In the process of becoming a certified emergency responder, individuals must demonstrate their ability to perform under pressure in a range of critical situations. These assessments are designed to test both technical knowledge and practical skills, ensuring candidates are equipped to handle real-world emergencies effectively. Understanding the structure and expectations of these evaluations is crucial for success.
During these assessments, candidates face various simulated emergencies, where they must apply their knowledge, make quick decisions, and provide appropriate care. Each test scenario requires a unique approach, whether it involves managing trauma, performing life-saving interventions, or communicating with patients under stress. Mastery of these challenges requires thorough preparation and a clear understanding of the key competencies that will be tested.
Effective practice and repetition in realistic settings allow individuals to build the confidence needed to excel in these high-pressure situations. Proper technique, attention to detail, and the ability to stay calm are essential for passing these evaluations and ultimately providing the best care possible in emergency situations.
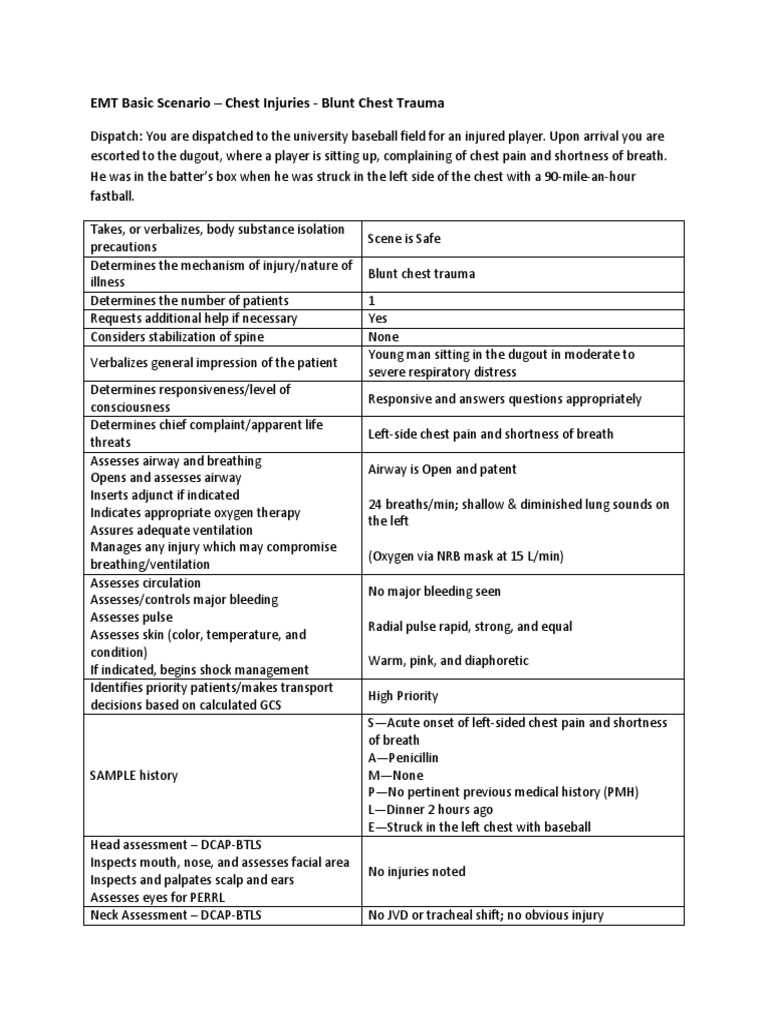
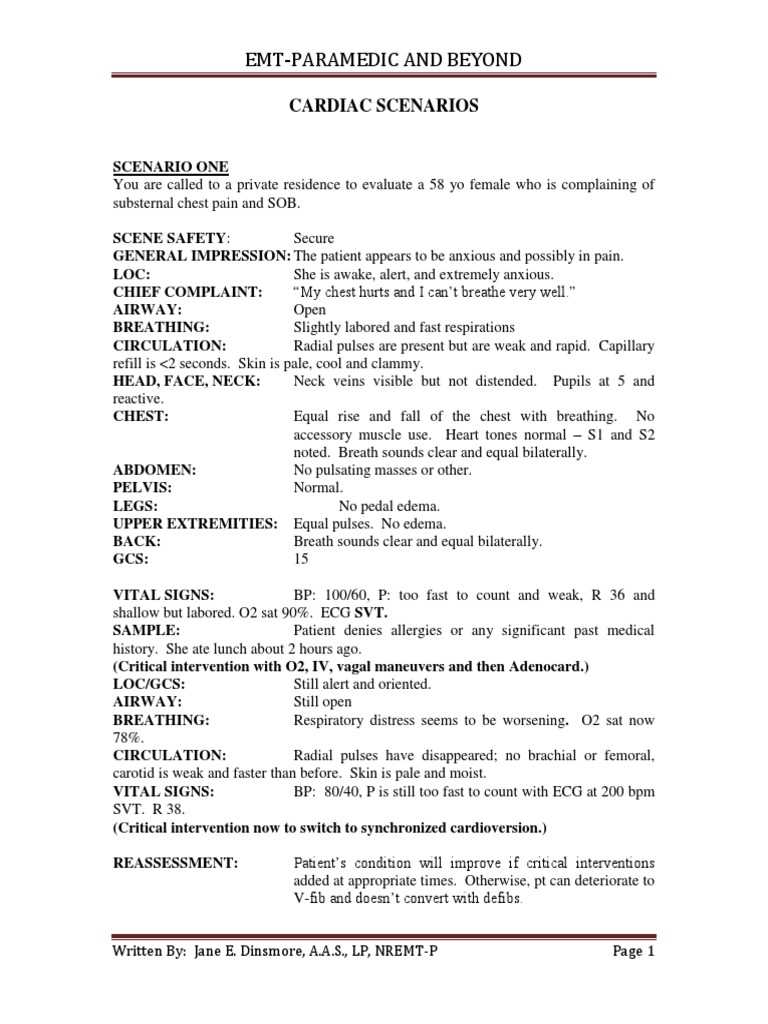
EMT Practical Exam Scenarios
In emergency responder assessments, candidates face a variety of simulated situations where they must demonstrate their ability to react effectively under pressure. These situations test a range of skills, from clinical knowledge to decision-making and communication. Success depends on not only technical proficiency but also the ability to stay calm and focused in high-stress environments.
