
Preparing for the Pediatric Advanced Life Support (PALS) certification involves a comprehensive review of key topics related to emergency pediatric care. The exam tests your ability to manage critical situations involving children, from cardiovascular issues to airway management. This guide offers insights into how to approach the preparation process and succeed in the exam.
Successful preparation requires a deep understanding of core concepts such as pediatric resuscitation, medication dosages, and recognition of life-threatening conditions. Knowing how to navigate these topics efficiently will not only help you perform well in the exam but also enhance your readiness for real-world clinical scenarios. Mastering these areas is crucial for healthcare providers involved in pediatric emergencies.
Staying focused on high-priority topics, practicing key skills, and reviewing common clinical cases will give you a solid foundation for the test. Additionally, being familiar with the structure and common pitfalls of the exam will allow you to tackle it with greater confidence and accuracy. This preparation is an important step toward becoming a certified professional in pediatric emergency care.
Pediatric Advanced Life Support Exam Preparation Insights
Before taking the exam for advanced pediatric life support, it is essential to familiarize yourself with the type of questions and topics that will be covered. This process helps ensure that you are well-prepared to tackle critical scenarios involving pediatric patients in emergency settings. It requires a solid understanding of key concepts such as airway management, CPR techniques, and recognizing pediatric arrhythmias.
Understanding the most frequently tested areas and practicing with sample scenarios can greatly improve your chances of success. The questions typically focus on diagnosing and managing life-threatening conditions in children, providing an opportunity to demonstrate both theoretical knowledge and practical skills. Reviewing the most common conditions and treatment strategies will help you navigate through the exam effectively.
By analyzing the test format and focusing on the critical aspects of pediatric emergency care, you will be able to confidently approach the exam. Being prepared for questions related to specific case studies and clinical situations will not only help you answer correctly but also reinforce the skills necessary for real-world application.
Understanding the PALS Assessment
The exam for pediatric emergency care is designed to evaluate your ability to manage critical situations involving children. It tests knowledge and practical skills required in high-pressure environments, focusing on accurate diagnosis and effective treatment strategies. The goal is to ensure that healthcare providers are well-prepared to respond to life-threatening conditions in pediatric patients.
The test typically covers a range of topics that are essential for anyone working in pediatric emergency care. These topics include:
- Cardiovascular emergencies, such as arrhythmias and shock management
- Airway management and ventilation techniques for children
- Drug dosages and proper administration in pediatric cases
- Recognizing and treating common pediatric emergencies
- CPR protocols and procedures specific to young patients
Familiarity with these topics is crucial for success, as the exam evaluates your theoretical understanding as well as your ability to apply this knowledge in practical scenarios. The questions are designed to simulate real-world situations, providing a true test of your readiness to handle pediatric emergencies with confidence and skill.
Key Changes in the 2025 Precourse
The upcoming exam for pediatric emergency care has undergone several updates to better reflect the latest practices and protocols in the field. These changes are intended to enhance the accuracy of testing, ensuring that healthcare providers are prepared for the most current and complex situations they might encounter. Staying informed about these updates is crucial for achieving success in the certification process.
Here are some of the key changes introduced in the latest version:
| Area | Previous Focus | New Focus |
|---|---|---|
| Cardiovascular Emergencies | Basic arrhythmia recognition and treatment | Advanced protocols for pediatric arrhythmias and shock management |
| Airway Management | Standard ventilation techniques | Enhanced focus on high-risk cases and non-invasive approaches |
| Medication Dosages | General dosage guidelines | More emphasis on weight-based calculations and updated drug protocols |
| CPR Techniques | Traditional CPR practices | New guidelines for CPR in cases of trauma and respiratory failure |
These adjustments reflect the evolving nature of pediatric emergency care and the growing complexity of medical scenarios. Healthcare professionals must familiarize themselves with these updates to stay ahead of the curve and ensure they are following the most current standards of care. Understanding these changes will not only help in passing the exam but will also improve real-world practice and decision-making in critical situations.
How to Approach the PALS Self Assessment
Preparing for the pediatric emergency care exam requires more than just memorizing facts; it demands a structured approach to ensure you are well-equipped to answer a range of challenging questions. By understanding the exam format and focusing on key areas of pediatric care, you can increase your chances of success. This section offers guidance on how to effectively prepare and navigate through the evaluation process.
Here are some strategies for a successful approach:
- Review Core Topics Thoroughly: Focus on critical areas such as airway management, pediatric shock, and arrhythmias. Make sure to understand the guidelines for different emergencies.
- Practice with Sample Scenarios: Familiarize yourself with case-based questions to improve your ability to think quickly and apply knowledge in real-life situations.
- Understand the Exam Format: Knowing the structure of the questions, whether multiple choice or clinical vignettes, will help you manage your time effectively during the test.
- Use Trusted Study Materials: Ensure you are using up-to-date resources that align with current guidelines and protocols in pediatric emergency care.
- Simulate Test Conditions: Practice under timed conditions to improve your speed and accuracy when answering questions.
Approaching the exam with these strategies will not only enhance your performance but also build your confidence in applying life-saving techniques to pediatric patients. By investing time in targeted study and practice, you will be better prepared for the challenges you may encounter during the certification process.
Common Mistakes to Avoid in 2025
During preparation for the pediatric emergency care exam, many candidates make a few common errors that can hinder their success. Recognizing and avoiding these mistakes will help you navigate the exam more efficiently and confidently. By focusing on the right areas and approaching the test with the correct mindset, you can avoid pitfalls that others often fall into.
Relying Too Much on Memorization
One of the most frequent mistakes is relying solely on memorization without fully understanding the underlying principles. While it’s important to remember specific protocols and drug dosages, it’s equally critical to grasp the reasoning behind these guidelines. Focus on how to apply knowledge in practical scenarios rather than just recalling facts.
Neglecting the Practical Application
Another mistake is not practicing enough real-world scenarios. The exam is designed to assess how well you can manage pediatric emergencies, so practicing case studies and simulation-based questions is essential. Hands-on practice with scenarios will improve your ability to think on your feet and make quick, informed decisions under pressure.
Inadequate Time Management is also a common issue. Many candidates spend too much time on certain questions and then run out of time before finishing the test. It’s important to pace yourself and move through questions at a steady rate to ensure you complete all sections within the allotted time.
By avoiding these mistakes, you will significantly improve your performance and be better prepared to handle the challenges of the exam. Keep a balanced approach to your study, focusing on both theoretical knowledge and practical application, and manage your time wisely throughout the process.
