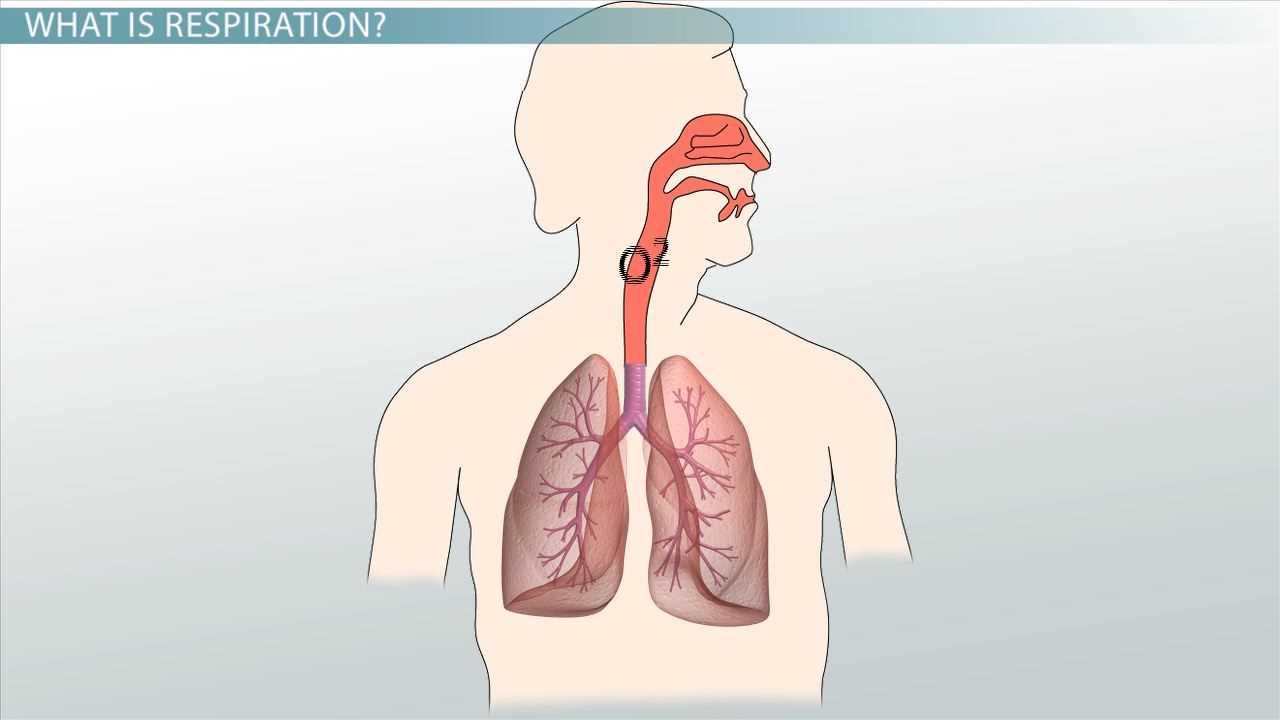
The process of breathing is vital for sustaining life, allowing the body to take in oxygen and expel carbon dioxide. This continuous cycle supports cellular functions and maintains overall health. In this section, we explore how the body facilitates this exchange, focusing on the mechanics and key components involved in the process.
Key structures such as the lungs, airways, and blood vessels work together to ensure that oxygen is delivered to tissues and waste gases are removed. The intricate process relies on several factors, including the movement of air, gas diffusion, and the role of specific cells. Understanding these functions is essential for grasping how the body maintains homeostasis and adapts to different conditions.
Health conditions can affect the efficiency of these functions, leading to various challenges. By examining these processes in detail, we can better understand common disorders and preventive measures for maintaining optimal health.
Understanding the Breathing Mechanisms
The process of taking in air and exchanging gases is crucial for maintaining life. This complex sequence involves several key structures that work together to ensure efficient oxygen transport throughout the body and the removal of waste products like carbon dioxide. By exploring these functions, we can better understand the roles each part plays in sustaining health.
Here are the fundamental steps that contribute to the process:
- Inhalation of air through the nose or mouth.
- Air passes through the trachea, branching into the lungs.
- Oxygen from the air diffuses into the bloodstream via the alveoli.
- Waste gases, such as carbon dioxide, diffuse from the blood into the alveoli.
- Exhalation expels the carbon dioxide-rich air from the lungs.
