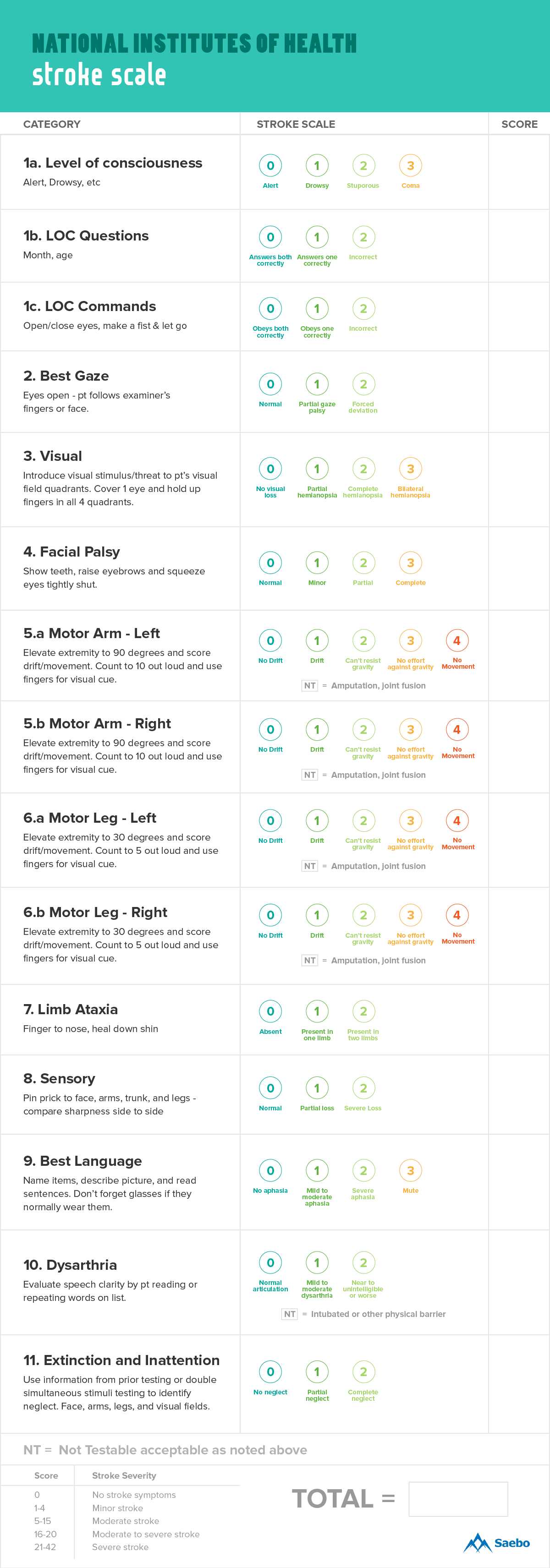
Accurate evaluation of neurological deficits plays a crucial role in understanding the severity of brain injuries or conditions. Medical professionals rely on standardized tools to assess a patient’s condition, which helps determine the appropriate course of treatment. These tools focus on various aspects of neurological function, from motor skills to cognitive abilities, and provide a clear picture of a patient’s state.
One such assessment system is widely used for measuring a patient’s neurological response. This method involves testing reflexes, speech, motor function, and other indicators, assigning numerical values to different outcomes. The scores provide essential insights into the extent of impairment, guiding healthcare providers in making informed decisions regarding immediate care and long-term management.
While scoring may seem straightforward, interpreting these results requires a solid understanding of the specific criteria and how they relate to overall health. Proper evaluation ensures that treatment decisions are based on objective data rather than subjective judgment, which is vital for improving patient outcomes. Understanding the intricacies of this assessment can help medical practitioners avoid common pitfalls and enhance the accuracy of their diagnoses.