Tips for Effective Exam Preparation
Preparing for the pediatric emergency care exam requires a well-organized study plan, consistent practice, and a strategic approach. To excel in the test, it’s important to focus on both theoretical knowledge and practical skills. Adopting the right techniques will not only improve your understanding of critical topics but also boost your confidence when facing the exam.
Create a Structured Study Schedule
One of the most effective ways to prepare is to establish a clear study schedule. Break down your study materials into manageable sections and allocate specific time for each topic. Prioritize areas where you feel less confident, but don’t neglect subjects that are your strengths. Consistent, focused study sessions will keep you on track and help you retain information better.
Utilize Practical Practice and Simulations
Simply reading or memorizing material isn’t enough for a comprehensive exam like this. You need to practice applying your knowledge to real-life scenarios. Engage in simulation exercises that mimic the conditions of the exam. These could include timed quizzes, case studies, or mock exams that test your ability to make decisions under pressure. The more you practice, the more prepared you’ll be for unexpected challenges during the actual test.
Review Past Cases and Guidelines regularly to reinforce your understanding of emergency protocols. Familiarity with common clinical situations and updated treatment guidelines will ensure that you can handle any question confidently. Practicing with sample cases and reviewing key concepts will prepare you for the most challenging portions of the exam.
By following these tips and staying consistent with your preparation, you’ll be well-equipped to perform at your best and succeed in the certification process. A balanced approach of structured study and practical application is key to mastering the material and excelling in the exam.
Important Topics Covered in Pediatric Emergency Care Certification
The pediatric emergency care certification exam focuses on the most critical aspects of treating children in life-threatening situations. It is essential to understand and apply core concepts that are routinely used in emergency and critical care settings. The exam tests both theoretical knowledge and practical decision-making skills, ensuring that candidates are prepared to handle urgent medical scenarios with confidence.
Cardiovascular Emergencies
One of the key areas of focus in the exam is managing pediatric cardiovascular emergencies. This includes understanding various arrhythmias, shock management, and cardiac arrest protocols for children. Proper assessment of circulation and quick intervention with the correct medications and techniques can significantly improve patient outcomes. In-depth knowledge of pediatric CPR, defibrillation, and pharmacological treatments is critical for success in this section.
Airway Management and Breathing Support
Another crucial topic involves airway management and the different strategies used to support breathing in pediatric patients. Candidates must be familiar with various ventilation techniques, such as bag-valve-mask (BVM) and intubation, as well as the use of advanced airways. The exam evaluates the ability to assess a patient’s airway and breathing status, as well as the ability to provide life-saving interventions in a timely and effective manner.
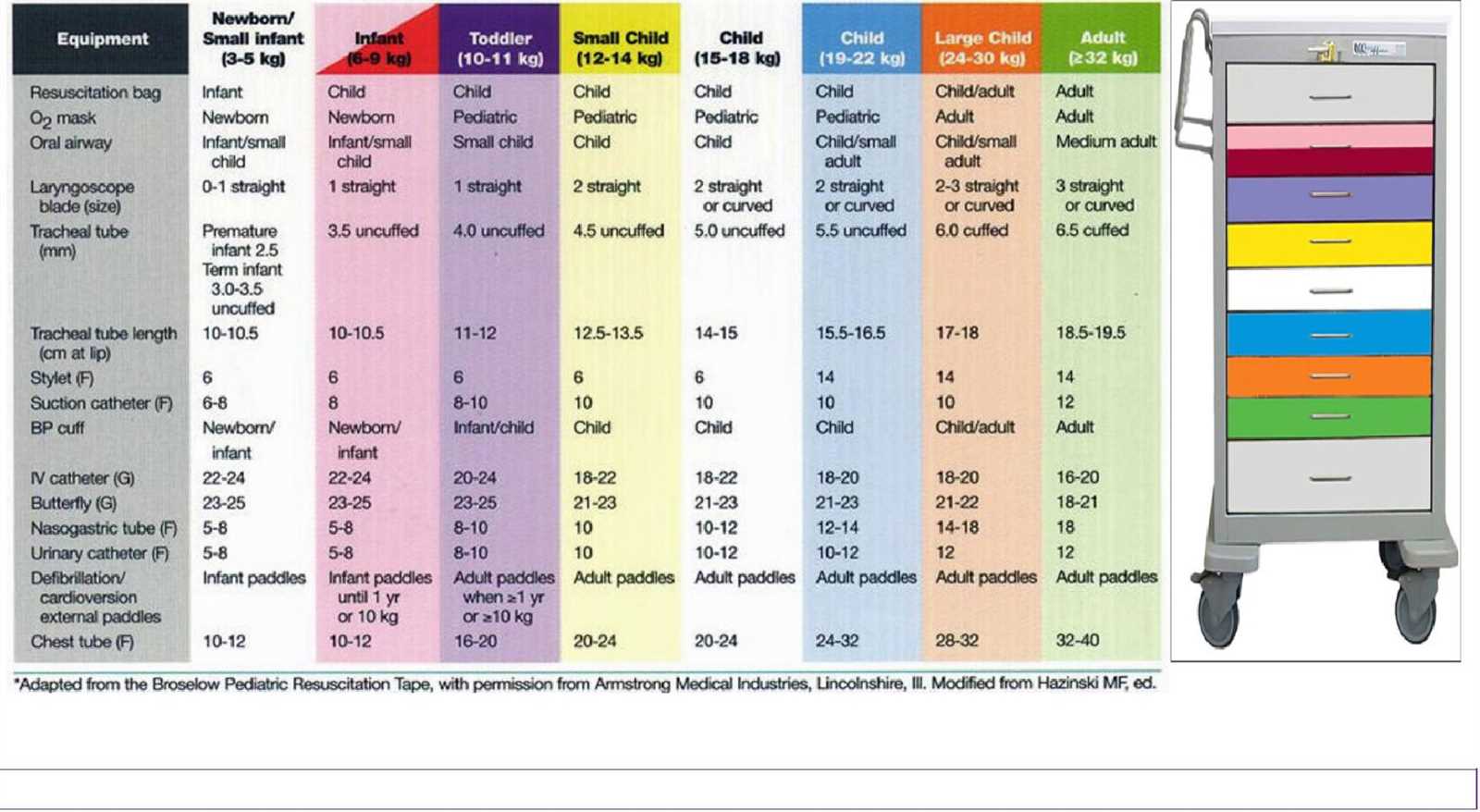
Drug Dosages and Administration are also central to the exam. Healthcare providers need to be able to calculate appropriate drug dosages based on the child’s age, weight, and condition. Understanding the pharmacology of emergency medications, such as epinephrine and atropine, and knowing when and how to administer them is critical for effective patient care.