Each step is essential for ensuring that tissues receive sufficient oxygen for cellular functions. Disruptions in any part of this process can lead to complications and health issues. It’s important to understand how each component of this cycle contributes to overall well-being.
The lungs and associated structures play the central role in this vital exchange, while the circulatory system supports the transport of gases to and from the cells. Various diseases can impair these processes, making it crucial to study their mechanics in-depth.
To further grasp the significance of these processes, let’s look at some of the key components involved:
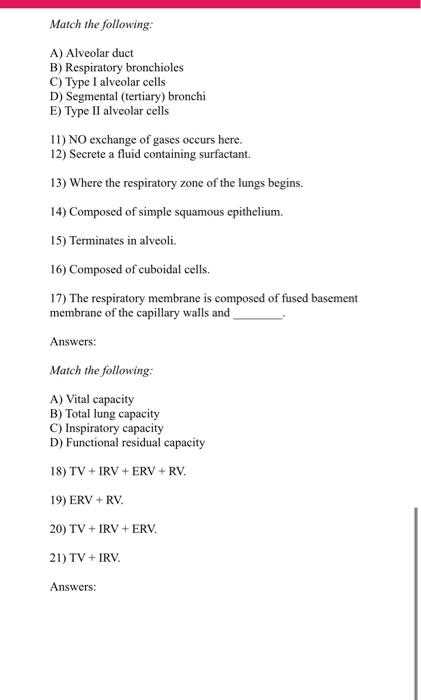
- Alveoli: Tiny air sacs where oxygen and carbon dioxide are exchanged.
- Capillaries: Small blood vessels that transport gases between the lungs and bloodstream.
- Diaphragm: The primary muscle involved in the expansion and contraction of the lungs.
- Trachea and Bronchi: Airways that direct air to the lungs.
Through this understanding, we can develop a clearer picture of how disruptions in these processes affect overall health and the steps needed for effective treatment and prevention.
Understanding the Breathing Process Basics
The act of breathing is a vital function that supports life by facilitating the intake of oxygen and the removal of carbon dioxide. This ongoing process enables cells throughout the body to perform necessary functions and maintain homeostasis. The process is not limited to the lungs alone but involves a network of structures working in harmony to ensure the delivery of oxygen to the bloodstream and the expulsion of waste gases.
The body relies on a series of interconnected parts to carry out this essential task. These include airways that channel air into the lungs, as well as tissues and organs that regulate gas exchange. The process is not passive; it is controlled by muscle contractions and the pressure differences between the lungs and the outside environment.