NIH Stroke Scale Exam Answers
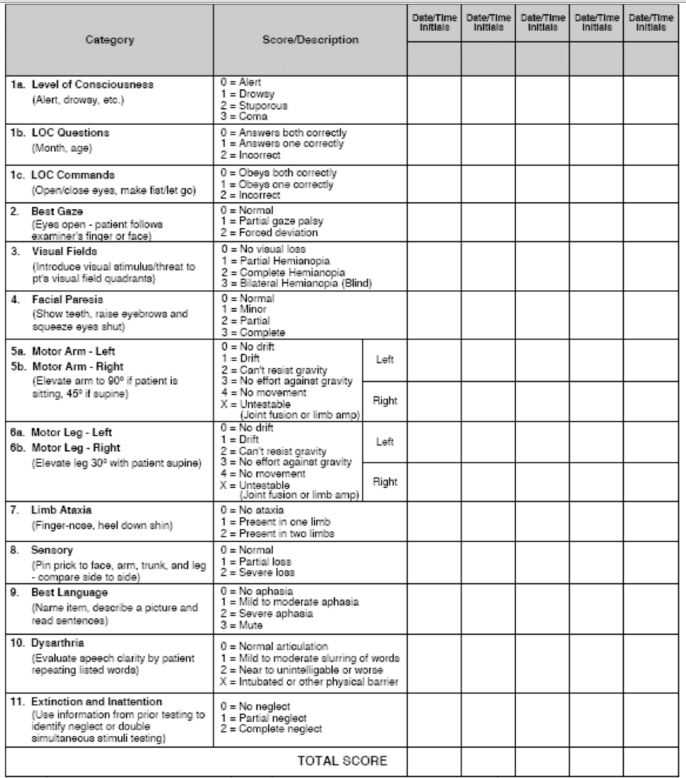
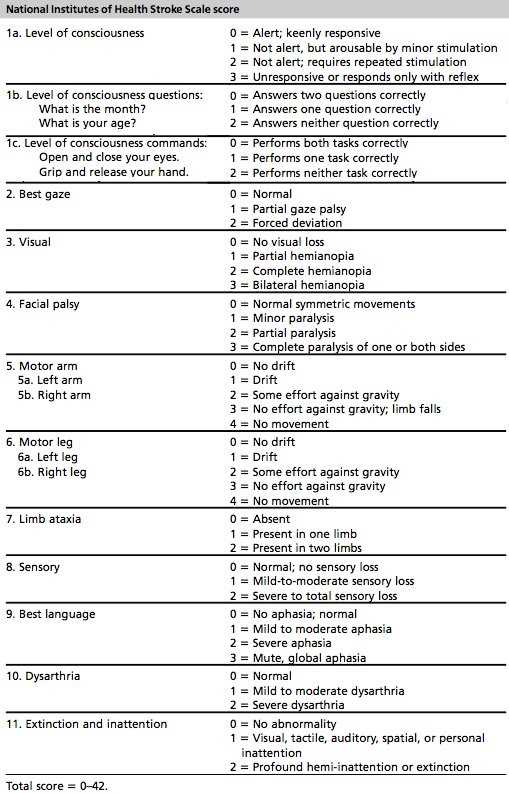
In neurological assessments, it is essential to evaluate a patient’s level of impairment accurately. Various tests are employed to assess cognitive, motor, and sensory functions, with numerical values assigned to specific responses. This objective scoring system helps healthcare providers quickly gauge the severity of brain injury and track recovery progress. A thorough understanding of these criteria is necessary for accurate assessments and effective treatment planning.
Understanding Key Evaluation Criteria
The assessment involves a series of tasks, each focusing on different aspects of a patient’s neurological state. These tasks assess a patient’s responsiveness, limb movements, and speech abilities. Scoring relies on the patient’s performance, which is then interpreted to determine the degree of impairment. It is vital to differentiate between varying levels of dysfunction to ensure the correct treatment approach is chosen.
Common Scoring Challenges and Considerations
While the scoring system is straightforward, challenges often arise when interpreting results. Factors such as patient cooperation, comprehension, and environmental conditions can affect the outcome of certain tests. Healthcare providers must account for these variables to avoid misinterpretation. Additionally, consistent practice and experience are crucial for achieving accurate results, as nuances in responses may require a more experienced eye to assess properly.
Understanding the NIH Stroke Scale
In the context of evaluating neurological impairments, it is crucial to employ a standardized method to assess a patient’s condition. This structured approach allows healthcare providers to quantify the severity of symptoms and understand the extent of a patient’s dysfunction. The process focuses on different aspects of brain function, ranging from basic motor skills to complex cognitive abilities. A clear understanding of the underlying methodology helps in delivering accurate assessments and making informed treatment decisions.
