
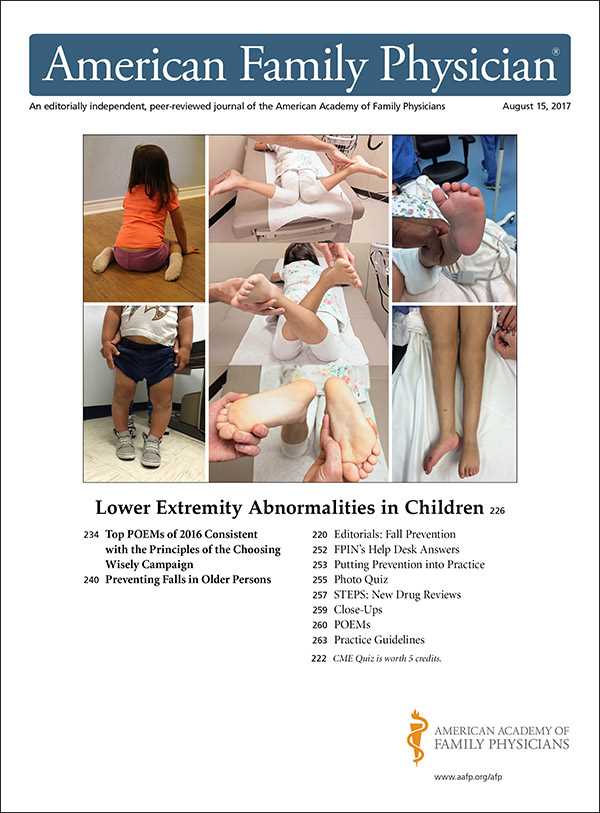
Understanding how to thoroughly assess the lower limb is critical in diagnosing various musculoskeletal issues. Effective evaluation techniques are essential for identifying injuries, ensuring proper treatment, and guiding rehabilitation efforts. This section delves into the recommended steps and strategies for conducting a thorough evaluation of the joint.
From performing basic mobility checks to more detailed tests for ligament and tendon health, each step plays a crucial role in determining the underlying cause of discomfort. Key methods used to assess joint integrity and functionality will be covered, as well as tips to avoid common pitfalls that could lead to misdiagnosis.
Whether you’re a healthcare professional or a student, mastering these procedures ensures that you can provide the most accurate care and support for your patients. A solid understanding of the assessment process not only aids in diagnosing but also enhances overall clinical practice.
Comprehensive Joint Assessment Overview

A thorough evaluation of the lower limb is fundamental in identifying underlying issues that may affect mobility and overall function. The process includes a combination of patient history, visual inspection, manual tests, and functional assessments to ensure a comprehensive approach. Understanding the specific techniques to evaluate each component is crucial for accurate diagnosis and treatment planning.
This section provides an overview of the essential steps and considerations when performing a full assessment. By following a systematic approach, healthcare providers can detect conditions ranging from soft tissue injuries to joint instability, ensuring proper care and rehabilitation strategies.
| Step | Purpose | Method |
|---|---|---|
| Patient History | Identify symptoms, previous injuries, and medical background | Ask targeted questions regarding pain, range of motion, and past events |
| Visual Inspection | Detect swelling, deformities, or abnormal posture | Examine the affected limb for signs of inflammation or asymmetry |
| Palpation | Assess for tenderness or structural abnormalities | Gently feel around the joint to locate areas of discomfort |
| Range of Motion | Evaluate flexibility and mobility | Guide the patient through movements to check for restrictions |
| Strength Testing | Assess muscle function and stability | Test muscle strength using resistance methods or manual force |
| Functional Tests | Determine impact on daily activities | Ask the patient to perform common movements or tasks |
By following these steps, healthcare providers can create a detailed understanding of the patient’s condition, leading to a more accurate diagnosis and effective treatment plan. Each component of the assessment contributes to a complete picture of joint health, ensuring the best possible outcome for the patient.
Importance of Joint Assessment in Healthcare
A thorough assessment of the lower extremities plays a vital role in diagnosing musculoskeletal issues, particularly those affecting mobility and quality of life. The ability to accurately evaluate and identify problems within the joints ensures that patients receive timely and effective treatment. A comprehensive examination helps healthcare providers pinpoint underlying causes of discomfort, leading to better clinical outcomes.
Early Detection and Prevention
By conducting regular assessments, medical professionals can detect conditions in their early stages, preventing more severe complications down the line. Early intervention can help manage symptoms, reduce pain, and improve functionality. Identifying underlying structural issues or soft tissue damage early can prevent long-term damage and improve recovery rates.
Enhancing Patient Care and Recovery
Proper evaluation not only aids in diagnosing but also plays a significant role in guiding treatment plans. With a clear understanding of a patient’s condition, healthcare providers can recommend personalized rehabilitation programs, physical therapy, or other interventions. This leads to more efficient recovery and ultimately enhances a patient’s ability to resume normal activities.