Through the efficient coordination of these components, the body is able to meet its metabolic needs, supporting the function of organs and tissues across different states of activity, from rest to intense exertion.
Key Components of the Human Lungs
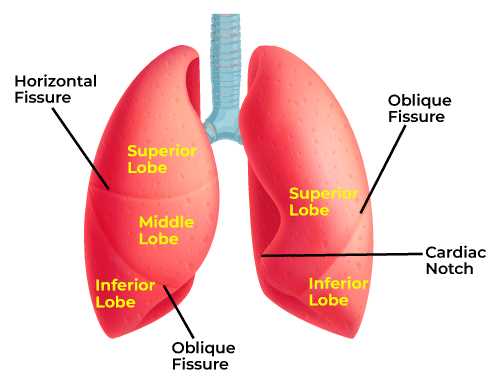
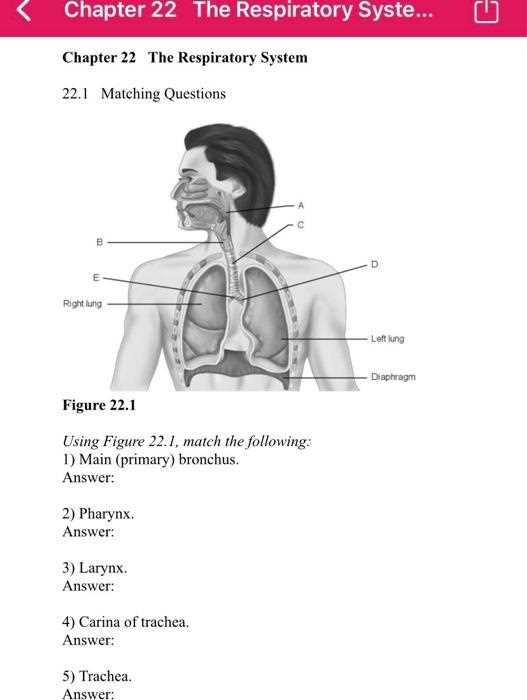
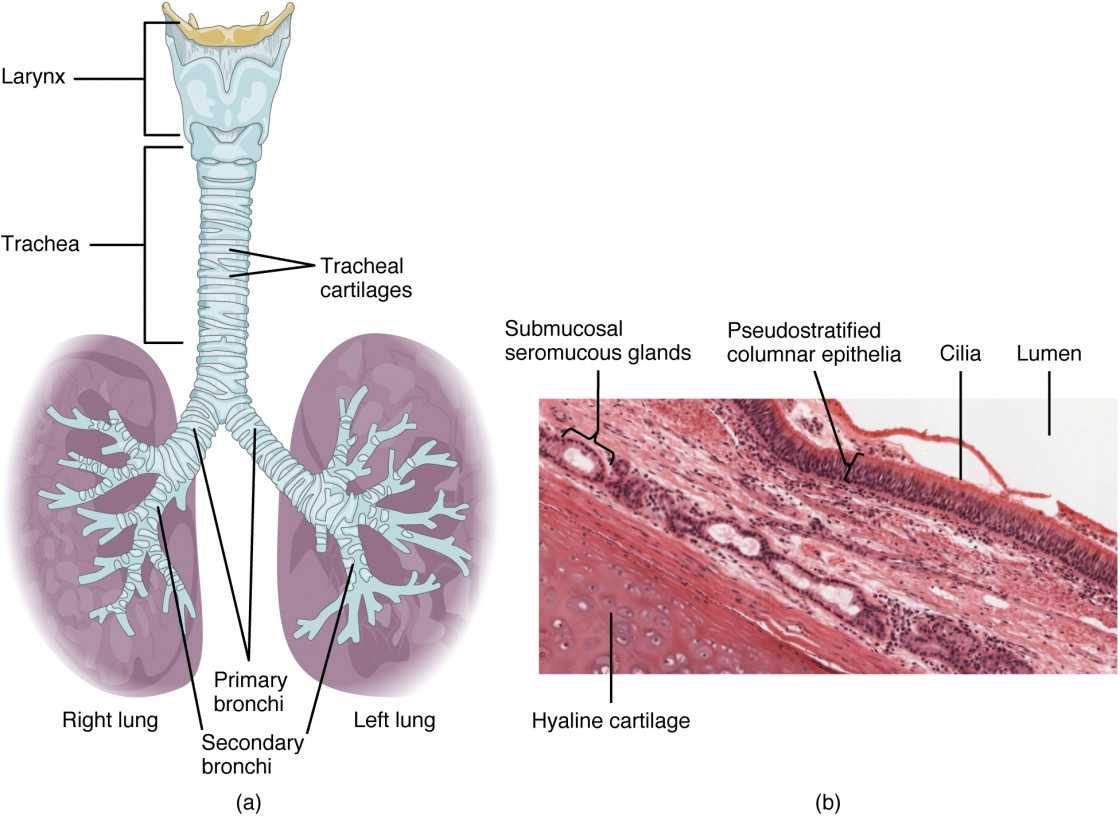
The lungs are vital organs responsible for exchanging gases between the air and bloodstream. They consist of several specialized structures, each playing a unique role in ensuring that oxygen is absorbed and carbon dioxide is expelled. Understanding these key components helps clarify how the body supports cellular function and maintains balance.
Lung Structure
The primary structure of the lungs consists of lobes, with the right lung having three lobes and the left lung having two. Inside the lungs, air passes through a network of branching tubes called bronchi, which split into smaller bronchioles. These tubes lead to tiny air sacs known as alveoli, where the actual gas exchange takes place. The alveoli have a large surface area and are surrounded by capillaries, allowing for efficient oxygen transfer into the blood and carbon dioxide removal.
Supporting Structures
In addition to the alveoli, other important components of the lungs include the diaphragm, a muscle that controls lung expansion and contraction during breathing. The pleura, a double-layered membrane, surrounds the lungs and helps protect them while facilitating smooth movement within the chest cavity. The bronchi and bronchioles are lined with mucous membranes and cilia that help trap and clear out foreign particles, preventing infections and maintaining airway cleanliness.