Each simulation presents a unique set of challenges that require candidates to apply learned skills in real-time. Responding appropriately to a variety of emergencies–whether trauma, medical, or environmental–ensures that candidates are prepared for any situation they may encounter on the job. Structured preparation and practice are key to mastering these challenges.
Key Elements Tested in Simulations
Assessments typically focus on essential elements such as patient assessment, airway management, and life-saving techniques. Candidates must be able to quickly assess a patient’s condition and decide on the best course of action. This includes knowing when to administer interventions and how to manage any equipment involved in treatment.
Responding Under Pressure
The ability to remain composed during critical moments is another key aspect of these assessments. In many situations, time is of the essence, and candidates must demonstrate efficient decision-making and clear communication with their team. Being able to stay focused and prioritize actions in a high-pressure environment is essential for ensuring the best possible outcomes for patients.
Understanding the EMT Practical Exam
The certification process for emergency responders involves a comprehensive evaluation where candidates must demonstrate their readiness to handle a variety of emergency situations. This assessment is designed to test both technical abilities and decision-making under pressure, ensuring that individuals are capable of performing their duties effectively in the field. Understanding the structure and expectations of the evaluation is crucial for proper preparation and success.
These assessments typically involve multiple testing stations, each focusing on a specific aspect of emergency care. Candidates are required to perform tasks such as assessing patients, providing life-saving interventions, and communicating with both patients and team members. Each station is meant to simulate real-life conditions and test how well candidates can apply their knowledge and skills under stress.
| Assessment Focus | Skills Tested |
|---|---|
| Patient Assessment | Physical examination, medical history taking, vital signs |
| Airway Management | Techniques for maintaining and securing airways |
| Trauma Response | Stabilization, wound care, transport techniques |
| Team Communication | Clear instructions, delegation, patient handoff |
Successfully completing this process requires not only strong technical knowledge but also the ability to remain composed and think critically in high-pressure environments. Candidates must be prepared to show their competence in various emergency care situations, ensuring they can provide the best possible outcomes for patients in the field.
Key Skills Tested in EMT Scenarios
In emergency responder assessments, individuals are tested on a variety of skills that are essential for providing efficient and effective care during critical situations. These evaluations focus on both the technical aspects of emergency response and the ability to perform under pressure. Mastering these core skills is necessary for ensuring patient safety and successful outcomes in real-world emergencies.
Core Competencies Evaluated
The following abilities are crucial for success during the testing process:
- Patient Assessment: Quickly and accurately evaluating a patient’s condition to determine the appropriate course of action.
- Airway Management: Ensuring that the patient’s airway is open and maintaining oxygen flow using various techniques and equipment.
- Medical Interventions: Administering necessary medications and performing interventions based on the patient’s needs.
- Trauma Care: Stabilizing patients with injuries, controlling bleeding, and applying first aid techniques effectively.
- Team Coordination: Communicating clearly and effectively with other team members, delegating tasks, and ensuring everyone is working in sync.
Decision-Making Under Stress
In addition to technical skills, the ability to make quick decisions in high-pressure situations is vital. Candidates are evaluated on how well they can prioritize actions, stay calm under stress, and adapt to rapidly changing circumstances. The following aspects are commonly tested:
- Critical Thinking: Assessing the situation quickly and determining the best course of action in emergency conditions.
- Time Management: Managing time effectively to ensure that patient care is provided in a timely manner.
- Adaptability: Adjusting to unexpected complications or challenges during the response process.
Common Mistakes to Avoid in Exams
During evaluations for emergency responders, candidates often face challenges that can lead to mistakes, especially when working under pressure. While these assessments are designed to test one’s skills and knowledge, they also provide an opportunity to demonstrate professionalism and composure. Avoiding common errors can make the difference between success and failure, ensuring that candidates are able to showcase their true capabilities.
It is important to recognize typical pitfalls and learn how to prevent them. A lack of preparation, poor communication, and failure to follow proper procedures are frequent issues that candidates must overcome. Understanding the common mistakes can help candidates stay focused and perform at their best during critical moments.
| Mistake | Consequence | How to Avoid |
|---|---|---|
| Inadequate Patient Assessment | Missing vital signs or symptoms that could impact treatment. | Practice comprehensive assessment techniques to ensure all areas are checked. |
| Failure to Communicate Effectively | Team confusion, delayed treatment, and poor patient outcomes. | Ensure clear, concise, and timely communication with team members. |
| Ignoring Protocols | Providing incorrect treatment or missing necessary interventions. | Study and memorize protocols to ensure adherence during situations. |
| Overlooking Time Management | Delaying interventions that could affect patient survival. | Practice prioritizing tasks and managing time effectively in high-pressure situations. |
| Getting Distracted by Stress | Loss of focus, leading to poor decision-making and errors in care. | Develop techniques for staying calm and focused under stress. |
By being aware of these common mistakes and taking steps to avoid them, candidates can perform with greater confidence and competence. Preparation, practice, and mental discipline are key components for success in these assessments, ultimately leading to more effective emergency response in real-world situations.