Familiarity with these core topics will not only ensure success on the exam but also enhance your ability to provide optimal care during pediatric emergencies. Understanding these areas in depth is essential for any healthcare professional involved in pediatric critical care or emergency medicine.
Reviewing Pediatric Cardiovascular Emergencies
Cardiovascular emergencies in children are among the most critical situations healthcare professionals must manage. Early recognition and prompt intervention can significantly impact a child’s outcome. Understanding the signs, causes, and treatment protocols for various cardiovascular conditions is essential for healthcare providers involved in pediatric care, especially during emergencies. This section will focus on the key aspects of pediatric cardiovascular crises and the best practices for managing them.
The most common pediatric cardiovascular emergencies include conditions like shock, arrhythmias, and cardiac arrest. Each of these conditions requires specific knowledge about pathophysiology, clinical signs, and treatment options. Healthcare providers must be prepared to assess the severity of the situation quickly, initiate appropriate interventions, and monitor for improvements or complications.
Shock in pediatric patients can result from a variety of causes, such as dehydration, blood loss, or sepsis. Recognizing the early stages of shock is critical, as it can rapidly progress to life-threatening situations. Management involves restoring circulation and oxygen delivery, which may include administering fluids, medications, or even blood products, depending on the underlying cause.
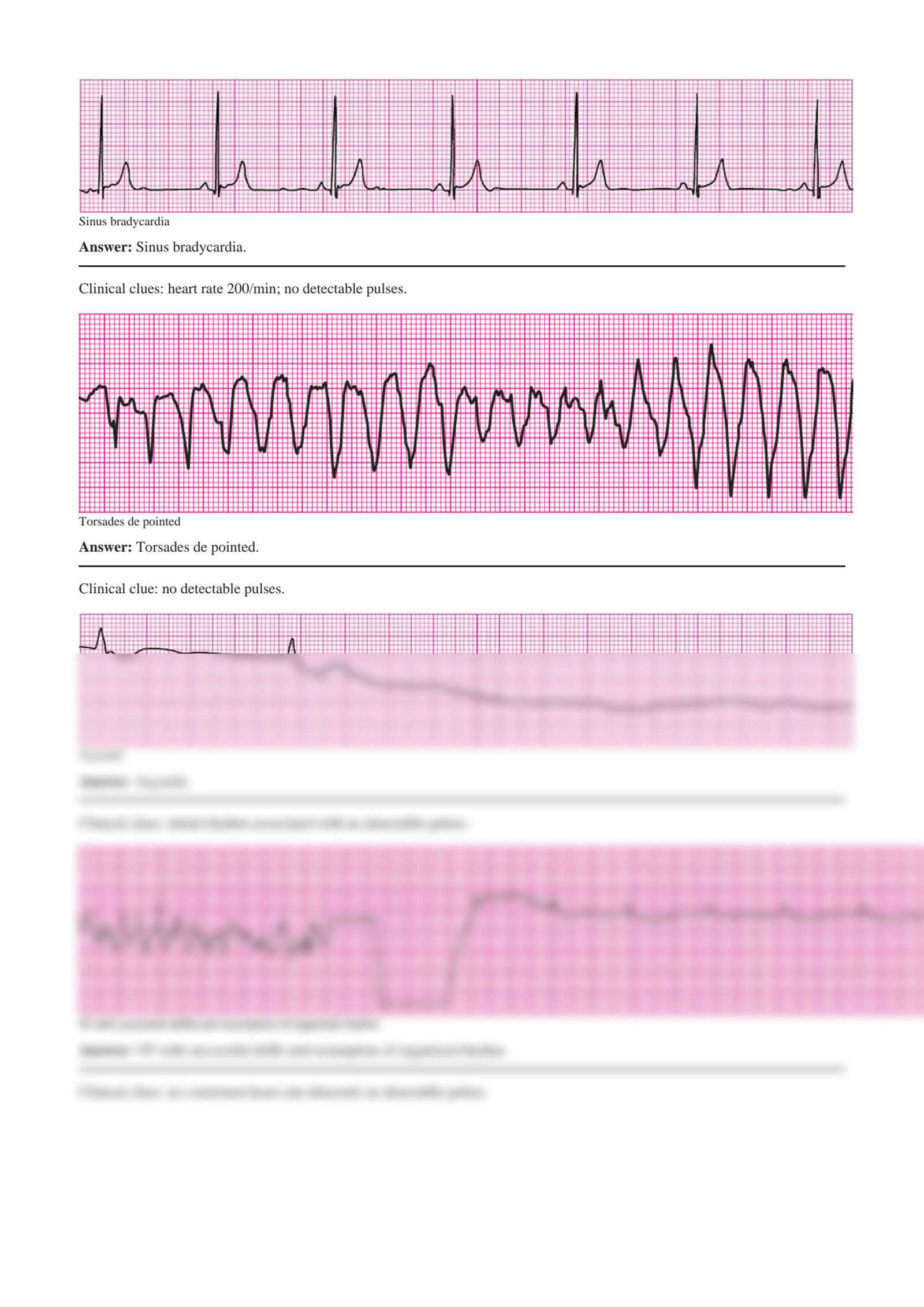
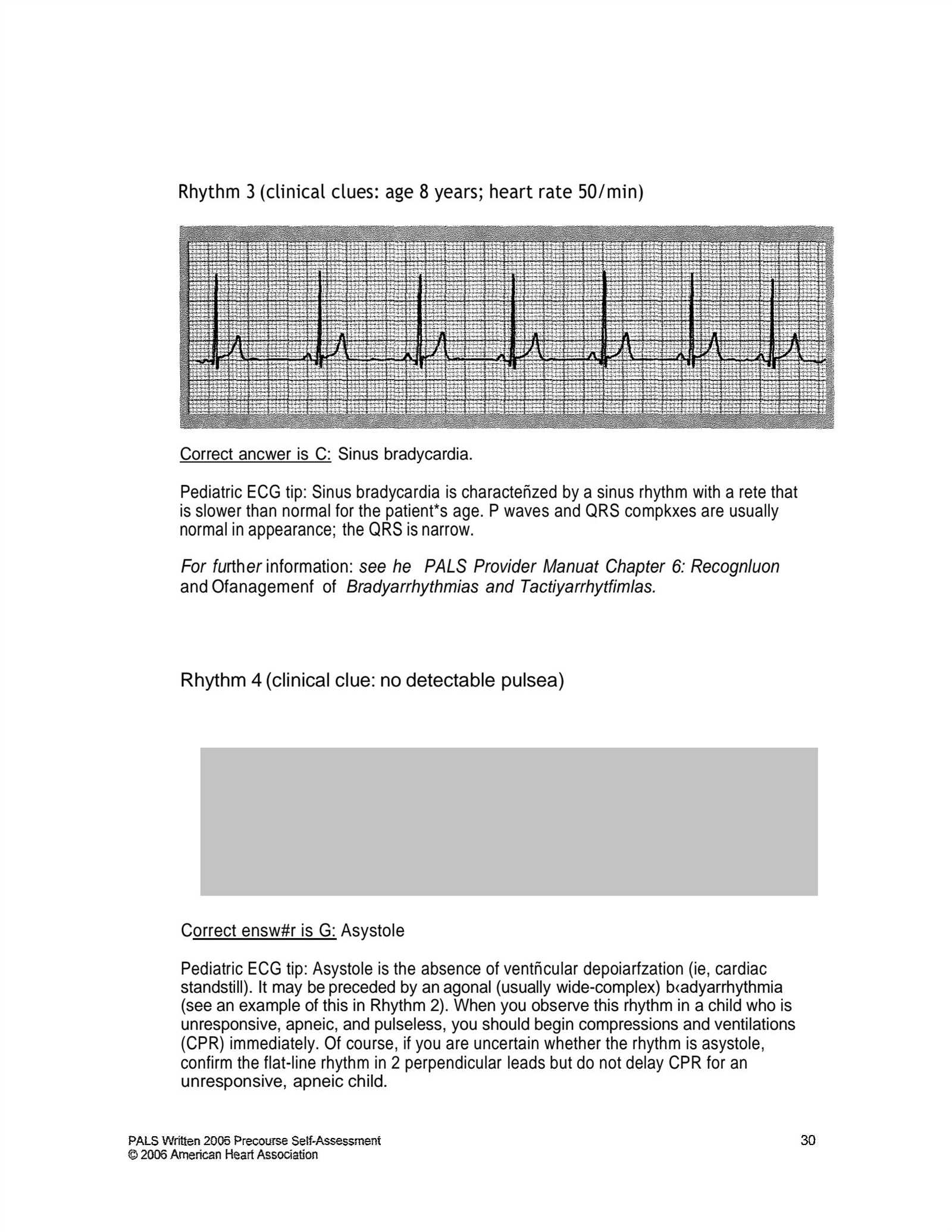
Arrhythmias are abnormal heart rhythms that can present with a wide range of symptoms, from mild discomfort to complete cardiac arrest. It is essential for clinicians to differentiate between different types of arrhythmias, including tachycardia, bradycardia, and ventricular fibrillation, to determine the most appropriate course of treatment. This may involve defibrillation, medication, or pacing to restore normal rhythm.
Finally, pediatric cardiac arrest requires immediate, high-quality CPR and advanced life support techniques. The timing of defibrillation, the use of medications such as epinephrine, and the careful management of airway and circulation are all vital in improving survival rates. Prompt intervention and adherence to updated protocols can make the difference between life and death in these high-stakes situations.
In preparation for handling these emergencies, healthcare providers should regularly review the latest guidelines and practice protocols. Familiarity with pediatric-specific interventions and the ability to make quick decisions are crucial skills for effectively managing cardiovascular emergencies in children.
Essential Airway Management Techniques
Effective airway management is a cornerstone of pediatric emergency care. In critical situations, ensuring an open and secure airway can make the difference between life and death. Healthcare providers must be proficient in various techniques to quickly assess and manage airway obstructions, maintain oxygenation, and ensure ventilation. This section focuses on the key airway management strategies that are essential for handling pediatric emergencies.