How Breathing Works in the Body
Breathing is a vital process that enables the body to take in oxygen and expel carbon dioxide. This cycle is essential for sustaining life and providing the necessary gas exchange for cellular functions. The mechanics of this process involve coordinated actions of muscles, airways, and organs, working together to maintain balance within the body.
When air is inhaled, it travels through the nose or mouth and moves down the trachea into the lungs. As it passes through the airways, oxygen is absorbed into the bloodstream through tiny sacs called alveoli. At the same time, carbon dioxide, a waste product of cellular processes, is transported from the blood into the lungs to be exhaled.
The diaphragm plays a central role in this process. It contracts and flattens during inhalation, expanding the chest cavity and allowing the lungs to fill with air. During exhalation, the diaphragm relaxes and the chest cavity decreases in size, forcing air out of the lungs. This cycle of expansion and contraction ensures that fresh air is continuously drawn in and waste gases are expelled from the body.
The body’s ability to regulate the rate and depth of breathing is controlled by the brain in response to factors such as oxygen levels, carbon dioxide concentration, and physical activity. This constant adjustment ensures that the body’s cells receive a steady supply of oxygen while maintaining homeostasis.
Functions of the Breathing Passageways
The breathing passageways serve multiple essential functions that are crucial for the proper exchange of gases within the body. These structures ensure that air is delivered efficiently to the lungs while filtering, warming, and moistening the air before it reaches the delicate tissues involved in gas exchange. Their role is to support optimal oxygen intake and waste removal, all while maintaining the body’s overall balance.
The airways act as a conduit for inhaled air, guiding it through the nose, throat, and windpipe into the lungs. Along the way, the passages filter out dust, pathogens, and other foreign particles through the action of mucus and tiny hair-like structures called cilia. This cleaning mechanism helps prevent infections and irritations in the lungs.
Additionally, the passageways help regulate the temperature and humidity of the incoming air, ensuring that the lungs receive air that is comfortable for the delicate alveolar structures. By maintaining the right conditions, these pathways support the overall function of the lungs, allowing for efficient gas exchange and protecting them from harmful environmental factors.
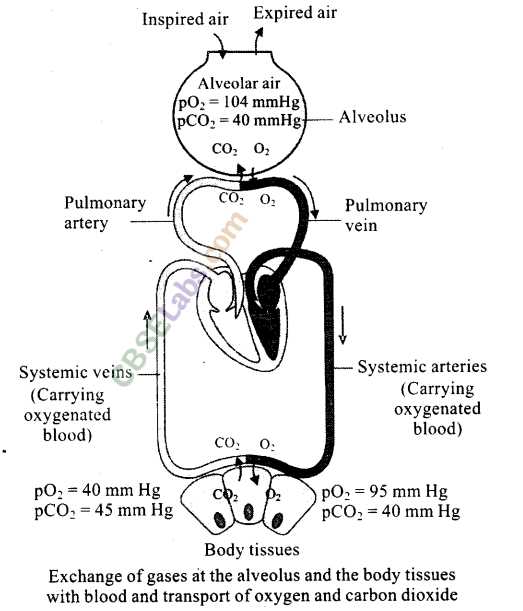
Exploring Gas Exchange Mechanisms
Gas exchange is a fundamental process that occurs in the lungs, allowing oxygen to enter the bloodstream while removing carbon dioxide. This exchange takes place in tiny air sacs where oxygen from the inhaled air diffuses into the blood, and waste gases like carbon dioxide move in the opposite direction to be exhaled. The efficiency of this process is essential for providing cells with the oxygen they need for energy production and removing metabolic waste.
The process relies on several factors, including the concentration gradients of gases, the surface area of the exchange tissues, and the permeability of the membrane. Oxygen moves from an area of higher concentration in the alveoli to a lower concentration in the blood, while carbon dioxide follows the opposite direction. This passive diffusion mechanism ensures that the body maintains a stable internal environment.
| Gas | Direction of Movement | Purpose |
|---|---|---|
| Oxygen | Inhaled air to bloodstream | Provide oxygen to cells for energy production |
| Carbon Dioxide | Bloodstream to exhaled air | Remove waste product of cellular metabolism |
The efficiency of this exchange is influenced by factors such as lung health, the surface area of the alveoli, and the overall circulation of blood. Any disruption in this process can lead to reduced oxygen supply to the tissues and an accumulation of waste gases, which can result in respiratory complications.