Preparing for Cardiac Arrest Situations
Cardiac arrest is one of the most critical emergencies that require immediate and precise action. In these situations, every second counts, and the ability to act swiftly and accurately can determine whether the patient survives. Preparing for such high-stakes events involves mastering several key techniques and understanding the sequence of interventions that need to be performed under pressure. The ability to stay calm and focused is just as important as the technical skills needed to perform life-saving measures effectively.
Responders must be familiar with the latest guidelines for resuscitation, which typically include early defibrillation, high-quality chest compressions, and proper ventilation. Understanding the importance of each step and how to prioritize actions when faced with limited time and resources is essential. Rehearsing these procedures regularly and being able to perform them without hesitation is vital for success in these high-stress situations.
Additionally, maintaining effective communication with other team members during a cardiac arrest event is crucial. Clear delegation of tasks, quick decision-making, and coordinating efforts can significantly improve patient outcomes. Through regular practice and continual learning, responders can increase their confidence and competence when faced with a cardiac arrest emergency.
Handling Trauma Cases Effectively

Trauma cases present unique challenges that require quick, decisive action and the ability to assess and treat injuries efficiently. When responding to a trauma situation, the primary goal is to stabilize the patient, control bleeding, and address life-threatening conditions. The ability to think critically and perform necessary interventions in a timely manner can greatly impact the outcome of the case.
Key steps in handling trauma situations involve a systematic approach to patient care. The following steps are crucial for effective management:
- Initial Assessment: Quickly assess the patient’s condition to identify immediate threats such as airway obstruction, severe bleeding, or spinal injuries.
- Airway Management: Ensure the airway is open and clear, and use appropriate techniques to maintain it if necessary.
- Hemorrhage Control: Apply pressure to wounds, use tourniquets if needed, and ensure that blood loss is minimized.
- Stabilization: Keep the patient still to prevent further injury, especially when spinal trauma is suspected.
- Transport Decision: Determine the appropriate method of transport based on the severity of the injuries and available resources.
In addition to these technical steps, clear communication with other team members is essential for coordinating care. Delegating tasks and ensuring that everyone is on the same page will lead to more effective treatment and a higher chance of positive outcomes for the patient.
Being well-prepared for trauma cases involves not only knowing how to apply medical interventions but also staying composed in high-pressure environments. Regular training and simulation exercises can help build the confidence and skills necessary to manage these emergencies successfully.
Airway Management in EMT Scenarios
Effective airway management is a critical skill in emergency care, as it directly impacts a patient’s ability to breathe and survive. In many emergencies, airway obstruction can lead to life-threatening consequences if not addressed promptly. The ability to quickly assess, clear, and secure the airway is essential for ensuring that oxygen reaches the lungs and circulates throughout the body.
Airway management involves a series of steps and techniques, from basic interventions such as positioning the patient to more advanced methods like intubation and the use of airway adjuncts. Each situation may require a different approach depending on the patient’s condition, and responders must be prepared to adapt their methods as needed. In addition, the importance of maintaining a patent airway throughout the entire care process cannot be overstated, as it affects all subsequent medical interventions.
Common techniques used in airway management include:
- Head-Tilt, Chin-Lift: This simple maneuver is often the first step in clearing the airway, especially when the obstruction is due to the patient’s tongue.
- Jaw-Thrust Maneuver: Used for patients with suspected spinal injuries, this technique helps open the airway without moving the neck.
- Oropharyngeal and Nasopharyngeal Airways: These devices help keep the airway open and are typically used for unconscious patients.
- Endotracheal Intubation: A more advanced method involving the insertion of a tube into the trachea to secure the airway in critically ill patients.
- Supraglottic Airways: Devices like the King LT or Laryngeal Mask Airway (LMA) can be used when intubation is not possible or practical.
Mastering these techniques requires not only a strong understanding of anatomy and physiology but also the ability to perform under pressure. Consistent practice and scenario-based training are essential for responders to gain confidence and proficiency in airway management, ensuring that they are ready to act quickly and effectively in real emergencies.