The first step in airway management is assessing the patient’s airway to identify any blockages or potential complications. This can be done by observing the patient’s breathing, checking for any visible obstructions, and listening for abnormal sounds such as stridor or wheezing. Once an assessment is made, the appropriate intervention can be chosen based on the severity of the situation.
Basic airway maneuvers, such as head-tilt/chin-lift and jaw-thrust, are the foundation of airway management. These techniques help open the airway by positioning the head in a way that relieves any potential obstructions. In cases of suspected cervical spine injury, the jaw-thrust maneuver is preferred to minimize head and neck movement.
When basic maneuvers are not sufficient, advanced airway techniques may be necessary. Endotracheal intubation involves inserting a tube into the trachea to maintain an open airway and provide ventilation. This technique requires proper training and practice to ensure correct tube placement and avoid complications such as injury or aspiration.
Another essential airway management technique is the use of supraglottic airway devices, such as laryngeal mask airways (LMA). These devices are often used when intubation is difficult or impractical. They can provide a secure airway and facilitate effective ventilation in emergency situations.
In addition to these techniques, it is important to monitor the patient’s oxygenation levels continuously. If the patient is not breathing adequately, supplemental oxygen should be administered, and mechanical ventilation may be required if the patient’s own breathing is insufficient.
Mastery of these airway management techniques is vital for handling pediatric emergencies effectively. Understanding when and how to use each technique, along with the ability to perform them efficiently, will greatly improve outcomes for pediatric patients in critical situations.
Understanding Medication Dosages for Pediatric Emergencies
Proper medication dosage is a critical component in the effective management of pediatric emergencies. Accurate dosing ensures that the right amount of medication is administered to achieve the desired therapeutic effect without causing harm. In the high-pressure environment of an emergency situation, healthcare providers must be able to quickly calculate and administer the correct dosages for children of varying ages and sizes. This section covers the essential principles of pediatric drug dosing and highlights the key considerations for healthcare professionals.
One of the most important aspects of pediatric medication dosing is adjusting for the child’s weight and age. Since children are not simply scaled-down adults, their bodies metabolize drugs differently. This requires careful calculation, often based on weight in kilograms or body surface area, to determine the correct dose. Understanding common dosing formulas, such as mg per kg, is crucial for preventing underdose or overdose, both of which can lead to serious complications.
Common Pediatric Medications often used in emergencies include epinephrine, atropine, and albuterol. These drugs play essential roles in managing cardiac arrest, bradycardia, and respiratory distress, respectively. Each medication comes with its own specific dosing guidelines based on a child’s weight or age group. For example, the recommended dose of epinephrine for cardiac arrest is usually 0.01 mg/kg, while the dose for atropine in bradycardic infants can range between 0.02 mg/kg depending on the situation.