The Role of Alveoli in Respiration
The alveoli are the small, specialized air sacs in the lungs where the crucial process of gas exchange takes place. These structures provide a large surface area that facilitates the transfer of oxygen into the blood and the removal of carbon dioxide from the bloodstream. Their unique design ensures efficient diffusion, supporting the body’s need for oxygen while expelling metabolic waste.
Structure and Function
Each alveolus is surrounded by a network of tiny blood vessels known as capillaries, creating a close relationship between air and blood. The walls of the alveoli are extremely thin, which allows gases to pass through easily. Oxygen from the inhaled air diffuses through the alveolar wall and into the blood, while carbon dioxide moves in the opposite direction to be exhaled.
Efficiency of Gas Exchange
The large number of alveoli in the lungs ensures a vast surface area, increasing the efficiency of gas exchange. This vast area, combined with the thinness of the alveolar walls and the high concentration gradients of oxygen and carbon dioxide, enables rapid diffusion of gases. Any damage to these air sacs can significantly reduce the body’s ability to absorb oxygen, leading to respiratory complications.
How Oxygen Reaches the Bloodstream
The journey of oxygen from the air into the bloodstream is a critical process that enables cells throughout the body to function. Once air is inhaled into the lungs, oxygen moves through the various passageways and reaches the alveoli, tiny sacs where the exchange of gases takes place. Here, oxygen diffuses from the air into the blood, while carbon dioxide, a waste product, moves from the blood to be exhaled.
This process relies on the differences in concentration between the oxygen in the alveoli and the blood in the surrounding capillaries. The oxygen in the air sacs is at a higher concentration than in the blood, prompting it to move into the bloodstream by diffusion. At the same time, carbon dioxide, which is more concentrated in the blood, diffuses out of the capillaries into the alveoli to be expelled from the body during exhalation.
The oxygen that enters the blood binds to red blood cells, specifically to hemoglobin, which carries it through the circulatory system to the tissues and organs. This efficient transport ensures that oxygen is delivered to where it is needed for energy production, allowing the body to carry out its essential functions.
The Mechanics of Inhalation and Exhalation
The process of breathing involves two main actions: taking in air (inhalation) and expelling air (exhalation). These movements are controlled by the muscles in the chest and diaphragm, which work in coordination to change the pressure in the lungs. Understanding the mechanics of these actions helps clarify how the body ensures a continuous supply of oxygen and removes carbon dioxide effectively.
Inhalation Process
During inhalation, the diaphragm contracts and moves downward, while the intercostal muscles between the ribs contract to expand the chest cavity. This expansion reduces the pressure inside the lungs, causing air to flow in from the outside to equalize the pressure. As the lungs fill with air, oxygen is delivered to the alveoli, where it can be transferred into the bloodstream.
Exhalation Process
Exhalation is a more passive process. As the diaphragm and intercostal muscles relax, the chest cavity decreases in size, increasing the pressure inside the lungs. This higher pressure pushes air out of the lungs and through the airways to be expelled. Carbon dioxide, a waste product from cellular activity, is carried out during this exhalation cycle.
| Action | Muscle Activity | Resulting Movement |
|---|---|---|
| Inhalation | Diaphragm contracts, intercostal muscles expand | Lungs expand, air flows in |
| Exhalation | Diaphragm relaxes, intercostal muscles relax | Lungs contract, air is expelled |
The coordinated action of these muscles allows for efficient air exchange, ensuring that the body receives oxygen and eliminates carbon dioxide with every breath.
Common Disorders of the Breathing Pathways
Various conditions can affect the body’s ability to take in oxygen and expel carbon dioxide. These issues can arise from infections, environmental factors, or chronic diseases that impact the efficiency of gas exchange. Understanding the most common disorders helps in recognizing symptoms early and seeking appropriate care.
- Asthma: A condition where the airways become inflamed and constricted, making it difficult to breathe. Triggers include allergens, smoke, or exercise.
- Chronic Obstructive Pulmonary Disease (COPD): A group of lung diseases, including emphysema and chronic bronchitis, that cause long-term breathing problems and difficulty expelling air.
- Pneumonia: An infection of the lungs that causes inflammation and fluid buildup, leading to symptoms like cough, fever, and difficulty breathing.
- Bronchitis: Inflammation of the bronchi, often caused by infection or irritants like smoke, leading to coughing and shortness of breath.
- Lung Cancer: Malignant growth in the lungs that can disrupt normal respiratory functions. It is often linked to smoking but can also occur in non-smokers.