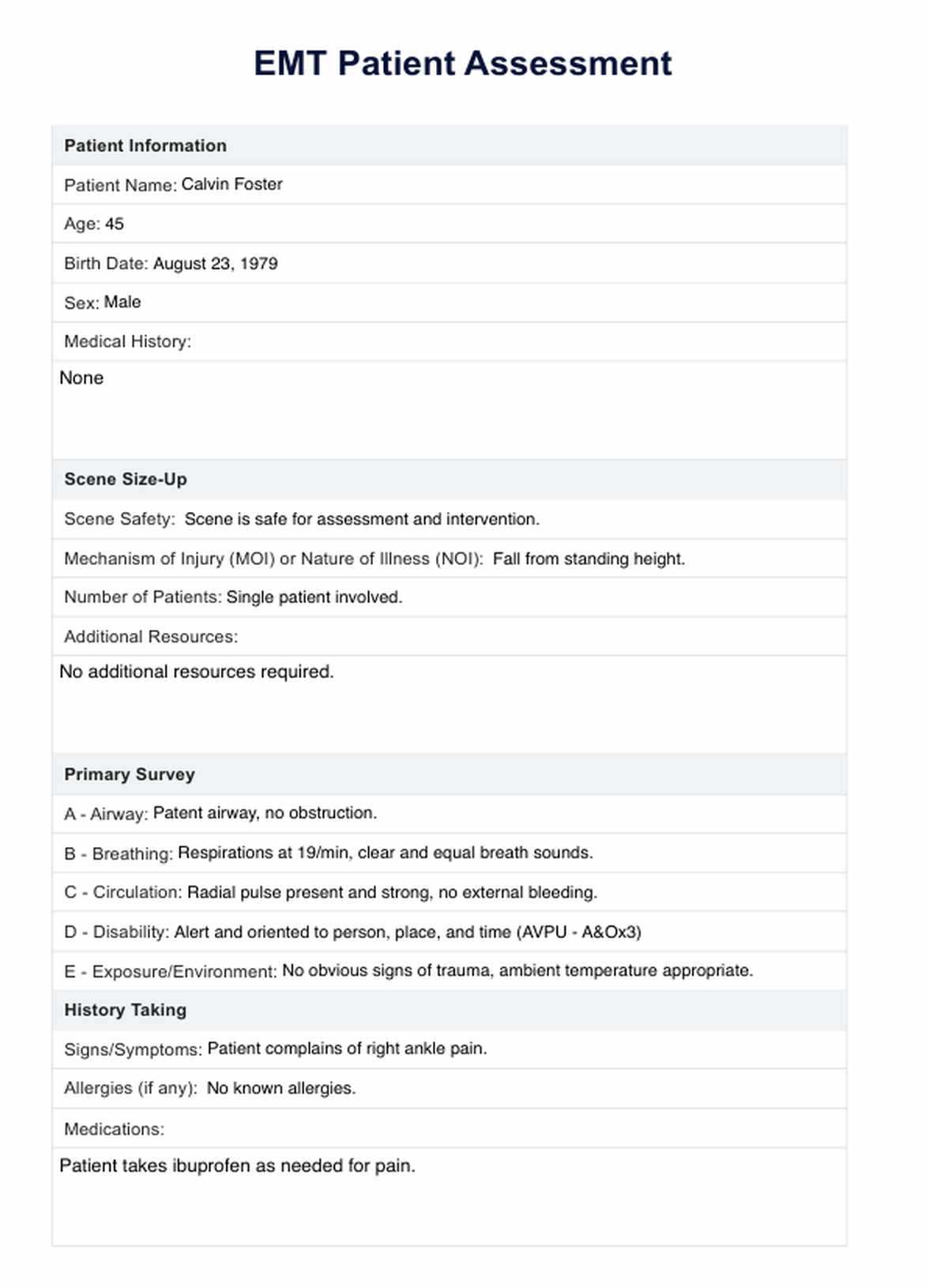
Assessment Techniques for EMT Candidates
In emergency medical situations, conducting thorough and accurate assessments is essential for determining the appropriate course of action. Evaluating a patient’s condition quickly and efficiently allows responders to prioritize care and make informed decisions. Candidates are tested on their ability to perform these evaluations under pressure, ensuring that they can assess a variety of symptoms and conditions to provide the best care possible.
Effective assessment involves a systematic approach that includes gathering vital information, observing key signs and symptoms, and making quick decisions based on the findings. It requires attention to detail, critical thinking, and strong communication skills to ensure that no vital aspect of the patient’s condition is overlooked.
Key Components of Patient Assessment
During any assessment, certain components must be prioritized to ensure all potential issues are identified. The following areas are key to providing a comprehensive evaluation:
- Primary Survey: Quickly evaluating the patient’s airway, breathing, circulation, disability, and exposure (ABCDE approach) to identify immediate life threats.
- Secondary Survey: Conducting a more detailed examination of the patient, focusing on specific injuries, medical history, and current complaints.
- Vital Signs Monitoring: Regularly checking heart rate, blood pressure, oxygen levels, and temperature to monitor changes in the patient’s condition.
- History Taking: Asking the patient (or bystanders) for a history of the present illness or injury, including past medical conditions, medications, and allergies.
- Physical Examination: Performing a head-to-toe assessment to identify any hidden injuries or abnormalities that could require urgent attention.
Common Assessment Tools and Techniques
Several tools and techniques can aid responders in performing thorough assessments and ensuring accurate results:
- Pulse Oximeter: A non-invasive tool to measure the patient’s blood oxygen saturation levels.
- Glasgow Coma Scale: A standardized scale used to assess the patient’s level of consciousness and neurological function.
- Blood Pressure Monitoring: Essential for detecting shock, internal bleeding, or other cardiovascular issues that require immediate attention.
- ECG Monitoring: Used to assess heart function and detect arrhythmias or other cardiac abnormalities.
By mastering these assessment techniques, candidates can develop the skills necessary to handle a wide range of medical emergencies. Successful evaluators must balance thoroughness with speed, ensuring that they can act decisively without missing critical details in fast-paced, high-pressure situations.
Teamwork in EMT Practical Testing
In high-pressure situations, effective collaboration is crucial to providing optimal care. When dealing with emergencies, the ability to work well with others, delegate tasks, and communicate clearly can significantly influence patient outcomes. During practical assessments, candidates are often tested not only on their individual skills but also on how they work as part of a team. Successful teamwork requires coordination, adaptability, and mutual trust, all of which contribute to a seamless response in critical moments.