In addition to weight-based calculations, healthcare providers must also be familiar with concentration units such as milligrams per milliliter (mg/mL), which are crucial when drawing up medications from vials or syringes. This requires attention to detail to ensure that the correct concentration is used for the specific patient needs. When in doubt, it’s always important to consult dosing charts or protocols available in the clinical setting.
Another critical concept is knowing the timing of drug administration. In many emergency situations, timing can be as important as the dose. For instance, medications like epinephrine must be administered at the correct intervals during resuscitation efforts to optimize chances of successful recovery.
Understanding these principles allows healthcare professionals to make informed decisions under pressure, improving the safety and effectiveness of treatments provided in pediatric emergencies. Mastery of medication dosing is essential for all providers involved in critical care and emergency response.
Dealing with Pediatric Arrhythmias in Emergency Care
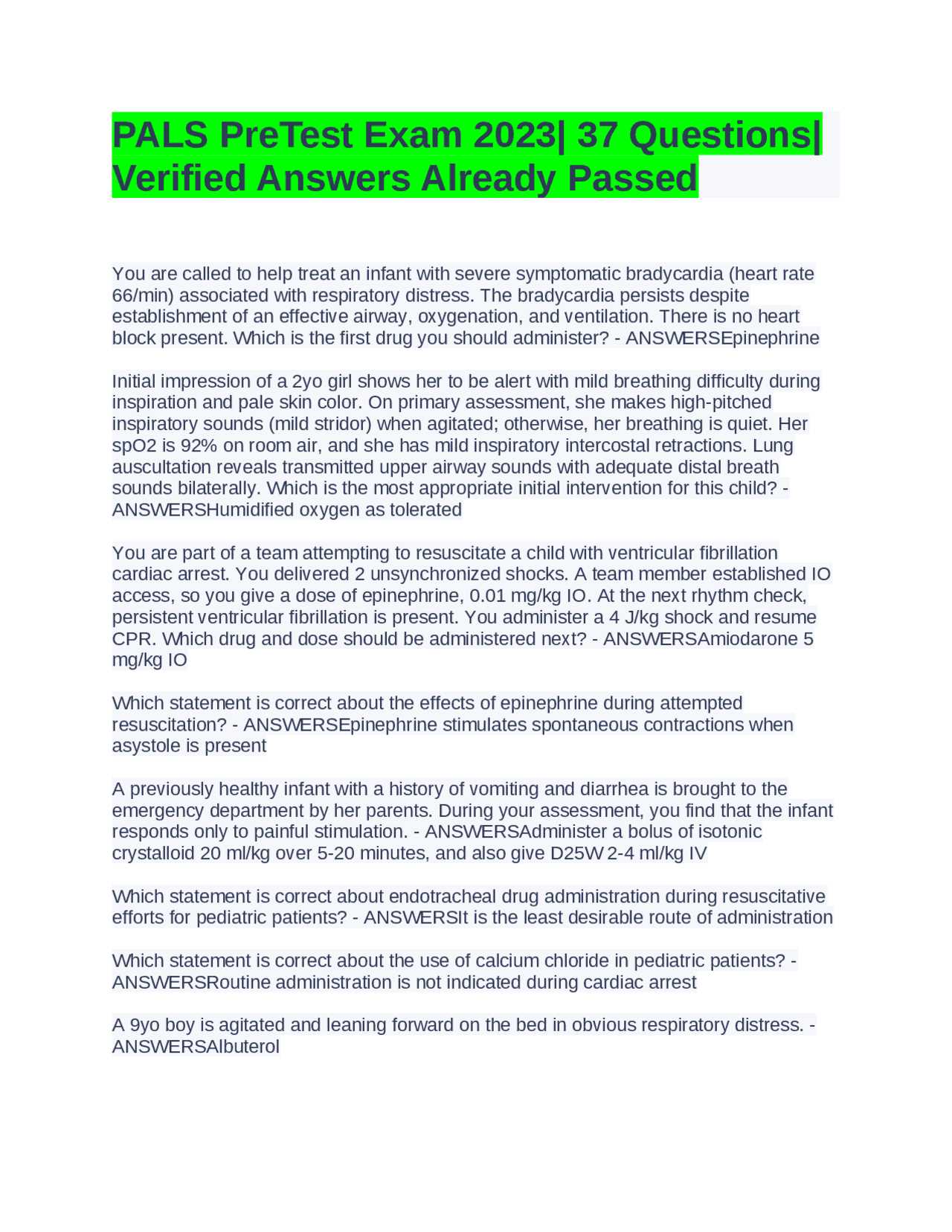
Pediatric arrhythmias are abnormal heart rhythms that can significantly impact a child’s ability to circulate blood and oxygen effectively. These conditions can range from relatively benign to life-threatening and require prompt recognition and intervention. Understanding how to manage various types of arrhythmias in children is a crucial skill for healthcare providers working in emergency settings. This section focuses on the key approaches and treatment options for handling pediatric arrhythmias in critical care environments.
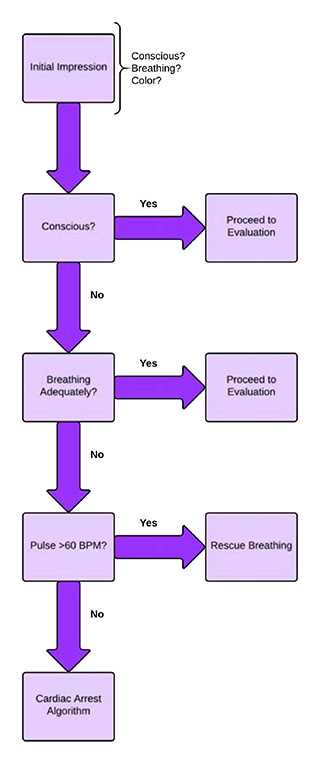
The first step in managing any arrhythmia is accurate identification. Not all arrhythmias present the same way, and symptoms can vary greatly depending on the child’s age, the type of arrhythmia, and its underlying cause. It is important for healthcare providers to recognize the clinical signs of arrhythmias, which may include tachycardia, bradycardia, irregular heartbeats, or even sudden collapse.