These conditions, whether acute or chronic, can significantly affect breathing and overall health. Early diagnosis and treatment are crucial for managing symptoms and improving quality of life.
Impact of Smoking on Lung Health
Smoking has a profound effect on the body’s ability to function properly, particularly when it comes to breathing. The harmful chemicals found in tobacco smoke can damage the delicate tissues of the lungs and airways, leading to a range of chronic conditions that impair normal lung function. Over time, these harmful effects accumulate, increasing the risk of severe health problems.
Short-Term Effects: Immediately after smoking, the airways become inflamed, and mucus production increases, leading to temporary symptoms such as coughing and shortness of breath. These effects can also make it more difficult for the lungs to clear out particles and toxins.
Long-Term Effects: Prolonged exposure to smoke can lead to serious damage, including chronic obstructive pulmonary disease (COPD), emphysema, and chronic bronchitis. The toxins in cigarette smoke damage the air sacs, causing the lungs to lose elasticity and reducing the efficiency of gas exchange. As a result, the body struggles to get enough oxygen and expel carbon dioxide.
Smoking also increases the risk of lung cancer, as the carcinogens in tobacco smoke can alter the DNA in lung cells, leading to uncontrolled cell growth and tumor formation. The combination of these long-term effects can drastically reduce lung function, making it harder for individuals to breathe and leading to a diminished quality of life.
Quitting smoking can significantly improve lung health, although some damage may be irreversible. Early intervention and cessation can help reduce further harm and promote recovery in the long run.
Respiratory System and Acid-Base Balance
The body maintains a delicate balance between acids and bases in the blood to ensure proper functioning of cells and organs. One of the key roles of the breathing pathways is regulating this balance by controlling the levels of carbon dioxide (CO2) in the blood. Changes in CO2 levels can directly influence the pH of the blood, making the regulation of breathing essential for maintaining homeostasis.
- Carbon Dioxide and pH Levels: As cells produce energy, they release CO2 as a byproduct. If CO2 accumulates, it forms carbonic acid in the blood, which lowers the pH and makes the blood more acidic. On the other hand, breathing out CO2 helps reduce acidity, raising the pH back to normal levels.
- Buffer Systems: The body also has buffering systems, like the bicarbonate buffer system, which help to neutralize excess acids or bases in the blood. These systems work in conjunction with the breathing pathways to prevent drastic changes in pH that could harm cells and organs.
- Hyperventilation and Hypoventilation: Breathing patterns can impact acid-base balance. Rapid, shallow breathing (hyperventilation) expels too much CO2, leading to alkalosis, where the blood becomes too basic. Conversely, slow breathing (hypoventilation) can cause an accumulation of CO2, leading to acidosis, where the blood becomes too acidic.
In this way, the body’s ability to adjust breathing rate and depth helps regulate acid-base balance, ensuring that internal conditions remain stable and conducive to life.
The Effect of Exercise on Breathing
Physical activity places increased demands on the body, requiring more oxygen to fuel muscles and other tissues. As a result, the body adjusts its breathing patterns to meet these demands. During exercise, the rate and depth of breathing increase to supply oxygen more efficiently and remove carbon dioxide, which is produced in greater quantities during activity.
Initially, the body compensates by increasing the rate of breathing, which allows for a higher intake of oxygen and quicker expulsion of carbon dioxide. As exercise continues, the muscles and lungs work together more effectively to maintain optimal oxygen levels in the blood. This process ensures that the body can continue performing strenuous tasks without experiencing fatigue or oxygen deprivation.
Over time, regular physical activity can improve the efficiency of the breathing pathways. This results in a lower resting breathing rate and improved lung capacity, allowing individuals to perform physical tasks with less effort and a quicker recovery time. The body becomes more adept at managing oxygen use, leading to better overall fitness and endurance.
Factors Influencing Breathing Rate
The rate at which a person breathes is not constant and can change based on various internal and external factors. The body adjusts its breathing rate to meet the changing demands for oxygen and to remove excess carbon dioxide. This dynamic process is influenced by several key factors, ranging from physical activity to emotional states.
Physical Activity and Oxygen Demand
One of the most significant factors influencing breathing rate is the level of physical activity. During exercise, muscles consume more oxygen and produce more carbon dioxide, prompting the body to increase its breathing rate. This ensures that enough oxygen is delivered to the tissues and that carbon dioxide is efficiently removed.