Responders must be able to quickly assess the situation, prioritize actions, and assign responsibilities to team members based on their strengths and expertise. It’s important to remember that no single individual can manage all aspects of patient care alone, and the collective effort of the entire team often determines the success of an intervention. Whether it’s coordinating with medical personnel or efficiently utilizing available resources, teamwork is integral to emergency medical services.
Essential Elements of Teamwork in Emergency Situations
For optimal coordination in emergencies, the following aspects of teamwork should be emphasized:
- Clear Communication: Effective verbal and non-verbal communication ensures that each team member knows their role and responsibilities in the response process.
- Delegation of Tasks: Assigning tasks based on each person’s skills and experience ensures that critical actions, such as airway management or wound care, are handled efficiently.
- Situational Awareness: Each team member must stay aware of the overall situation, constantly reassessing the patient’s condition and adjusting actions as necessary.
- Support and Trust: Team members should support one another, recognizing each other’s strengths, offering assistance when needed, and trusting each other’s judgment in stressful situations.
Team Roles and Responsibilities
In emergency care, each team member has specific roles that contribute to the overall effectiveness of the response. The following table outlines common roles and their associated responsibilities:
| Role | Responsibilities |
|---|---|
| Team Leader | Coordinates the response, makes key decisions, and ensures tasks are being performed according to priorities. |
| Airway Management Specialist | Focuses on maintaining or securing the patient’s airway using various techniques and tools. |
| Medical Assistant | Assists with vital signs monitoring, administering medications, and preparing equipment for transport. |
| Driver | Responsible for safely transporting the patient to the hospital, navigating through traffic while maintaining patient stability. |
In practical evaluations, teamwork can be the defining factor in the success of an intervention. Being prepared to collaborate with others, maintain a clear role, and adjust as the situation evolves is critical in any emergency medical response. Practicing these elements during training prepares candidates to work effectively under the stress of real-life situations.
Responding to Pediatric Emergency Situations
Handling emergencies involving children requires a distinct approach due to their unique physiological and psychological needs. In these situations, caregivers and responders must adjust their techniques to accommodate the differences in size, vulnerability, and communication abilities of pediatric patients. Effective care for children during emergencies often involves a combination of technical skills and compassionate, age-appropriate communication to reduce fear and anxiety.
When responding to pediatric emergencies, it is crucial to approach the child gently, establish trust quickly, and ensure that both the child and their caregivers feel supported. In some cases, the emotional state of parents or guardians can impact the care provided, so it’s important to maintain a calm, reassuring demeanor while delivering medical treatment.
Key Considerations in Pediatric Emergency Care
In pediatric emergencies, several factors should be prioritized to ensure proper care:
- Size and Anatomy: Children have smaller airways, less body mass, and differing metabolic rates, requiring modified approaches for airway management, medication dosages, and physical assessment.
- Communication Techniques: Children may be frightened or unable to understand the situation fully, so it’s essential to explain procedures in a way that is appropriate for their developmental stage and to use soothing, non-threatening language.
- Parental Involvement: In many cases, involving parents or guardians in the process can help calm the child and provide critical information about the child’s medical history, allergies, and behavior.
- Age-Specific Protocols: Different age groups, from infants to adolescents, require tailored care. For example, CPR and defibrillation guidelines differ based on the child’s age and size.
Effective Approaches to Pediatric Assessment
When assessing a pediatric patient, it is important to be systematic while also being mindful of the child’s emotional state. The following steps help ensure a comprehensive evaluation:
- Initial Survey: Focus on airway, breathing, and circulation, while being aware of signs of distress, such as crying, poor color, or irregular breathing patterns.
- Detailed History: Obtain information from parents or caregivers about the child’s medical history, vaccinations, allergies, and any prior conditions that may affect treatment.
- Physical Examination: Perform a gentle head-to-toe check, being cautious around sensitive areas such as the neck, abdomen, and extremities, and using toys or distractions if needed to make the child feel more comfortable.
By mastering pediatric emergency protocols, responders can provide efficient and compassionate care while ensuring that both the child and their family are supported throughout the process. Being well-prepared for these unique challenges can greatly improve outcomes in pediatric emergencies.
Exam Tips for Critical Care Situations
When assessing skills in high-pressure environments, candidates must demonstrate their ability to manage life-threatening conditions efficiently and effectively. The key to success in these tests lies in maintaining focus, prioritizing actions, and applying theoretical knowledge in real-time, high-stakes situations. Responding to critical care scenarios requires a calm demeanor, quick decision-making, and the ability to adapt to rapidly changing conditions.
To excel in these assessments, it’s essential to develop a systematic approach. Prioritize the most immediate threats to the patient’s life, such as airway, breathing, and circulation. Understand how to perform critical interventions under time constraints while being mindful of proper techniques and safety protocols. The ability to think clearly under pressure, without rushing, is crucial for success.
Key Tips for Managing Critical Situations
To ensure that you handle these assessments with confidence, consider the following tips:
- Stay Calm: Panicking in a critical care situation can lead to poor decision-making. Keep your composure, think logically, and trust your training.
- Prioritize Life-Threatening Conditions: Begin with the basics–airway, breathing, and circulation. Assess these first before moving on to less critical aspects of care.
- Communicate Clearly: Effective communication with teammates and patients is essential. Be concise, direct, and ensure that everyone involved knows their role and responsibilities.
- Adhere to Protocols: Make sure you are familiar with the latest guidelines and follow protocols precisely, especially when it comes to medication administration and advanced interventions.