The assessment tool used in this approach is designed to evaluate the patient’s responses across several domains. Each domain is tested through a series of tasks or questions, and the responses are scored based on predefined criteria. These results give an overall picture of the patient’s neurological health, helping to determine the best course of action.
| Domain | Task | Score Range |
|---|---|---|
| Consciousness | Level of awareness | 0 – 3 |
| Motor Function | Limb movement abilities | 0 – 4 |
| Speech | Ability to communicate | 0 – 3 |
| Facial Symmetry | Facial droop assessment | 0 – 3 |
Each category plays a significant role in understanding the full scope of a patient’s condition. For example, evaluating consciousness can help determine the extent of brain function, while motor function tests gauge physical impairment. Through careful scoring and interpretation, this assessment method provides essential information for ongoing medical management and recovery planning.
Scoring Criteria for NIH Stroke Exam
The evaluation of neurological function relies heavily on a clear, consistent scoring system. The primary goal is to quantify the severity of impairments observed during an assessment, ensuring that healthcare providers have an objective basis for treatment decisions. Each task within the assessment has specific criteria, with corresponding points assigned based on the patient’s response. The final score reflects the overall condition and guides healthcare professionals in determining the appropriate care plan.
General Scoring Guidelines
The scoring system is designed to cover several key aspects of neurological function, each contributing to the final assessment. The criteria used in the evaluation help differentiate between varying levels of dysfunction and recovery. Points are assigned based on the extent of the patient’s response, ranging from full ability to no function at all. Here are some general guidelines:
- Consciousness: Points are given based on the patient’s level of alertness and responsiveness to stimuli.
- Motor Function: Scores reflect the ability to move limbs, with higher values indicating less impairment.
- Speech: The patient’s capacity to communicate effectively is assessed, with varying scores based on fluency and clarity.
- Facial Symmetry: The degree of facial drooping is evaluated to determine neurological damage.
Detailed Scoring Breakdown
Each domain is scored independently, and the results are combined to provide a comprehensive overview of the patient’s neurological status. The higher the score, the more severe the condition. The scoring system follows a structured approach:
- 0: No impairment or normal response.
- 1-2: Mild to moderate impairment, requiring further observation.
- 3-4: Severe impairment, indicating the need for urgent medical intervention.
This method ensures consistency in assessments and supports accurate decision-making. Proper understanding of these criteria is essential for all professionals involved in patient care, as it directly impacts the effectiveness of treatment strategies.
Interpreting NIH Stroke Scale Scores
Interpreting the results of a neurological assessment is a critical step in understanding the extent of impairment and determining appropriate treatment. The scores assigned to different tasks offer insights into the patient’s condition and provide valuable information for medical professionals. However, simply assigning scores is not enough; it is essential to understand what each score represents in the context of the patient’s overall health and recovery potential.
The scores reflect different levels of neurological function, ranging from normal to severely impaired. Understanding the implications of these numbers requires familiarity with the underlying tasks, as each score corresponds to specific observable behaviors or responses. By analyzing the scores, clinicians can assess whether the patient is improving, remaining stable, or worsening, which guides the next steps in care.
| Score Range | Interpretation | Clinical Implications |
|---|---|---|
| 0 – 4 | Normal to mild impairment | Indicates minimal neurological dysfunction, patient may require observation and supportive care. |
| 5 – 9 | Moderate impairment | Requires closer monitoring, potential for rehabilitation interventions to address dysfunction. |
| 10 – 15 | Severe impairment | Requires urgent medical intervention, potential for long-term disability without intensive treatment. |
By understanding how to interpret these scores, healthcare professionals can make better-informed decisions regarding immediate care, rehabilitation, and long-term management. It also enables a clearer picture of the patient’s progress over time, facilitating the adjustment of treatment plans as necessary.
Common Mistakes in Stroke Assessments
Accurate evaluation of neurological impairments is essential for effective treatment, but even experienced clinicians can make mistakes during assessments. These errors can lead to misinterpretation of a patient’s condition, affecting diagnosis and subsequent care decisions. It is crucial to be aware of common pitfalls to ensure that each assessment is as precise as possible.