Types of Pediatric Arrhythmias
Common arrhythmias in pediatric patients include tachycardias, such as supraventricular tachycardia (SVT), and bradycardias, such as sinus bradycardia. Each type of arrhythmia requires specific interventions and treatments. Below is a table summarizing the management strategies for some of the most common arrhythmias in children:
| Arrhythmia Type | Symptoms | Initial Treatment | Advanced Treatment |
|---|---|---|---|
| Supraventricular Tachycardia (SVT) | Rapid heart rate, dizziness, chest pain | Vagal maneuvers, adenosine | Cardioversion (if unresponsive to initial treatment) |
| Sinus Bradycardia | Fatigue, weakness, pale skin | Observation, oxygen support | Atropine, pacing (if symptomatic) |
| Ventricular Tachycardia | Rapid heart rate, fainting, cyanosis | CPR, defibrillation | Antiarrhythmic medications, cardioversion |
| Heart Block | Slow heart rate, dizziness | Observation, atropine (if symptomatic) | Pacing, possible temporary pacing wire |
Management and Treatment
Once the arrhythmia is identified, the treatment protocol varies depending on the severity and type of rhythm disturbance. For example, in cases of supraventricular tachycardia (SVT), vagal maneuvers such as the Valsalva maneuver can often be effective in resetting the heart rate. However, if these methods do not resolve the issue, medications like adenosine may be used to restore a normal rhythm.
For life-threatening arrhythmias such as ventricular tachycardia or complete heart block, immediate intervention is crucial. This may involve advanced treatments like defibrillation or the use of a temporary pacemaker. In some cases, ongoing monitoring and additional therapies may be required to ensure stable heart function and prevent recurrence.
Effective management of pediatric arrhythmias also includes close monitoring of the patient’s vital signs, oxygenation, and overall clinical status. A multidisciplinary approach involving cardiologists, intensivists, and emergency care professionals is often necessary for comprehensive care.
By recognizing the signs and implementing appropriate interventions promptly, healthcare providers can improve outcomes for children experiencing arrhythmias in emergency settings.
Commonly Tested Pediatric Emergency Scenarios
Emergency care providers are often required to respond to a variety of critical situations involving children. These scenarios can range from respiratory distress to cardiac arrest and require rapid, accurate decision-making. Healthcare professionals must be prepared to manage these emergencies effectively, employing a structured approach to care and treatment. This section outlines some of the most commonly tested pediatric emergency situations that healthcare providers may encounter.
In each scenario, timely intervention, clear assessment of the child’s condition, and a solid understanding of treatment protocols are crucial. Knowing how to manage these emergencies not only improves patient outcomes but also helps healthcare providers build the necessary skills for real-life situations. Below are several scenarios frequently encountered in pediatric care assessments.
Respiratory Arrest and Failure
One of the most critical situations involves a child experiencing respiratory arrest or failure. Common causes include airway obstruction, asthma, or severe allergic reactions. In this case, the first priority is to secure the airway and ensure effective oxygenation. Providers must be able to recognize signs of respiratory distress, such as rapid breathing, cyanosis, and inability to speak or cry.
Initial management may include positioning the child, performing basic airway maneuvers, and administering supplemental oxygen. Advanced interventions could involve mechanical ventilation or medication to relieve airway constriction. This scenario tests both knowledge of pediatric airway management techniques and the ability to respond to evolving clinical conditions quickly.
Cardiac Arrest in Children
Another critical situation commonly tested in pediatric care is cardiac arrest. While rare, it can occur as a result of trauma, arrhythmias, or underlying conditions such as congenital heart disease. The scenario requires providers to promptly initiate cardiopulmonary resuscitation (CPR) and defibrillation if indicated.
The provider must be familiar with the proper compression depth and rate for children, as well as the timing of ventilations. Defibrillation with a pediatric-sized defibrillator is typically required if the child is experiencing certain types of arrhythmias, such as ventricular fibrillation or pulseless ventricular tachycardia. This scenario tests both clinical knowledge and the ability to perform CPR in a high-pressure environment.
Severe Trauma and Shock
Severe trauma, such as head injuries or fractures, can lead to shock in pediatric patients. Shock presents as a medical emergency where the circulatory system fails to deliver adequate oxygen and nutrients to tissues. It is essential for healthcare providers to identify the early signs of shock, including tachycardia, weak pulse, cool extremities, and altered mental status.
In these situations, immediate fluid resuscitation, monitoring, and preparation for possible advanced interventions like blood transfusions or surgical intervention are key. This scenario challenges providers to think critically about the need for stabilization and the management of shock in pediatric patients.
Severe Allergic Reactions
Anaphylaxis, a severe allergic reaction, can cause rapid deterioration in pediatric patients. This often involves a sudden onset of respiratory distress, swelling of the throat, and hypotension. Recognizing the signs of anaphylaxis and administering the appropriate treatment, such as epinephrine, is essential for saving the child’s life.
Quick action is critical, and this scenario assesses a provider’s ability to respond to a fast-developing allergic reaction, including airway management, medication administration, and monitoring for any complications that may arise.
Mastering these common scenarios not only helps prepare healthcare providers for exams but also builds their capacity to handle pediatric emergencies with confidence and efficiency in clinical practice.
Role of CPR in Pediatric Emergency Care
Cardiopulmonary resuscitation (CPR) is a vital skill in managing pediatric emergencies, particularly when a child is unresponsive and not breathing. In such critical situations, CPR plays a central role in maintaining circulation and oxygenation, ultimately improving the chances of survival. The technique is fundamental in any pediatric emergency care protocol and is an essential part of assessments designed to test clinical competence in handling life-threatening conditions.
In emergency settings, healthcare providers must demonstrate not only the ability to initiate CPR promptly but also the precision required for performing chest compressions and ventilation. Effective CPR can buy valuable time until more advanced interventions are available, and proper technique can significantly influence outcomes for the child in distress.
Key Components of Pediatric CPR
CPR for children differs in several aspects from adult resuscitation techniques. Below are key components of pediatric CPR that healthcare providers need to master:
| Component | Details |
|---|---|
| Compression Depth | For infants, compress the chest about 1.5 inches (4 cm); for children, compress about 2 inches (5 cm). |
| Compression Rate | Perform chest compressions at a rate of 100-120 per minute, ensuring good recoil. |
| Compression-to-Ventilation Ratio | For a single rescuer, the ratio is 30:2. For two rescuers, it is 15:2. |
| Airway Management | Ensure the airway is open using the head-tilt-chin-lift maneuver, and provide rescue breaths. |
| Defibrillation | Use an AED with pediatric pads if available, or adult pads in a child who weighs more than 25 kg (55 lbs). |
These guidelines ensure that CPR is delivered effectively, with the proper depth, rate, and technique to enhance survival outcomes. A failure to maintain correct compression depth or a misstep in ventilation technique can lead to less efficient blood circulation and oxygenation, ultimately affecting the outcome of resuscitation efforts.