Effective Time Management
In critical care situations, time is often of the essence. While it’s important to remain calm, you also need to be efficient in your actions. Prioritize tasks in the order of importance and be mindful of time constraints when performing interventions. When you have multiple tasks to complete, delegate effectively and trust your team members to handle their responsibilities. This will help ensure that every aspect of care is addressed in a timely manner.
By focusing on these strategies, you will improve your performance in critical care situations and ensure that you are well-prepared to handle any challenges that arise during the assessment.
Managing Patient Communication During Assessments
Effective communication with patients is a critical skill that must be demonstrated during high-stress assessments. Being able to establish rapport quickly, provide clear instructions, and offer reassurance are essential for success. During these evaluations, the ability to communicate effectively not only impacts the patient’s well-being but also influences the outcome of the scenario. Responders must balance technical skills with empathetic communication to create a supportive environment, even in stressful situations.
Clear and concise communication helps ensure that the patient understands what is happening, reduces anxiety, and enables the healthcare provider to gain the necessary information for proper treatment. It’s important to speak calmly and confidently, using language that is easy for the patient to understand, while maintaining a professional and compassionate demeanor.
Building Trust with the Patient
Establishing trust with the patient is a crucial first step. This can be achieved by:
- Introducing Yourself: Clearly introduce yourself and your role in the situation. This helps create transparency and reduces uncertainty for the patient.
- Active Listening: Pay attention to the patient’s concerns, show empathy, and validate their feelings. Listening is a key part of building rapport and ensuring effective care.
- Maintaining a Calm Presence: Speak in a calm, soothing tone, even if the situation is chaotic. A calm demeanor can help reduce the patient’s anxiety and allow for better cooperation.
Providing Clear Instructions
Once trust is established, it is important to give clear instructions to the patient. These instructions should be simple, direct, and appropriate for the patient’s level of understanding. Avoid medical jargon and use language the patient can relate to. Key points to remember include:
- Simple Instructions: When providing directions, keep them short and simple. Instead of overwhelming the patient with multiple steps, break the information down into manageable pieces.
- Reassurance: Reassure the patient that they are receiving the best care possible. This can help alleviate stress and foster a sense of security.
- Maintain Eye Contact: Making eye contact during communication can help convey sincerity and help the patient feel heard and understood.
By maintaining effective communication throughout an assessment, responders not only improve patient outcomes but also enhance the overall experience for both the patient and the healthcare provider. Mastering these communication skills is key to demonstrating competence in high-stress environments.
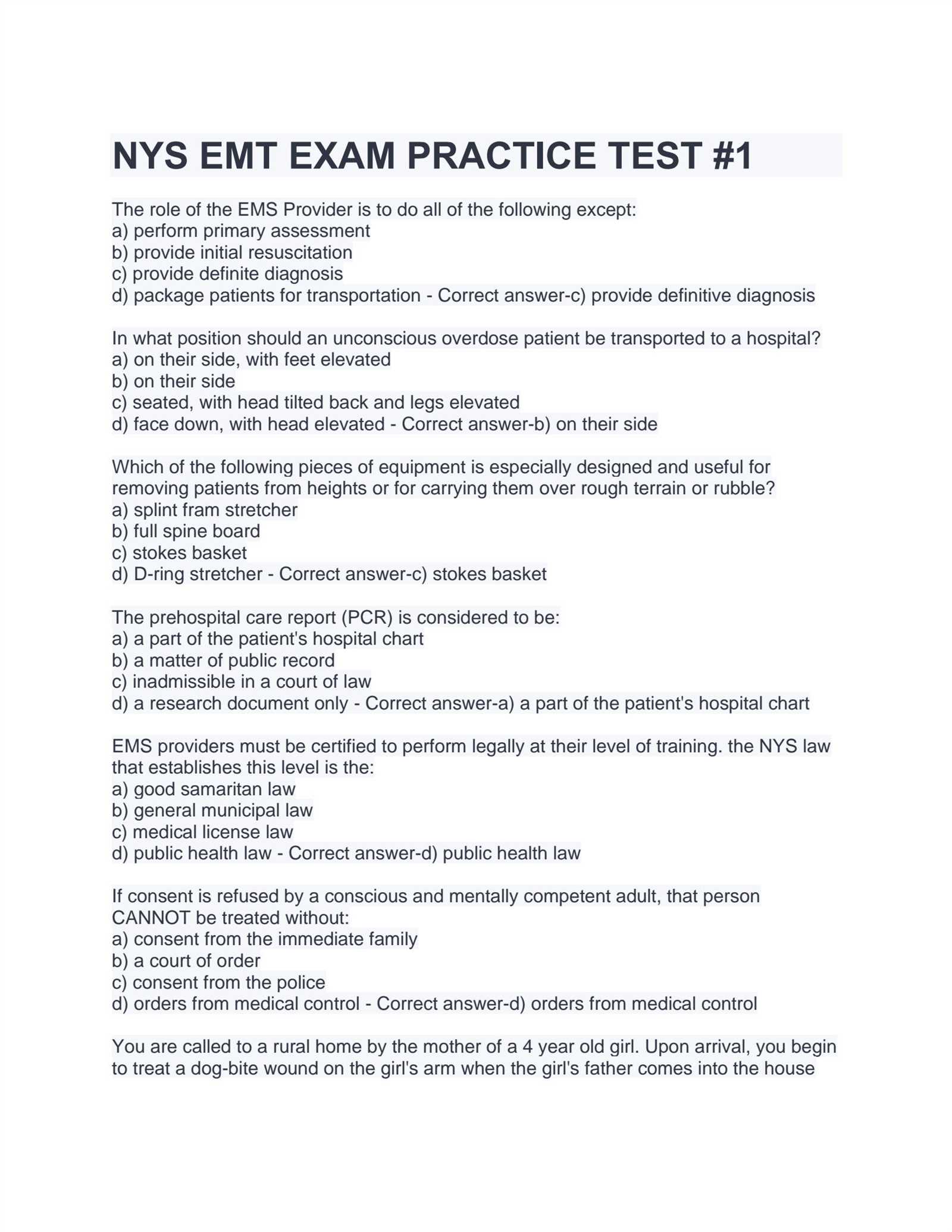
Legal and Ethical Considerations in Testing
When participating in assessments, especially those that simulate real-world emergencies, it is crucial to understand the legal and ethical responsibilities that come with the role. These evaluations not only test technical knowledge and skills but also assess the candidate’s ability to act within the bounds of the law and uphold professional ethical standards. Responders must be prepared to navigate complex situations that may involve patient rights, consent, and confidentiality, all while ensuring that they are performing within their legal scope of practice.