AAFP Recommendations for Joint Assessment
Comprehensive evaluation guidelines provided by leading medical organizations ensure that healthcare providers can accurately diagnose and address issues affecting lower limb function. These recommendations emphasize a systematic approach that includes both standard techniques and specialized tests to detect a wide range of musculoskeletal conditions. Following these guidelines enhances diagnostic accuracy and contributes to better patient outcomes.
Systematic Approach to Assessment
The recommended approach includes a thorough patient history review, careful observation of joint alignment, and palpation to detect areas of tenderness or swelling. Medical professionals are advised to incorporate functional movement assessments to evaluate how the joint performs under load and stress. This helps in identifying potential limitations or abnormal motion that may indicate injury or degeneration.
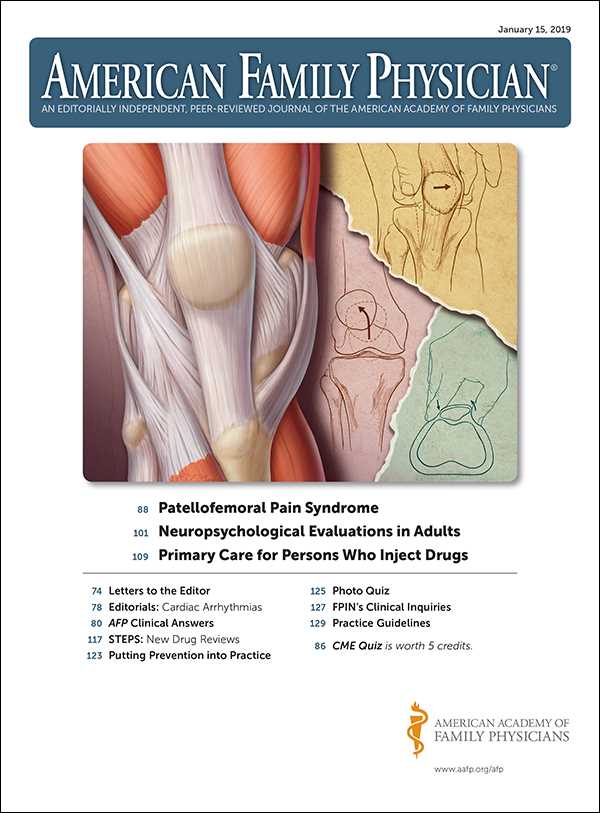
Specialized Tests for Joint Integrity
In addition to basic assessments, specific tests are recommended to evaluate the integrity of ligaments, tendons, and surrounding soft tissues. These tests help in detecting common injuries like sprains, strains, and tears. AAFP guidelines suggest that clinicians perform tests like stability checks and stress maneuvers to better understand the full extent of the damage and determine the best course of action for treatment.
Key Steps in Performing a Joint Assessment

To ensure a thorough and accurate evaluation of the lower limb, a systematic approach must be followed. Each step plays a critical role in identifying potential issues and providing a clear picture of the patient’s condition. By focusing on the right methods and maintaining a structured process, healthcare professionals can confidently diagnose musculoskeletal disorders and injuries.
- Patient History: Begin by gathering detailed information on the patient’s symptoms, past injuries, and relevant medical background. This information helps guide the examination process and identifies potential areas of concern.
- Visual Inspection: Observe the joint for any signs of swelling, redness, or deformities. This helps in identifying surface-level issues such as inflammation or misalignment.
- Palpation: Use your hands to gently feel around the joint, assessing for tenderness, warmth, or abnormal structures. This can help detect soft tissue injuries, such as sprains or strains.
- Range of Motion (ROM) Testing: Ask the patient to move the joint through its full range of motion. Limited or painful movements may indicate underlying issues such as arthritis or ligament damage.
- Strength Testing: Assess the muscle strength around the joint by applying resistance while the patient performs specific movements. This will highlight any weakness or imbalances that might be contributing to the problem.
- Special Tests: Perform specific maneuvers designed to test the stability of ligaments and other soft tissues, such as drawer tests or pivot shifts, to assess for injuries like tears or sprains.