Emotions and Stress Responses
Emotional states, such as anxiety or stress, can also lead to changes in the rate and pattern of breathing. In stressful situations, the body enters a fight-or-flight response, which can cause rapid, shallow breathing. This helps prepare the body for action but can also lead to hyperventilation if prolonged.
Other factors that can influence breathing rate include:
- Altitude: At higher elevations, the air contains less oxygen, so the body compensates by increasing the rate of breathing to bring in more oxygen.
- Temperature: Extreme temperatures, either hot or cold, can affect the rate of breathing. Cold air may cause constriction of airways, making breathing slightly more difficult, while hot air can increase the need for cooling through faster breathing.
- Health Conditions: Certain illnesses, like lung infections or asthma, can impact how efficiently the lungs function, leading to changes in the breathing rate as the body tries to maintain oxygen levels.
Understanding these factors helps explain why breathing patterns can vary in different situations and how the body adapts to meet its needs.
Diseases Affecting Lung Capacity
Lung capacity refers to the amount of air the lungs can hold, and it plays a crucial role in maintaining efficient oxygen exchange in the body. Several diseases can reduce lung capacity, making it difficult for individuals to breathe properly. These conditions may affect the structure or function of the lungs, leading to shortness of breath, reduced exercise tolerance, and in severe cases, respiratory failure.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease is a progressive condition that causes inflammation and narrowing of the airways, making it harder for air to flow in and out of the lungs. This results in a decreased lung volume and difficulty breathing. The two most common forms of COPD are emphysema and chronic bronchitis. Over time, the lungs lose their ability to expand fully, leading to a significant reduction in lung capacity.
Fibrosis and Scarring of Lung Tissue
Lung fibrosis is a condition in which the lung tissue becomes scarred and stiff, limiting its ability to stretch and expand. This leads to a decrease in total lung capacity. The scarring process can be triggered by various factors, including long-term exposure to pollutants, certain medications, and autoimmune diseases. As the lungs become less flexible, the body’s ability to take in sufficient oxygen is compromised.
Other conditions that can impact lung capacity include:
- Asthma: Asthma causes temporary narrowing of the airways, which may reduce lung function, especially during an attack.
- Pulmonary Hypertension: High blood pressure in the lungs’ arteries can make it harder for the heart and lungs to function properly, reducing lung capacity.
- Obesity: Excess weight can restrict the expansion of the lungs, leading to a decrease in overall lung capacity and increased difficulty breathing, especially during physical activity.
Managing these conditions often requires medication, lifestyle changes, and in some cases, breathing exercises to help improve lung function and capacity. Early diagnosis and treatment are key to preventing further damage and improving quality of life for those affected.
Respiratory System and Immune Response
The body’s defense mechanisms are closely linked with the process of breathing. The primary role of the lungs is not only to provide oxygen but also to act as a barrier against harmful pathogens that can enter through the air. This connection between the lung functions and immune protection is crucial for maintaining overall health. As we inhale, we also take in bacteria, viruses, and other foreign particles, and the body has built-in defense strategies to prevent these from causing harm.
Defensive Mechanisms in the Airways
The airways have several layers of defense that help filter out unwanted particles and microbes. These include:
- Mucus Production: The mucus lining of the airways traps dust, pathogens, and other foreign particles, preventing them from reaching deeper into the lungs.
- Cilia: Tiny hair-like structures called cilia move in a coordinated manner to push trapped particles upward toward the throat, where they can be swallowed or expelled through coughing.
- Antibacterial Enzymes: Enzymes present in the mucus can neutralize harmful bacteria and viruses before they cause infection.
Immune Cells in the Lungs
The lungs are also home to various immune cells that actively monitor for threats. These include:
- Macrophages: These cells are the first line of defense and help engulf and destroy harmful microbes that enter the lungs.
- Dendritic Cells: These cells identify invaders and trigger an immune response by signaling other parts of the immune system.
- Neutrophils: In cases of infection, neutrophils are recruited to the lungs to fight off pathogens and prevent them from spreading.
While the body’s natural defense mechanisms work to protect the lungs from infection and harm, certain conditions, such as allergies or chronic illnesses, can weaken these defenses, making the lungs more vulnerable to disease. This highlights the importance of maintaining lung health through good habits such as avoiding smoking, staying active, and avoiding exposure to harmful pollutants.