is key in making adjustments and ensuring the best possible outcomes for the infant.
Finally, family communication plays a significant role. Offering clear explanations and guidance can help reduce the stress experienced by parents during these difficult times, ensuring that they feel supported as their child receives care.
Post-Resuscitation Care for Newborns
After a newborn has received emergency intervention, the next crucial phase of care focuses on stabilization and recovery. This period involves closely monitoring the infant’s vital signs, supporting respiratory and circulatory functions, and preventing potential complications. The goal is to ensure that the newborn is able to maintain homeostasis while receiving the necessary support to thrive.
Proper post-resuscitation management is essential to ensure that the infant does not experience any long-term consequences from the stressful delivery or resuscitation process. Careful attention is required in areas such as temperature regulation, nutritional support, and neurological monitoring. Providing the right environment and interventions can significantly reduce the risk of complications and promote recovery.
Key Aspects of Post-Resuscitation Care
- Monitoring Vital Signs: Regular checks of heart rate, oxygen saturation, respiratory rate, and blood pressure are essential to ensure stable conditions.
- Thermoregulation: Maintaining body temperature is vital to prevent hypothermia, which can hinder recovery.
- Respiratory Support: Continued respiratory support, such as supplemental oxygen or mechanical ventilation, may be required based on the newborn’s condition.
- Neurological Assessment: Regular assessments of neurological function help detect any signs of brain injury or distress early on.
- Feeding and Nutrition: Ensuring the newborn is able to feed, either through breastfeeding or via tube feeding, is critical for recovery.
Care Team Coordination
Effective communication and coordination between the healthcare team members is critical during this stage. Each team member plays an important role, whether it’s monitoring for signs of distress, providing respiratory support, or managing medications. Regular updates and discussions ensure that any changes in the newborn’s condition are addressed promptly, allowing for timely adjustments to treatment.
Family members also play an important role during this phase, as their emotional support and involvement can significantly impact the well-being of both the infant and the parents. Clear communication with the family, reassuring them of the care plan, and providing emotional support, is an important part of the overall recovery process.
Tips for Passing the NRP Exam
Preparing for the certification exam in neonatal care requires a combination of theoretical knowledge, practical skills, and the ability to stay calm under pressure. Success in this exam is not only about memorizing facts but also about applying critical thinking and hands-on techniques effectively. To excel, a strategic approach to studying and practice is essential.
While the process can be challenging, following some key strategies can help maximize your chances of success. Focus on understanding key principles, practicing skills regularly, and familiarizing yourself with the exam format. By combining these elements, you can approach the test with confidence and the right mindset.
Study Techniques to Master Key Concepts
- Review the Guidelines: Make sure you are familiar with the most up-to-date protocols and guidelines related to neonatal care. Understanding current recommendations is crucial.
- Practice Scenarios: Simulate real-life situations to build both your knowledge and confidence. This includes practicing with manikins or in team settings where you can refine your techniques.
- Understand the Rationale: Don’t just memorize steps–understand why each action is important. This helps in recalling the correct procedures during the exam.
- Take Practice Exams: Taking practice tests under timed conditions can help you get comfortable with the format and the types of scenarios you might encounter.
Essential Practical Skills
- Airway Management: Practice clearing airways and ensuring proper ventilation techniques. This is one of the core skills that will be tested during the practical portion of the exam.
- Chest Compressions: Repeated practice of the correct compression technique is key. Ensure you understand the appropriate depth and rate for neonatal chest compressions.
- Medication Administration: Learn the dosages and methods of administering medications during resuscitation. This is often tested in the form of both theoretical and practical components.
- Team Coordination: In a real emergency, working with a team is essential. Practice clear communication and collaboration with other healthcare providers.
By consistently reviewing the materials, practicing the skills, and preparing for different scenarios, you will be well-equipped to perform confidently during the exam. Approach your preparation with focus, and remember to take care of your mental and physical health throughout the process.