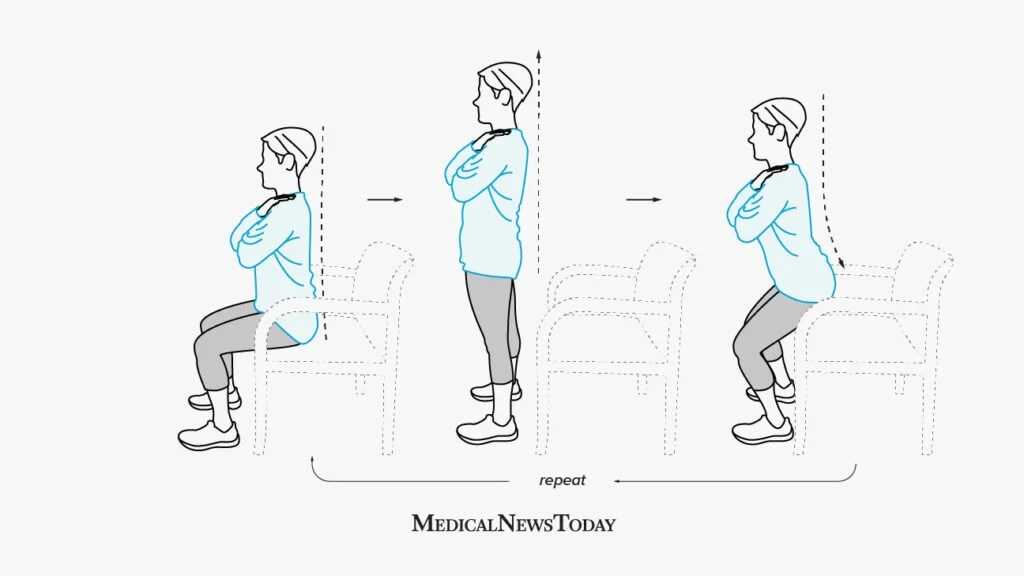
- Functional Movement Assessment: Ask the patient to perform functional tasks, such as walking, squatting, or jumping, to evaluate how the joint performs under load and stress.
By carefully following these steps, healthcare professionals can ensure a comprehensive evaluation that will lead to a more accurate diagnosis and effective treatment plan.
Identifying Common Joint Injuries
Injuries affecting the lower limb can vary greatly in severity and type. Recognizing the symptoms and understanding the potential causes is essential for effective diagnosis and treatment. This section outlines common conditions that may be encountered during an assessment, helping clinicians identify specific injuries based on patient presentation and clinical findings.
Common Soft Tissue Injuries
Soft tissue injuries are among the most frequently observed conditions in the lower limb. These can involve muscles, tendons, or ligaments, and they often result from trauma, overuse, or improper movement patterns.
- Sprains: Ligament injuries caused by overstretching or tearing. Symptoms include swelling, instability, and pain during movement.
- Strains: Injuries to muscles or tendons, often resulting from sudden movements or overexertion. These injuries typically cause pain, weakness, and limited mobility.
- Contusions: Bruises that occur when blood vessels under the skin break due to direct impact. These injuries are marked by discoloration and tenderness.
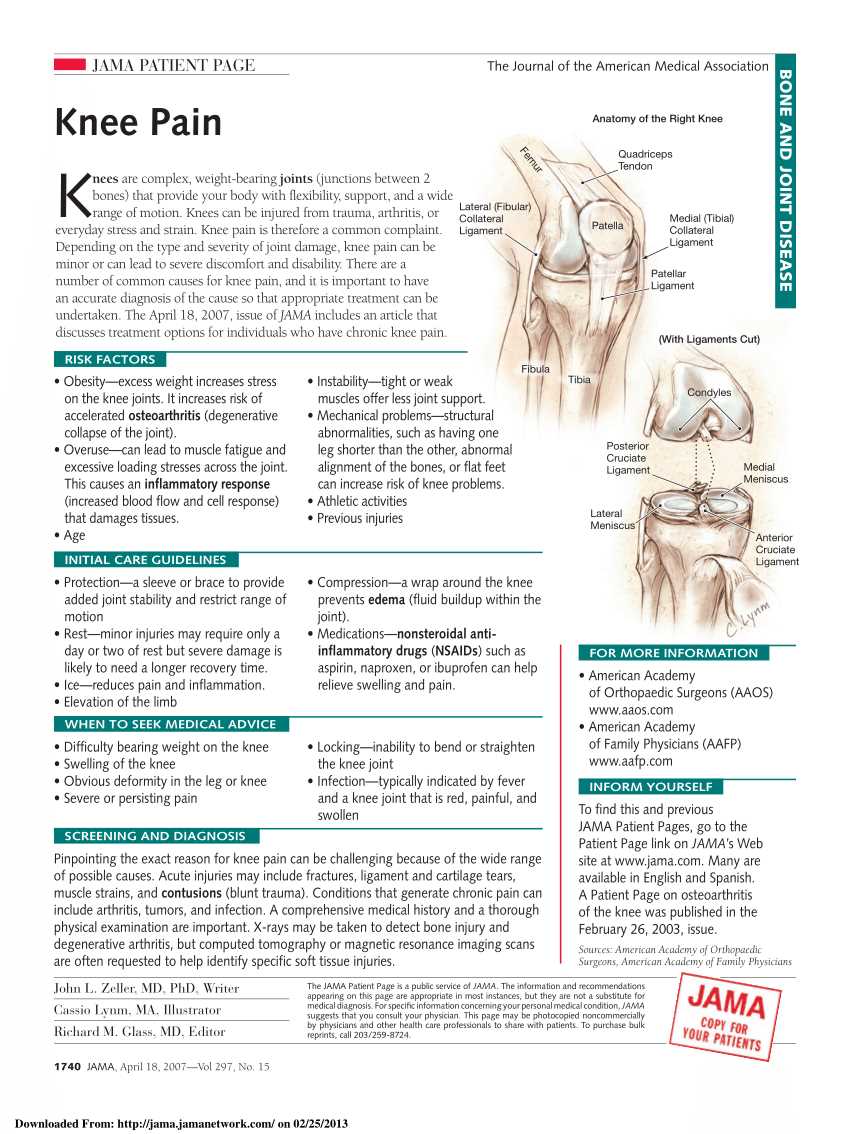
Bone and Joint Injuries
Bone fractures and joint issues often arise from traumatic events or prolonged wear and tear. Identifying these injuries requires careful examination and, in some cases, imaging for confirmation.