Ethical considerations in these assessments often focus on respect for patient dignity, ensuring that care is provided impartially, and maintaining professionalism in stressful environments. Legal issues might include understanding consent laws, reporting requirements, and maintaining proper documentation. Knowledge of these principles is essential to avoid potential legal pitfalls and to protect both the patient and the healthcare provider from harm.
Key Legal Considerations
In any assessment, candidates must be aware of the following legal responsibilities:
- Informed Consent: Always ensure that the patient or their legal representative understands and agrees to the interventions being performed. This is a cornerstone of ethical medical practice.
- Confidentiality: Respect patient confidentiality at all times. Any personal health information should only be shared with those directly involved in the patient’s care or as legally required.
- Scope of Practice: Be aware of your legal scope of practice and do not perform tasks that exceed your certification level or training. Overstepping these boundaries can have serious legal implications.
Ethical Responsibilities in Testing
Ethical conduct in assessments is just as important as technical proficiency. Some key ethical considerations include:
- Respect for Patient Autonomy: Always respect the patient’s right to make decisions regarding their care, provided they are capable of doing so.
- Non-Maleficence: Ensure that no harm is done during the assessment process. This means avoiding unnecessary risks and taking steps to prevent further injury or distress to the patient.
- Honesty and Integrity: Be truthful about your skills, experience, and limitations. If uncertain about any aspect of the situation, it is important to communicate this and seek assistance when needed.
By understanding and adhering to both legal and ethical guidelines, candidates can demonstrate their professionalism and commitment to patient safety, ensuring a positive outcome in both the assessment and real-life situations.
Dealing with Stress During Practical Exams
Stress is a natural response to high-pressure situations, especially when performing tasks that have real-life implications. During assessments, the pressure to perform at your best can be overwhelming. However, managing stress effectively is essential not only for your performance but also for your well-being. Learning to stay calm and focused under pressure is a skill that can be developed with the right strategies and mindset.
While stress is unavoidable in high-stakes evaluations, how you handle it can make all the difference. This section will explore techniques to help manage anxiety and stay focused during testing, ensuring that you can perform at your best even when the situation feels intense.
Effective Stress Management Techniques
There are several strategies that can help reduce stress and maintain composure during an assessment:
- Preparation is Key: One of the best ways to reduce anxiety is through thorough preparation. The more familiar you are with the procedures and techniques being assessed, the more confident and relaxed you will feel when it’s time to demonstrate your skills.
- Breathing Exercises: Deep breathing can help calm your mind and body. Taking slow, controlled breaths before and during the assessment can help reduce stress and refocus your attention.
- Positive Visualization: Visualizing yourself successfully completing the tasks can build confidence and reduce feelings of doubt. Picture yourself handling the situation calmly and effectively.
- Stay Present: Avoid getting caught up in negative thoughts or worrying about the outcome. Focus on the task at hand and take things one step at a time.
Building Confidence Through Experience
Confidence plays a significant role in stress management. The more you practice, the more confident you become in your abilities, which in turn helps reduce anxiety. Engaging in mock assessments or simulated practice sessions can provide valuable experience and help you familiarize yourself with the testing environment.
Remember, stress is a natural part of any evaluation process, but with the right mindset and techniques, you can manage it effectively and perform at your best. The key is preparation, focus, and the ability to remain calm when it counts the most.
Using Equipment Efficiently in Simulations
In any high-pressure situation, being able to use equipment efficiently is crucial for ensuring both the safety of the patient and the success of the operation. During simulated scenarios, familiarity with medical tools and devices plays a vital role in how well candidates perform. Understanding each piece of equipment’s function, handling it with precision, and knowing when and how to use it can make all the difference when working under time constraints.
In this section, we’ll explore best practices for utilizing equipment effectively during testing simulations. Mastering these techniques can help candidates save valuable time and avoid unnecessary mistakes during assessments.
Key Equipment Handling Tips
- Familiarity with Tools: Before entering a simulation, candidates should take time to familiarize themselves with all the equipment they may need. Understanding the functions of various tools–such as airway devices, defibrillators, and monitoring equipment–ensures quick and efficient use when needed.
- Organization and Setup: Keeping tools organized and easily accessible is essential. During a simulation, time is often of the essence, so ensuring everything is properly set up and within arm’s reach can reduce stress and improve efficiency.