Importance of Timely Intervention
The timing of CPR intervention is crucial. Prompt recognition of cardiac arrest or respiratory failure followed by immediate CPR can double or triple the chance of survival. It is also important to continue CPR without interruption until advanced medical personnel or equipment takes over. The role of CPR is not just about administering chest compressions and ventilation; it also includes recognizing when to switch to defibrillation or provide medications to stabilize the child.
In pediatric emergency care assessments, proficiency in CPR is often tested to ensure healthcare providers are ready to act swiftly and effectively. Mastery of CPR techniques is a critical aspect of pediatric resuscitation training and contributes significantly to the overall quality of emergency care provided to young patients.
How to Manage Pediatric Shock
Pediatric shock is a life-threatening condition that requires rapid identification and intervention to prevent organ failure and improve the chances of recovery. It occurs when the body’s circulatory system is unable to provide adequate oxygen and nutrients to tissues, leading to a state of cellular dysfunction. Understanding the various types of shock, recognizing the early signs, and applying the appropriate interventions are crucial in managing this emergency effectively.
Shock can manifest in several forms, including hypovolemic, distributive, cardiogenic, and obstructive shock, each with its own underlying causes and treatment approaches. Early recognition and immediate action are key to stabilizing the child and preventing further complications. In this section, we will outline the steps for managing pediatric shock, focusing on assessment, fluid resuscitation, and monitoring vital signs.
Steps for Initial Management of Shock
- Assess the Airway and Breathing: Ensure the child’s airway is clear and provide appropriate oxygenation if necessary. Respiratory support is vital for restoring oxygen levels in the bloodstream.
- Evaluate Circulation: Check the child’s pulse, blood pressure, and perfusion. Immediate interventions, such as IV fluid administration or medication, may be required depending on the type of shock.
- Identify the Underlying Cause: Determine whether the shock is due to blood loss, infection, heart failure, or obstruction. This helps guide the treatment strategy.
- Initiate Fluid Resuscitation: Administer isotonic saline or Ringer’s lactate as the first line of treatment for most types of shock, especially hypovolemic shock.
Types of Pediatric Shock and Management
Managing pediatric shock effectively requires understanding the different types, each of which requires a tailored approach:
- Hypovolemic Shock: Caused by a significant loss of blood or fluids, this type of shock is treated with aggressive fluid resuscitation to restore circulating volume.
- Distributive Shock: Often caused by sepsis or anaphylaxis, this shock type results from blood vessel dilation, leading to poor perfusion. Treatment may include antibiotics, antihistamines, or vasopressors.
- Cardiogenic Shock: Occurs when the heart is unable to pump effectively. It is often treated with medications to improve heart function and may require inotropic support.
- Obstructive Shock: Caused by physical blockages, such as a pulmonary embolism or tension pneumothorax. Treatment typically involves relieving the obstruction and providing supportive care.
Continuous monitoring of the child’s response to treatment is essential for guiding further interventions. Tracking changes in vital signs, oxygen levels, and fluid balance allows healthcare providers to adjust the treatment plan accordingly and ensure the child’s condition improves.
Managing pediatric shock requires a systematic, methodical approach that prioritizes rapid action and targeted interventions. The earlier the shock is recognized and treated, the better the chances of a positive outcome for the child.
Improving Your Confidence for the Exam
Approaching an exam with confidence is key to performing well, especially in high-pressure scenarios. The ability to stay calm, focused, and prepared can make all the difference in your results. Confidence doesn’t come overnight, but with the right strategies, you can significantly enhance your readiness and mindset. In this section, we’ll explore effective methods to boost your confidence and reduce anxiety as you prepare for the test.
Key Strategies to Build Confidence
- Thorough Preparation: The more prepared you are, the more confident you will feel. Spend time reviewing key topics, and break your study sessions into manageable chunks to avoid feeling overwhelmed.
- Practice Under Test Conditions: Simulate the actual exam environment by timing yourself during practice tests. This can help you become accustomed to the pressure and improve your time management skills.
- Understand Your Weak Points: Identify areas where you feel less confident and dedicate extra time to mastering those concepts. Strengthening your weaknesses will make you feel more capable and secure in your knowledge.
- Positive Visualization: Visualizing success can help reduce anxiety and increase your confidence. Take a few minutes before each study session or the actual exam to picture yourself answering questions successfully and remaining calm under pressure.
Mindset Techniques to Enhance Performance
- Stay Positive: A positive attitude can influence your ability to retain information and think clearly during the exam. Avoid negative self-talk and focus on what you know rather than what you don’t.
- Take Care of Your Well-being: Rest, nutrition, and exercise play a significant role in maintaining mental clarity. Make sure you’re getting enough sleep, eating healthy, and managing stress leading up to the exam.
- Focus on the Process, Not the Outcome: Concentrate on doing your best rather than obsessing over the result. A focus on effort and progress can help alleviate performance anxiety.
By using these techniques and maintaining a focused approach, you can build confidence and improve your overall exam performance. Remember that consistent preparation and a positive mindset are powerful tools to help you succeed.