- Fractures: Breaks or cracks in the bone caused by high-impact trauma or stress. Symptoms include severe pain, swelling, and an inability to move the affected area.
- Dislocations: When bones in a joint are forced out of their normal position. This can cause extreme pain, visible deformity, and loss of function in the joint.
- Arthritis: Inflammation of the joint that can result from long-term wear and tear, causing pain, stiffness, and swelling. This condition is often diagnosed in older adults.
Recognizing these injuries early allows for prompt and appropriate management, ensuring the best possible outcomes for recovery. Understanding the common signs and symptoms associated with each condition helps guide the examination process and the selection of appropriate diagnostic tests and treatment plans.
Best Practices for Joint Range of Motion
Assessing the full range of motion of the lower extremity is a critical component of a comprehensive evaluation. This step helps identify limitations or abnormalities in movement that could indicate underlying issues, such as stiffness, pain, or structural damage. A careful and consistent approach to measuring range of motion ensures accurate results and guides the overall treatment strategy.
To achieve the most reliable findings, it is essential to follow established guidelines and techniques when evaluating mobility. Proper technique not only improves diagnostic accuracy but also minimizes discomfort for the patient during the assessment.
- Patient Preparation: Ensure the patient is relaxed and comfortable before starting the assessment. Ask them to perform movements slowly and within a pain-free range to avoid injury.
- Passive vs. Active Range: Measure both passive and active movements. Passive range refers to the motion the joint can achieve with assistance, while active range is the patient’s ability to move the joint independently.
- Use of Goniometer: A goniometer is a precise tool used to measure angles during joint movement. Ensure the device is aligned correctly with the joint to capture accurate measurements.
- Consistent Technique: Always measure the same movements in the same order for consistency. Document the range in both flexion and extension, noting any discomfort or limitations.
- Comparative Measurements: If applicable, compare the affected joint with the unaffected side to detect any asymmetry or significant restriction in motion.
Proper assessment of joint mobility not only identifies potential impairments but also provides crucial information that can inform rehabilitation strategies, such as targeted physical therapy exercises. This practice helps to optimize movement and alleviate pain, improving the patient’s functional capacity over time.
How to Evaluate Joint Stability
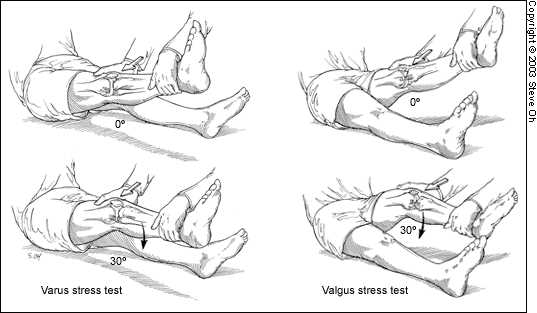
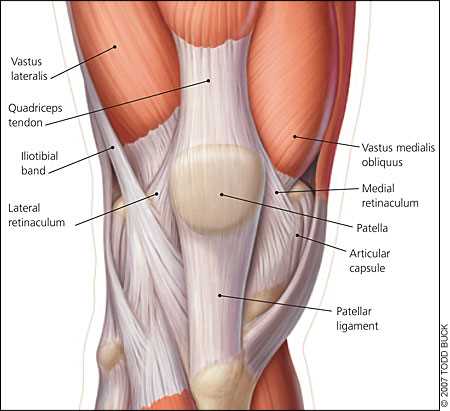
Assessing the stability of the lower extremity is essential in determining the integrity of its structures, such as ligaments and tendons. Joint instability can be caused by trauma, overuse, or degenerative conditions, and can significantly affect a patient’s mobility and function. A proper evaluation of stability is crucial to diagnose the underlying issues and guide appropriate treatment options.
The evaluation process involves specific maneuvers and tests designed to assess the resilience of the joint’s supporting structures. These tests help to determine the degree of instability, whether it’s related to ligament injuries, dislocations, or other mechanical issues.
- Anterior Drawer Test: This test evaluates the stability of the front ligaments by applying pressure to the joint while the patient is in a relaxed position. An abnormal result may suggest a tear or sprain in the supporting ligaments.
- Posterior Drawer Test: Similar to the anterior test, this maneuver assesses the stability of the posterior ligaments. A lack of resistance or abnormal movement may indicate an issue with the ligament’s integrity.
- Lachman Test: This is a sensitive test used to assess the stability of the primary stabilizing ligaments. The test involves applying gentle forward pressure to the joint to determine how stable it remains under stress.