- Prioritize Actions: In many situations, there are multiple tasks that must be performed. Prioritizing which equipment to use first can help streamline the process and prevent delays. For instance, securing the airway might be more urgent than taking vitals in certain emergencies.
- Practice Simulations: Regular practice with medical equipment in controlled environments helps candidates become more comfortable and confident. This practice can improve speed and accuracy, especially in high-stress scenarios.
Common Equipment Mistakes to Avoid
While practice is essential, it’s equally important to be aware of common mistakes that can occur when using medical tools during simulations. Avoiding these errors ensures a more effective and professional performance.
| Error | Consequence | How to Avoid |
|---|---|---|
| Improperly Setting Up Equipment | Delays in treatment, confusion during critical moments | Always double-check setup before starting a scenario |
| Failure to Test Equipment | Non-functional equipment when needed | Perform a quick functionality check before using any device |
| Overuse of Tools | Wasted time, unnecessary actions | Use only the tools necessary for the situation at hand |
In any high-stakes situation, being able to handle equipment efficiently and effectively can have a significant impact on both the outcome of the scenario and your performance. Practice, preparation, and a calm, organized approach are essential to using tools to their full potential.
What to Expect on Your Test Day
On the day of your assessment, it’s important to be well-prepared and mentally focused. Knowing what to expect can help alleviate any anxiety and ensure you’re ready to perform at your best. The day is typically structured to assess your clinical skills, decision-making, and ability to handle real-life situations under pressure. Understanding the flow of the day will help you approach each task confidently and effectively.
From the moment you arrive at the testing site, there will be a series of steps to follow, from registration to completing various tasks. Here’s a breakdown of what you can expect:
Before the Testing Begins
- Arrive Early: It’s crucial to arrive early to allow time for check-in, setup, and any necessary paperwork. This also gives you the opportunity to acclimate to the environment and clear your mind before starting.
- Provide Documentation: Be prepared to present any required documents, such as identification, certification of training, or proof of eligibility for the assessment.
- Equipment Check: You may be required to inspect and familiarize yourself with the equipment that will be used during the day. This is your chance to ensure everything is functioning properly.
During the Assessment
- Station-Based Testing: The assessment is often broken down into multiple stations, each focused on different aspects of patient care. At each station, you will be required to perform specific tasks or demonstrate certain skills in a controlled environment.
- Time Constraints: Each task or station typically comes with a time limit. It’s important to manage your time effectively and prioritize actions to complete the scenario successfully.
- Evaluation: Evaluators will observe your performance at each station, assessing your competence in various areas such as decision-making, communication, and technical skills. Their feedback will be used to determine your overall performance.
- Stay Calm and Focused: While the pressure may be high, maintaining composure and focusing on each task as it comes will help you perform better. Take deep breaths, think clearly, and follow your training.
After the Testing
- Feedback: Once the assessment is complete, you may receive immediate feedback on your performance. In some cases, there may be a debriefing session to discuss your strengths and areas for improvement.
- Results: Results may be provided at the end of the day or within a few days, depending on the testing process. If you pass, you’ll be one step closer to certification. If not, you’ll likely be given feedback on areas to focus on for a retake.
Test day can be stressful, but with proper preparation, a clear mindset, and a calm approach, you’ll be equipped to handle the challenges and showcase your skills effectively.
Post-Assessment Reflection and Improvement
After completing your assessment, it is essential to take time for reflection in order to learn from the experience and identify areas for improvement. This process allows you to understand what went well, what could have been done better, and how to prepare more effectively for future challenges. Reflecting on your performance will not only help you grow but also build confidence in your abilities as a healthcare provider.
Key Areas to Reflect On
- Task Execution: Consider how efficiently you performed each task. Did you follow the correct steps? Were there any moments where you hesitated or made errors? Identifying these moments can help you pinpoint areas that need more practice.
- Time Management: Think about how well you managed your time during the assessment. Were you able to complete all the required steps within the time limit? If not, try to evaluate where you lost time and plan how to improve for the future.
- Communication Skills: Reflect on your ability to communicate with patients, colleagues, and evaluators. Effective communication is crucial in emergency situations, so evaluate how clearly and confidently you conveyed information.
- Decision-Making: Assess your decision-making under pressure. Did you make sound judgments based on the situation? Were there any moments where you might have taken a different approach? Understanding your decision-making process can help you make quicker and more accurate choices in the future.
Steps to Improve
- Practice Regularly: The more you practice, the more comfortable and efficient you will become. Set aside time to practice key skills, whether it’s through mock assessments, hands-on drills, or working with colleagues in a clinical environment.
- Review Feedback: Pay close attention to any feedback you received during or after the assessment. Constructive criticism can provide valuable insights into areas where you need to focus your efforts for improvement.
- Self-Assessment: Regularly assess your own performance. This could involve reviewing case studies, evaluating your technique, or using simulation tools to practice your skills in various scenarios.
- Stay Calm Under Pressure: Stress can impair performance, so finding ways to remain calm and focused in high-pressure situations is crucial. Practice relaxation techniques, such as deep breathing or visualization, to help manage stress effectively.
- Seek Mentorship: If possible, find a mentor who can provide guidance and share their experiences. A mentor can offer advice, share tips for improvement, and help you navigate challenges more effectively.
By reflecting on your performance and actively working to improve, you can increase your confidence and skills for future assessments and real-world situations. Consistent effort and a focus on learning will allow you to grow as a healthcare professional and provide the best care possible in every situation.