One of the most frequent mistakes is overlooking subtle signs of impairment, especially when a patient appears to be minimally affected. Small deficits in motor function, speech, or cognitive abilities can easily be missed without a careful, systematic approach. Additionally, failing to account for environmental factors, such as patient fatigue or discomfort, can lead to inaccurate results. Properly assessing each task without rushing and ensuring the patient is in the best possible condition for evaluation are essential steps.
Other common errors include:
- Inconsistent scoring: Assigning incorrect points due to misunderstanding the severity of certain responses.
- Misinterpreting non-verbal cues: Relying too heavily on verbal responses and not adequately evaluating facial expressions or limb movements.
- Ignoring patient cooperation: Not considering how a patient’s ability to engage with the test might affect the results, especially in the case of cognitive impairments.
Being mindful of these issues can help clinicians avoid missteps and ensure that assessments are more accurate, ultimately leading to better treatment outcomes for the patient.
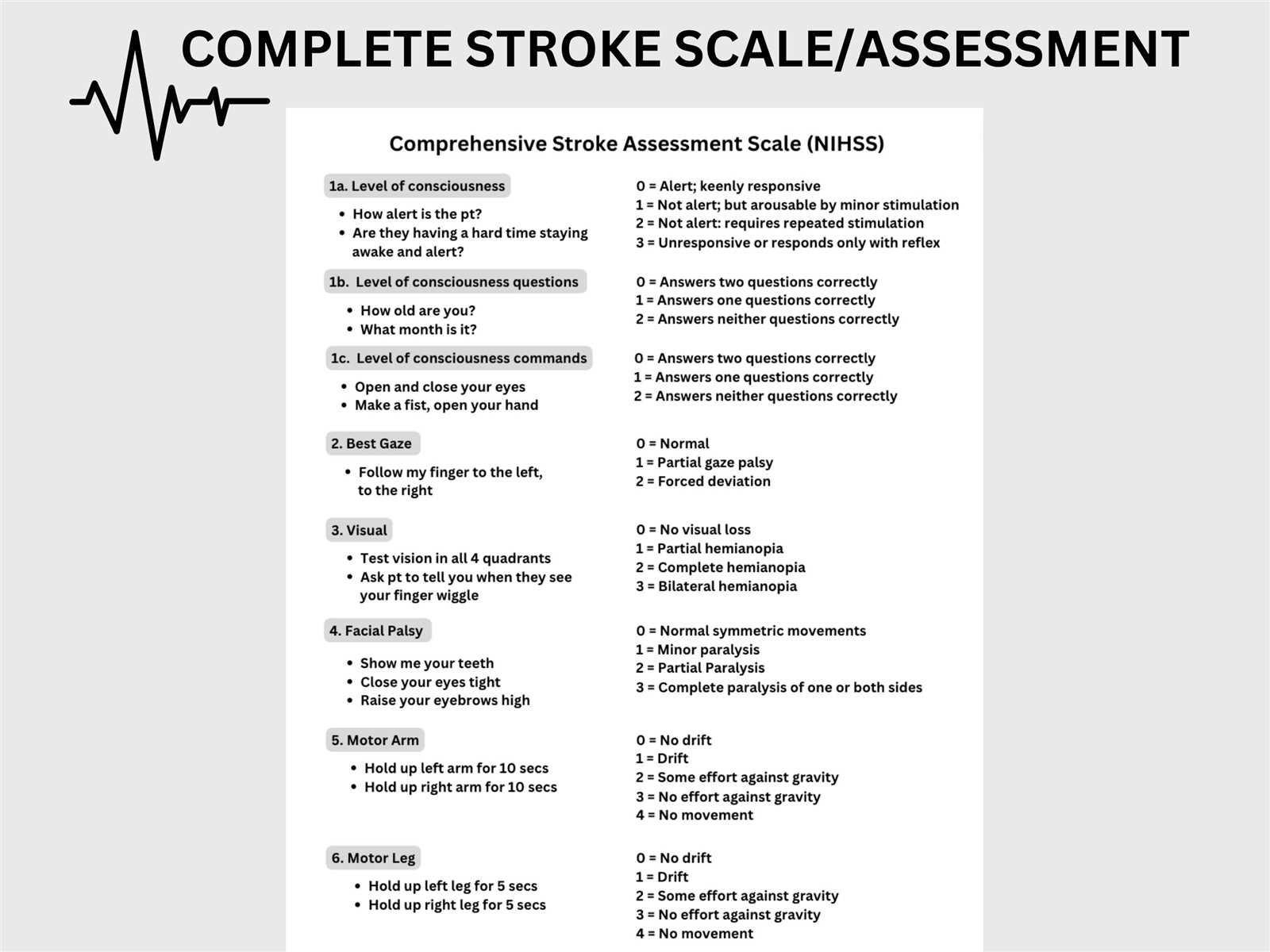
How to Administer the NIH Stroke Exam
Properly administering a neurological assessment is vital to ensure accurate evaluation of a patient’s condition. This process involves a series of structured tasks that assess different aspects of brain function, such as cognitive abilities, motor skills, and speech. To achieve reliable results, it is important to follow a consistent and systematic approach throughout the procedure.