- Varus and Valgus Stress Tests: These tests evaluate the stability of the medial and lateral sides of the joint by applying pressure in both directions. Any abnormal movement can indicate ligament damage or laxity.
Evaluating joint stability through these methods ensures a comprehensive understanding of the integrity of the joint structures, which is key to diagnosing conditions such as sprains, tears, or degenerative disorders. Proper diagnosis enables clinicians to create effective treatment plans tailored to the patient’s specific needs and recovery goals.
Assessing Ligament and Tendon Integrity
Evaluating the condition of the ligaments and tendons surrounding the joint is crucial for diagnosing injuries that affect the stability and function of the lower extremity. Ligaments and tendons play an essential role in joint movement and support, and any compromise in their integrity can lead to pain, instability, and long-term functional limitations. A careful assessment helps identify sprains, tears, or other damage, allowing for timely and effective treatment.
Injury to these structures often results from trauma, overuse, or sudden movement. Healthcare professionals can evaluate their integrity through specific tests that place stress on the ligaments and tendons to detect any abnormal movement or resistance. These tests are vital for pinpointing the exact location and severity of the injury, and they guide the development of rehabilitation or surgical intervention plans.
- Palpation: Gently feeling the area around the joint can help identify any abnormal swelling, tenderness, or bumps that may indicate tendonitis or ligament strain.
- Ligament Stability Tests: These tests, such as the Lachman or drawer tests, are designed to stress the ligaments and assess for any signs of tears or laxity. A positive result often indicates significant ligament damage.
- Movement Testing: Evaluating the range of motion under stress can provide insights into tendon flexibility and ligament stability. Limited motion or pain during movement can suggest tendon or ligament injury.
- Strength Testing: Applying resistance during movement helps assess the strength of the muscles and tendons around the joint. Weakness or pain during this phase may point to tendon damage.
Assessing ligament and tendon integrity accurately is essential for determining the appropriate treatment approach, whether it involves rest, physical therapy, or more advanced interventions such as surgery. Early detection and intervention can significantly improve recovery outcomes and restore normal function.
Role of Palpation in Joint Assessment
Palpation is a key technique in physical examinations, allowing clinicians to gather vital information about the condition of the structures surrounding the joint. This hands-on approach helps detect tenderness, swelling, and abnormal masses, which may indicate underlying injuries or conditions. By applying pressure in different areas, the examiner can identify areas of discomfort or irregularities that are not always visible but may be crucial for an accurate diagnosis.
Identifying Areas of Tenderness

One of the primary purposes of palpation is to locate specific areas where the patient experiences pain. These areas can reveal the presence of inflammation, muscle strains, or ligament sprains. By gently pressing on various parts of the joint, the healthcare provider can assess the level of discomfort and identify whether the pain is localized or diffused, which provides valuable insight into the type of injury or condition present.
Detecting Abnormalities and Swelling
Swelling and abnormal masses can indicate serious issues such as infections, cysts, or joint effusion. Through palpation, the examiner can assess the consistency, temperature, and texture of the affected area. Unusual warmth, firm masses, or uneven swelling can point to conditions such as bursitis or tendinitis, helping to direct further testing or treatment options.
Overall, palpation is an essential part of any joint assessment, providing a hands-on method for identifying issues that may not be immediately obvious through visual inspection or basic movement tests. It helps build a more complete picture of the patient’s condition and ensures that the appropriate course of action is taken.
Common Joint Assessment Errors to Avoid
During any physical assessment, accurate technique is essential for obtaining reliable results. Mistakes in performing tests can lead to incorrect diagnoses, unnecessary treatments, or missed conditions. It is crucial to avoid common errors to ensure the examination is thorough, consistent, and effective. Small missteps in technique or interpretation can significantly affect the outcome of the evaluation process.
Improper Patient Positioning
One of the most common mistakes is failing to position the patient correctly before starting the assessment. Incorrect positioning can result in inaccurate readings and may cause discomfort or pain for the patient. It is vital to ensure that the joint is in a relaxed and neutral position, allowing for a comprehensive evaluation of its range of motion and stability. Always ensure the patient is comfortable and the joint is appropriately aligned to facilitate an accurate assessment.
Inconsistent Pressure Application
Applying inconsistent pressure during palpation or other tests can lead to unreliable results. Whether testing for ligament integrity or assessing tenderness, varying the force used can impact the assessment’s accuracy. Always apply a consistent, gentle pressure to evaluate the joint correctly. Inconsistent pressure may either fail to reveal underlying issues or cause unnecessary discomfort to the patient.
Neglecting to compare sides is another frequent error. When assessing a joint, it is important to compare the affected side with the unaffected side to detect any asymmetry. Ignoring this step can lead to missing subtle differences in range of motion or tenderness that may be critical in diagnosing an injury or condition.
Avoiding these common errors is key to performing a thorough and reliable joint assessment. By ensuring proper positioning, consistent technique, and careful comparison, healthcare providers can obtain accurate findings that lead to effective treatment and better patient outcomes.
Diagnostic Tests for Joint Conditions
Accurate diagnosis of joint-related issues often requires more than just a physical assessment. Diagnostic tests play a vital role in identifying underlying causes of pain, instability, or dysfunction. These tests help confirm the presence of conditions such as tears, arthritis, or infections, and guide healthcare providers in formulating effective treatment plans. Through imaging, laboratory tests, and specialized procedures, clinicians can gather detailed information that isn’t always visible during an initial examination.
Imaging Techniques
Imaging is one of the most common diagnostic tools used to visualize joint structures and detect abnormalities. Techniques such as X-rays, MRIs, and CT scans allow healthcare professionals to examine bones, cartilage, ligaments, and tendons in detail. These tools help identify fractures, misalignments, joint effusion, and degenerative changes that may not be apparent through physical testing alone. For example, MRIs are particularly useful in evaluating soft tissue injuries, while X-rays can reveal bone fractures or arthritis.
Arthroscopy
In cases where non-invasive tests do not provide sufficient information, arthroscopy can be used. This minimally invasive procedure involves inserting a small camera into the joint to directly visualize its interior. Arthroscopy allows for both diagnosis and treatment, as it can also be used to remove damaged tissue or repair torn structures. It is often used when other diagnostic methods fail to provide conclusive results, particularly for complex joint conditions.
These diagnostic tests, when used in conjunction with a thorough physical evaluation, provide comprehensive insights into the patient’s condition. They are essential for identifying the specific cause of symptoms and guiding healthcare providers toward the most appropriate treatment strategies.
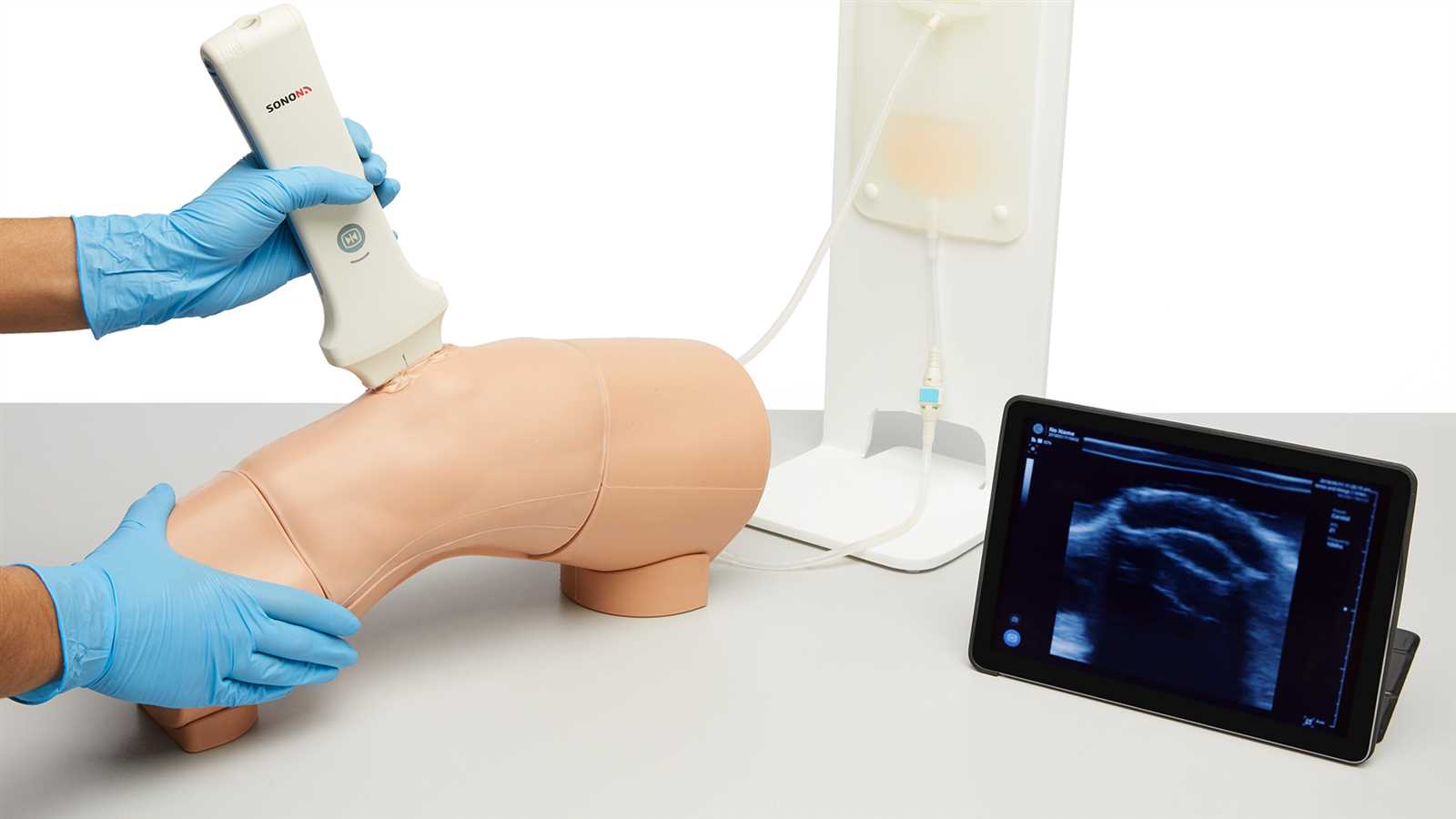
Using Imaging in Joint Assessments
Imaging techniques have revolutionized the way healthcare providers assess joint health, offering a clearer view of the internal structures that might not be visible during a physical examination. These technologies are essential for diagnosing injuries, degenerative conditions, and other abnormalities. By utilizing advanced imaging methods, clinicians can obtain detailed images of bones, cartilage, ligaments, and tendons, which assist in creating accurate treatment plans and improving patient outcomes.