Preparing the Patient
Before starting the assessment, ensure that the patient is in a comfortable and calm environment. Make sure they are seated or lying down in a relaxed position. Clear communication is essential: explain the process in simple terms, and ensure the patient understands the tasks they need to perform. If possible, provide them with some time to adjust and focus before beginning the assessment.
Following the Assessment Protocol
The assessment consists of several tasks, each focusing on different neurological functions. Administer each task carefully and note the patient’s responses. Be consistent in how you ask questions and observe their actions to avoid influencing the outcome. For example, when assessing motor abilities, guide the patient through movements slowly and give clear instructions. When evaluating speech or cognition, observe the clarity, fluency, and appropriateness of their responses. Always ensure that the patient is given ample time to respond, but do not provide cues or help unless necessary.
Following these steps ensures that the assessment is both accurate and reliable, providing essential insights into the patient’s neurological status and guiding the next steps in their treatment.
Assessment of Consciousness Levels
Evaluating a patient’s level of consciousness is one of the first and most crucial steps in assessing neurological health. Consciousness assessment helps determine how alert and responsive the individual is to external stimuli. This is critical in understanding the severity of any brain dysfunction, as impaired consciousness often indicates a more serious condition requiring immediate medical intervention.
When assessing consciousness, it is essential to observe the patient’s ability to respond to verbal, tactile, and noxious stimuli. The responses can vary from full awareness to complete unresponsiveness. The method of scoring for this aspect involves categorizing the patient’s reaction into distinct levels based on their reactions.
Levels of Consciousness
- Alert: The patient is fully aware of their surroundings and responsive to questions and commands without any difficulty.
- Confused: The patient responds but with some disorientation or confusion, often struggling to understand or follow commands.
- Stuporous: The patient exhibits minimal awareness and may only respond to stimuli such as touch or pain, with limited ability to communicate.
- Comatose: The patient is unresponsive to any form of external stimuli and does not exhibit purposeful reactions.
Important Considerations
- Consistency: Ensure that the same criteria are applied consistently throughout the assessment.
- Environmental Factors: Take into account any external factors, such as medications, that may affect consciousness levels.
- Time: Some patients may regain responsiveness over time, so it is important to monitor for changes in their condition.
By carefully assessing the patient’s level of consciousness, healthcare professionals can gather important information about the extent of neurological impairment and plan appropriate interventions.
Facial Droop and NIH Stroke Scale
Facial drooping is a significant sign of neurological impairment and is commonly observed in individuals with certain types of brain damage. This condition, characterized by a noticeable asymmetry in facial muscles, often affects the ability to smile, speak, or express emotions on one side of the face. It can result from various factors, including brain injury, and is frequently used as an indicator of more severe neurological deficits.
Assessing facial droop involves a simple observation of the patient’s facial symmetry and responsiveness to commands. Any drooping or weakness on one side of the face is typically an indication of underlying neurological dysfunction, which may be tied to a variety of health conditions. Understanding the severity of facial droop can provide vital clues about the patient’s overall condition and the extent of brain involvement.
Evaluating Facial Droop
- Ask the patient to smile: A noticeable asymmetry between the right and left side of the face may indicate facial droop.
- Observe for weakness: Weakness on one side of the face can be seen as drooping of the mouth or eyelid, and the inability to lift the brow.
- Check for involuntary movements: In some cases, the affected side may show a lack of movement or decreased responsiveness to voluntary commands.
Implications of Facial Droop
- Severe cases: Significant drooping or inability to move the face on one side is often associated with more severe impairment, potentially affecting other motor functions.
- Indication for further evaluation: Facial droop, especially when observed suddenly, warrants immediate medical attention and may indicate a more serious underlying condition.
- Recovery and rehabilitation: Depending on the cause, recovery from facial droop can vary. Early intervention and therapy can improve outcomes.
By accurately assessing and documenting facial droop, healthcare professionals can better understand the nature of the neurological impairment and make informed decisions about the appropriate course of treatment.
Arm Weakness and Stroke Scoring
Arm weakness is a key indicator of neurological dysfunction and is commonly assessed during clinical evaluations to gauge the extent of brain impairment. This condition can manifest as reduced strength, coordination, or control over the arms, often affecting one side of the body. Accurately scoring this weakness is crucial in understanding the severity of the damage and helps guide treatment decisions.
Assessing arm weakness involves a series of tests to determine the patient’s ability to move and control their arms. The severity of weakness is typically classified into different levels, from mild weakness to complete paralysis. This scoring system allows healthcare providers to objectively track the progression or improvement of the condition and tailor interventions accordingly.
Assessing Arm Weakness
- Ask the patient to raise both arms: Observe for any asymmetry or inability to hold the arm in the air.
- Test for arm drift: Have the patient close their eyes and hold both arms out. One arm may begin to drift downwards if weakness is present.
- Assess muscle strength: Gently apply pressure to both arms to check for resistance. Weakness may be indicated by a lack of force or difficulty maintaining posture.
Scoring Arm Weakness
- Normal: The patient exhibits equal strength in both arms with no noticeable weakness.
- Mild weakness: The patient shows some difficulty holding the arm up or controlling movement, but can still perform most tasks.
- Severe weakness: The arm is unable to be lifted or controlled, even with effort. The patient may have limited or no functional use of the arm.
- Paralysis: The arm exhibits no movement or response to commands, indicating complete paralysis or significant motor impairment.
Accurate scoring of arm weakness is essential for evaluating a patient’s condition and planning appropriate interventions. By systematically testing and documenting muscle function, healthcare providers can better assess the extent of brain injury and determine the most effective treatment strategies.
Evaluating Speech and NIH Scale
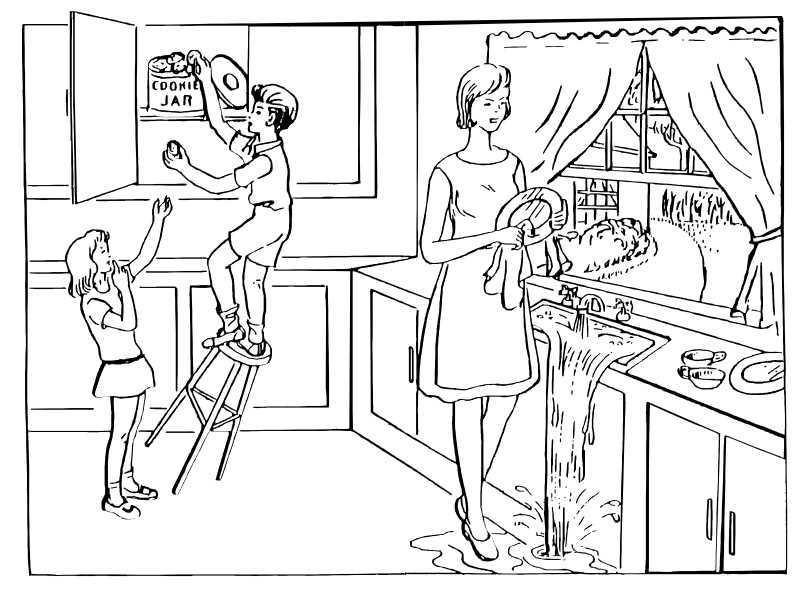
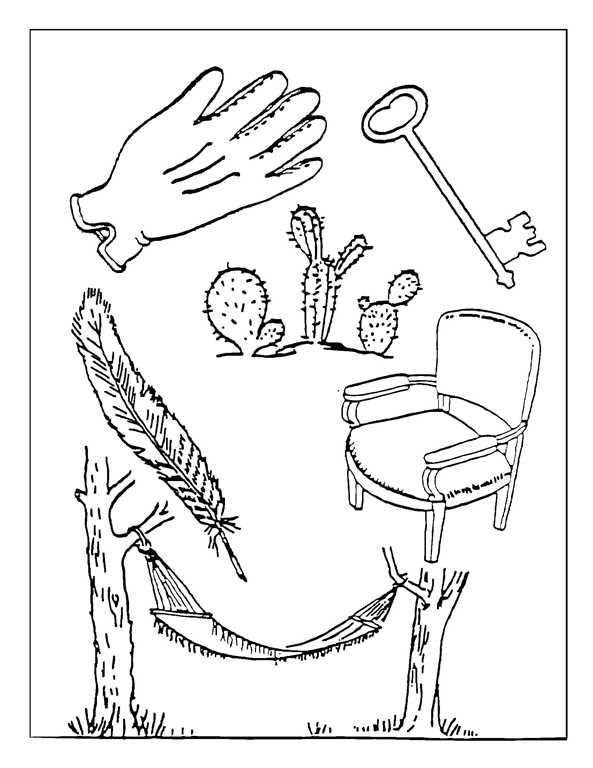
Assessing a patient’s ability to speak clearly and effectively is a crucial component of understanding neurological function. Speech difficulties can arise from damage to various areas of the brain, and evaluating these impairments helps determine the extent of the injury. Impairments in speech can range from mild slurring to complete inability to speak, and understanding these variations is key to gauging a patient’s condition and guiding treatment.