Common Imaging Techniques
Several imaging modalities are commonly used in joint assessments, each with its unique advantages and limitations. Below are some of the most frequently employed techniques:
- X-rays: Primarily used for evaluating bone fractures, joint alignment, and signs of arthritis. X-rays are quick, widely available, and helpful in detecting structural issues.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues like cartilage, ligaments, and tendons. MRIs are particularly useful for detecting tears, sprains, or inflammation that might not be visible on X-rays.
- CT Scans (Computed Tomography): Combines X-ray images from multiple angles to create cross-sectional views of the joint, offering more detailed information than standard X-rays. CT scans are helpful in assessing bone fractures or complex joint injuries.
Advantages of Imaging in Assessments
Using imaging in joint assessments offers several benefits, including:
- Improved Diagnosis: Imaging provides a clearer understanding of internal joint structures, allowing for more accurate identification of injuries or conditions.
- Non-invasive: These techniques do not require surgery or other invasive procedures, making them safer and more comfortable for patients.
- Guiding Treatment Decisions: By identifying the exact nature of a problem, imaging helps healthcare providers determine the most effective treatment plan, whether it involves physical therapy, medication, or surgical intervention.
Overall, imaging plays a critical role in joint assessments, offering essential insights that complement physical evaluations and enabling more precise diagnoses and better patient care.
How to Handle Joint Pain Complaints
When patients report discomfort in the joints, particularly those that bear weight, it’s essential to approach the situation with a thorough and methodical strategy. Joint pain, especially in weight-bearing areas, can arise from various causes such as inflammation, injury, or degenerative diseases. A proper assessment, along with an understanding of the patient’s medical history and lifestyle, is crucial for determining the right course of action. Addressing these complaints effectively requires a combination of diagnostic insight, patient communication, and appropriate treatment options.
Initial Assessment and Considerations
When a patient presents with joint discomfort, the initial evaluation should focus on understanding the nature and intensity of the pain, as well as its duration and triggers. Key questions to ask include:
- When did the pain start, and how long has it been present?
- Does the pain occur during activity, at rest, or both?
- Is the pain associated with any specific movements or positions?
- Has there been any history of injury or trauma to the affected area?
- Are there any other symptoms, such as swelling, warmth, or redness?
Additionally, a physical examination is necessary to check for any visible signs of damage, such as swelling or bruising, and to assess the range of motion and stability of the joint.
Treatment and Pain Management
Once the cause of the pain is identified, treatment options can be discussed with the patient. These may include:
| Treatment Option | Description |
|---|---|
| Rest and Ice | For acute pain, reducing activity and applying ice can help alleviate swelling and provide temporary relief. |
| Physical Therapy | Exercises to strengthen the muscles around the joint, improve flexibility, and restore function. |
| Medications | Non-steroidal anti-inflammatory drugs (NSAIDs) or other pain relievers to manage inflammation and discomfort. |
| Surgical Intervention | If conservative measures fail, surgical procedures may be necessary to repair damaged tissues or alleviate chronic pain. |
In some cases, additional diagnostic tests may be required to confirm the cause of the pain. A follow-up plan should also be put in place to monitor progress and adjust treatment strategies as needed.
By taking a structured approach to joint pain complaints, healthcare providers can ensure that patients receive the appropriate care tailored to their specific needs, helping to reduce pain and improve overall function.
Physical Therapy’s Role in Joint Recovery
Physical therapy plays a pivotal role in the rehabilitation of individuals recovering from joint injuries or surgeries. Its primary goal is to restore function, alleviate pain, and enhance mobility through targeted exercises and specialized treatments. By addressing both the strength and flexibility of the muscles surrounding the joint, therapy helps to promote healing, prevent further damage, and improve overall quality of life. Whether recovering from an acute injury or managing a chronic condition, physical therapy is often an integral part of the recovery process.