During the assessment, healthcare professionals focus on several key aspects of speech: clarity, articulation, fluency, and comprehension. A thorough evaluation includes listening for abnormal speech patterns, such as slurring or inability to form coherent sentences, which can indicate brain dysfunction. This assessment is critical in diagnosing and tracking the recovery process for those who have suffered neurological damage.
Key Areas of Speech Evaluation
- Articulation: Evaluate the patient’s ability to pronounce words clearly. Difficulty forming sounds may suggest motor issues affecting speech.
- Fluency: Listen for smoothness of speech. Hesitation, fragmented speech, or long pauses may indicate cognitive or motor impairment.
- Comprehension: Assess the patient’s ability to understand and respond appropriately to simple questions or commands. Impaired comprehension may signal deeper cognitive issues.
Speech Impairments and Severity Levels
- Mild impairment: The patient may exhibit slight slurring or difficulty with specific words but is still able to communicate effectively.
- Moderate impairment: Speech is noticeably unclear or disjointed, and the patient may have difficulty forming complete sentences or responding to questions.
- Severe impairment: The patient is unable to speak clearly or may be completely non-verbal, with significant difficulty expressing themselves.
- Non-verbal: Complete inability to communicate verbally, which may indicate profound neurological damage.
Accurately evaluating speech impairments is essential for diagnosing the underlying cause of neurological issues and determining appropriate rehabilitation strategies. Through careful observation and scoring, healthcare professionals can assess the degree of impairment and monitor progress over time.
Impact of Limb Movement on Scoring
Assessing limb movement is a critical aspect of evaluating a patient’s motor function and neurological health. The ability to move limbs, or the lack thereof, provides valuable insights into the severity of neurological impairment. When scoring motor function, movements of the arms and legs are carefully observed to determine whether they indicate weakness, paralysis, or normal function. These assessments are essential for understanding the extent of damage and guiding further clinical decisions.
Limb movement is graded based on the patient’s ability to perform voluntary actions. This includes testing for strength, coordination, and motor control, which can be impacted by damage to specific brain regions. Scoring the severity of limb movement impairment allows healthcare professionals to track recovery or deterioration over time, playing a pivotal role in treatment planning.
Grading Limb Movement
- Full movement: The patient is able to move the limbs normally, demonstrating full control and strength.
- Partial movement: The patient exhibits some ability to move the limb but struggles with coordination or strength.
- Minimal movement: The patient can make very limited or weak movements, indicating significant motor impairment.
- No movement: The patient is unable to move the limb at all, indicating total paralysis or severe motor dysfunction.
Evaluating Limbs for Symmetry and Coordination
- Symmetry: Assess both sides of the body to ensure equal strength and movement. Asymmetry often indicates a more severe issue on one side of the body.
- Coordination: Check for smoothness of motion. Jerky or uncoordinated movements can suggest neurological dysfunction.
- Strength: Apply resistance to assess the patient’s muscle strength and evaluate the level of weakness or paralysis.
Accurate scoring of limb movement provides critical information about the patient’s condition. This helps doctors evaluate the progression of the illness or injury and adjust treatments as needed. By focusing on both the range and quality of movement, clinicians can better understand the underlying neurological damage and provide more targeted interventions.
Eye Movement and Stroke Assessment
Eye movement plays a significant role in assessing neurological function, as it provides valuable insight into the health of the brain and nervous system. During an assessment, the ability to track, move, and control eye movements is tested to evaluate how well the brain and muscles are functioning. Impairments in eye movement can point to issues within specific regions of the brain that are responsible for controlling these actions, such as the brainstem and certain cranial nerves.
In patients with neurological conditions, abnormal eye movement patterns can reveal the severity of the condition and help identify which areas of the brain may be affected. The range of movement, coordination, and ability to follow visual stimuli are all assessed to understand the extent of any impairments. Proper evaluation of these movements is essential for accurate diagnosis and treatment planning.
Common abnormalities in eye movement may include difficulty focusing on objects, inability to track moving objects, or uncoordinated or jerky eye movements. These signs may indicate underlying neurological issues that require further investigation and intervention.
Importance of NIH Scale in Diagnosis
The ability to accurately assess neurological function is crucial for diagnosing and treating patients with brain injuries or disorders. Standardized tools that measure the severity of symptoms are essential for determining the extent of impairment and planning the most effective course of treatment. These tools allow healthcare professionals to quickly evaluate a patient’s condition, monitor changes over time, and make informed decisions based on objective data.
The standardized assessment system is particularly valuable in clinical settings where rapid decision-making is critical. By using a structured approach, clinicians can identify the most affected areas of the nervous system and determine the level of impairment. This method not only aids in diagnosing the condition but also plays a key role in tracking recovery, guiding rehabilitation efforts, and predicting outcomes.
One of the most significant advantages of using this evaluation method is its ability to provide consistent results across different medical professionals and institutions. It offers a reliable way to document a patient’s condition, ensuring that all healthcare providers are on the same page when making clinical decisions.
Practical Tips for Accurate Scoring
Accurate assessment of neurological function is crucial in clinical settings, and the ability to assign correct scores plays a key role in ensuring proper diagnosis and treatment. To achieve reliable results, it is important to follow specific guidelines and techniques during the evaluation. Consistency, attention to detail, and a systematic approach can help reduce errors and improve the accuracy of the scoring process.
One important tip is to ensure that the patient is relaxed and comfortable before beginning the assessment. This helps to avoid any external factors, such as anxiety or discomfort, that may influence the results. It’s also essential to take the time to observe the patient carefully and evaluate each response thoroughly, rather than rushing through the process. In addition, scoring should be based on the most accurate and consistent observations, avoiding assumptions or estimates based on incomplete information.
Another key factor is familiarity with the scoring criteria. The more familiar you are with the specific questions and scoring system, the more efficiently you can assess the patient’s condition. Repetition and practice help to improve confidence and minimize the risk of overlooking important details. Additionally, collaborating with other healthcare professionals for second opinions can ensure the reliability of the scoring process.
Common Challenges with NIH Stroke Exam
Assessing neurological function in patients can be a complex task, with various factors influencing the accuracy of the results. While standardized assessment tools provide a structured framework, several challenges can arise during the evaluation process. These challenges often stem from patient-specific conditions, external factors, or the difficulty of interpreting certain symptoms. Recognizing these common obstacles is key to improving the reliability of assessments and ensuring appropriate care.
One of the most frequent challenges is dealing with patients who are unable to fully cooperate due to confusion, weakness, or language barriers. This can make it difficult to gather accurate responses or assess certain physical functions. In these cases, healthcare professionals must rely on their clinical judgment and adjust their approach to obtain the most reliable information, sometimes through repeated or alternative methods of testing.
Another common difficulty involves the subjective nature of certain assessments. For example, evaluating speech, motor functions, or consciousness can vary depending on how questions are phrased or how patients react at the moment of assessment. Inconsistent results may occur if the evaluation is rushed or if the examiner has not thoroughly reviewed the scoring criteria. Thorough training and repeated practice can help reduce this variability and enhance the examiner’s confidence in the results.