Key Components of Physical Therapy
Physical therapy for joint recovery typically involves several stages, each designed to progressively improve the patient’s condition. The treatment plan is customized based on the severity of the injury, the patient’s goals, and their overall health. Below are some of the key components:
| Component | Description |
|---|---|
| Strengthening Exercises | These exercises target the muscles that support the affected joint, improving strength and stability. Strengthening helps reduce stress on the joint and improves overall movement. |
| Range of Motion Exercises | These exercises focus on enhancing flexibility and restoring the full movement of the joint. Increased mobility helps in performing daily activities with less pain and discomfort. |
| Manual Therapy | Physical therapists may use hands-on techniques to manipulate soft tissues and joints, improving movement and reducing pain. |
| Functional Training | This phase of therapy emphasizes exercises that simulate everyday movements, ensuring the patient can return to normal activities safely. |
Benefits of Physical Therapy in Recovery
The benefits of physical therapy extend far beyond pain relief. Some of the most notable advantages include:
- Improved Mobility: By restoring range of motion and flexibility, physical therapy enables patients to move more freely and comfortably.
- Prevention of Future Injuries: Targeted exercises help stabilize the joint, reducing the likelihood of further damage or re-injury.
- Pain Management: Physical therapy techniques such as stretching and manual therapy can help alleviate discomfort and promote long-term relief.
- Increased Independence: Through strength-building and functional training, patients are better able to manage daily tasks without assistance.
Incorporating physical therapy into a treatment plan is essential for ensuring a successful and lasting recovery. By addressing the root causes of pain and dysfunction, it offers a comprehensive approach to joint rehabilitation that supports both short-term healing and long-term health.
When to Refer a Joint Patient

Knowing when to refer a patient to a specialist is a critical aspect of providing comprehensive care for individuals experiencing joint discomfort or dysfunction. While many cases can be effectively managed with initial interventions, certain situations require the expertise of an orthopedic or rheumatology specialist. Recognizing the signs that warrant a referral ensures that patients receive the appropriate level of care and reduces the risk of complications in the future.
Indicators for Referral
There are several key signs and symptoms that suggest a patient may benefit from a referral. These may include:
- Unresolved Pain: When pain persists despite conservative treatments, further evaluation by a specialist may be necessary to determine the underlying cause.
- Severe Instability: If the joint is unstable and causes significant difficulty with weight-bearing activities, referral to an expert in musculoskeletal disorders is advised.
- Inability to Bear Weight: If the patient experiences significant difficulty walking or standing, further diagnostic imaging and consultation may be needed.
- Limited Range of Motion: Significant restrictions in joint mobility that do not improve with rehabilitation should be assessed by a specialist.
- Joint Deformity: Any noticeable changes in the joint’s structure, such as swelling, malalignment, or visible deformities, warrant further medical evaluation.
When to Consider Surgical Consultation
In some cases, patients may require surgical intervention. Referral to a surgeon is appropriate when:
- Chronic or Severe Conditions: When conservative treatments fail to provide relief for degenerative conditions, surgery may become a necessary option.
- Acute Injury: For cases involving fractures, ligament tears, or tendon ruptures, early referral to a specialist can help determine whether surgery is required for repair.
- Progressive Damage: If the joint shows signs of progressive damage or deterioration, a surgical approach may be considered to restore function or relieve pain.
Referring a patient at the right time is essential to ensure they receive timely and effective care, ultimately improving their quality of life and minimizing long-term complications.
Continuing Education for Joint Evaluation Skills
Maintaining and enhancing diagnostic proficiency in joint assessments is an ongoing process for healthcare professionals. With the evolving nature of medical practices and the introduction of advanced techniques, continuous learning plays a crucial role in ensuring accurate evaluations and effective treatment. Practitioners need to stay informed about the latest methodologies, tools, and clinical guidelines to provide the highest level of care to their patients.
Importance of Ongoing Training
There are several key reasons why ongoing education is essential for professionals involved in joint evaluations:
- Advances in Techniques: New diagnostic approaches and technologies are continually being developed, and staying updated ensures practitioners can provide the most accurate assessments.
- Improved Diagnostic Accuracy: Regular training helps professionals refine their skills, reducing the likelihood of misdiagnosis and improving overall patient outcomes.
- Adaptation to Emerging Guidelines: Clinical guidelines are regularly updated based on new research findings. Professionals who keep abreast of these changes can apply the most current evidence-based practices.
- Enhanced Patient Care: By continually honing assessment skills, healthcare providers can offer more personalized and effective treatments, leading to better recovery and management of conditions.
Methods for Continuing Education

Healthcare providers can pursue various methods to continue their education and develop expertise in joint evaluations:
- Workshops and Conferences: Attending hands-on workshops and specialized conferences allows practitioners to learn directly from experts and observe new techniques in practice.
- Online Courses and Webinars: Many platforms offer online courses that focus on specific areas of joint evaluation, allowing for flexible learning that fits into a busy professional schedule.
- Clinical Supervision and Peer Review: Engaging in case reviews with colleagues and mentors helps improve diagnostic skills by discussing challenging cases and receiving feedback.
- Research and Literature Review: Staying updated on the latest studies and clinical trials related to musculoskeletal health helps professionals apply the most current evidence to their practice.
Incorporating continuing education into a healthcare professional’s career development ensures they remain adept in their field and capable of providing the highest quality care to patients with joint concerns.