Sample Questions from the 2025 Preparation Course
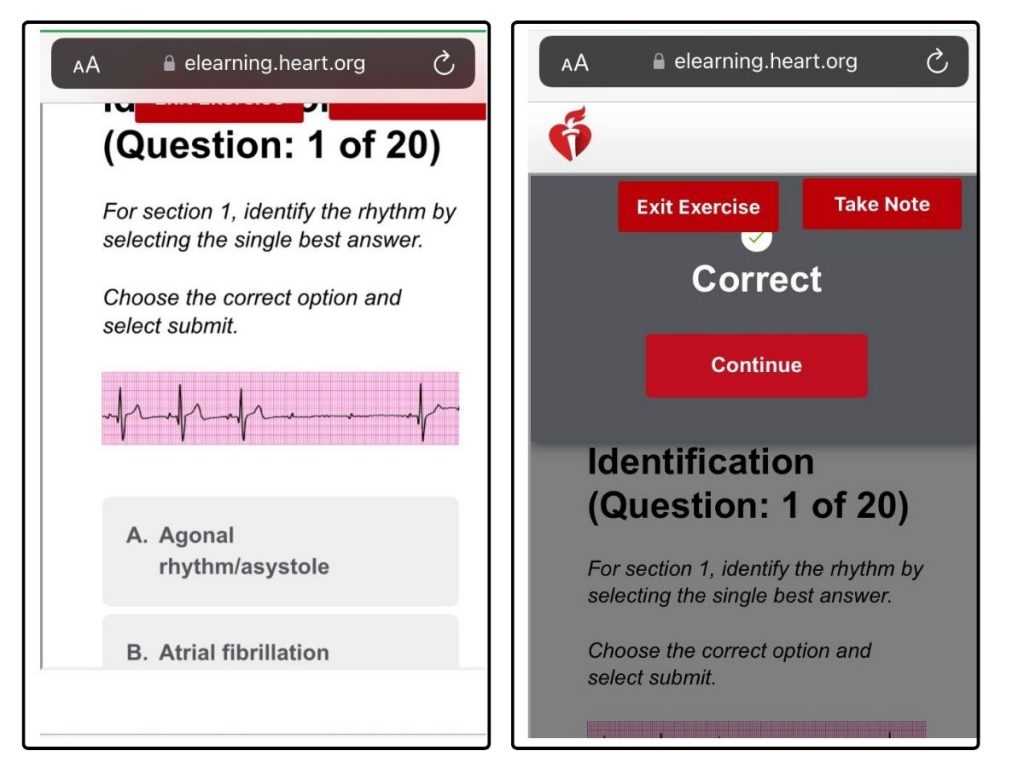
One of the most effective ways to prepare for any exam is to familiarize yourself with the types of questions you may encounter. This section offers examples of questions commonly found in preparatory courses for medical professionals, aimed at testing critical knowledge in emergency care. Reviewing these sample questions can help you gauge the level of difficulty, the range of topics covered, and improve your ability to respond quickly and accurately during the actual evaluation.
Types of Questions You May Encounter
These sample questions focus on a range of topics relevant to pediatric emergency care. They are designed to test both theoretical knowledge and practical application in urgent clinical situations.
- Clinical Scenario: A 5-year-old child presents to the emergency room with labored breathing and a heart rate of 150 bpm. What is your first course of action?
- Knowledge of Drugs: Which medication would be most appropriate for a child in severe respiratory distress with suspected asthma exacerbation?
- Diagnostic Interpretation: A 3-year-old child has a heart rate of 80 bpm, with a blood pressure of 70/40 mmHg. What is the most likely diagnosis?
- Emergency Procedure: You are required to administer chest compressions to an infant in cardiac arrest. What is the correct technique?
Understanding the Questions
These sample questions help test your ability to recall essential knowledge and apply it under pressure. They are based on scenarios you may face in a clinical setting, requiring you to make fast, informed decisions. The goal is to assess your readiness for real-world situations and ensure that you are capable of performing life-saving interventions efficiently.
Familiarizing yourself with these types of questions is an important part of your preparation. It will not only boost your confidence but also sharpen your critical thinking and decision-making skills when faced with pediatric emergencies.
Where to Find Reliable Resources for Pediatric Emergency Care
In order to successfully prepare for any pediatric emergency care evaluation, it is crucial to access trustworthy materials. The right resources can enhance your understanding, provide accurate information, and ensure that you are well-prepared for critical situations. This section will highlight some of the best places to find reliable learning tools and references, helping you stay current and well-informed.
Top Sources for Reliable Information
Here are several sources where you can find quality resources for mastering pediatric emergency care principles:
- Official Medical Organizations: Leading health organizations, such as the American Heart Association (AHA), offer comprehensive guidelines and study materials that are regularly updated. Their online platforms often include e-learning modules, webinars, and downloadable resources.
- Medical Journals and Research Papers: Peer-reviewed journals are excellent for accessing the latest studies and clinical guidelines. Platforms like PubMed and Google Scholar allow you to search for specific topics related to pediatric emergencies and treatments.
- Medical Textbooks: Comprehensive textbooks on pediatric care are an invaluable resource. These texts often provide detailed, evidence-based content covering a range of topics from basic emergency care to complex procedures.
- Online Learning Platforms: Websites such as Coursera, MedEdPORTAL, or other specialized educational platforms offer free and paid courses specifically designed for healthcare professionals. These courses can help you prepare for exams and improve your practical knowledge.
- Peer Support and Forums: Online forums and communities for healthcare professionals, such as Medscape or Reddit’s medical threads, can be helpful for sharing insights, asking questions, and discussing case studies with others in the field.
Books and Study Guides
There are many highly regarded books that serve as comprehensive study guides for pediatric emergency care. Some of the top recommendations include:
- “Pediatric Emergency Medicine” by Peter S. Horn – This book provides in-depth coverage of pediatric emergencies, including clear protocols and practical case studies.
- “Advanced Pediatric Life Support: The Pediatric Emergency Medicine Resource” – A well-structured guide focused on real-world applications and emergency response techniques.
- “Emergency Medicine: A Comprehensive Study Guide” by Judith E. Tintinalli – Though not exclusively pediatric, this resource is widely regarded as one of the most thorough guides in emergency medicine.
By utilizing these sources, you can ensure that your preparation is based on solid, up-to-date, and trusted information. Whether you are studying on your own or with a group, these resources will provide the necessary foundation for success.
What to Do After Completing the Evaluation
Once you have completed the evaluation, it is important to take a strategic approach to the next steps in order to maximize your learning and ensure you are well-prepared. Reflecting on your performance and taking the necessary actions based on your results will help you identify areas for improvement and solidify your understanding of the material. Here are the key steps to follow after finishing your evaluation.
Review Your Results
Start by thoroughly reviewing your results. Focus on areas where you may have struggled or received lower scores. This step is crucial for understanding your strengths and weaknesses, which will guide your future study efforts. Make note of any concepts or topics that need further attention.
- Identify Knowledge Gaps: Look for patterns in the areas where you scored lower. If you find recurring topics, it could indicate a need for deeper study in those specific areas.
- Understand Mistakes: Review the questions you answered incorrectly and understand why the correct answers are what they are. This will help clarify any misconceptions.
Make a Plan for Improvement
After analyzing your results, it is time to make a plan for improvement. Focusing on the weaker areas you identified will allow you to concentrate your efforts where they are most needed. Break down the topics into manageable sections and allocate time to review each one thoroughly.
- Use Trusted Resources: Use reliable textbooks, online courses, or medical journals to strengthen your knowledge of the areas you need to improve.
- Practice with Scenarios: Engage in case study scenarios to apply the theoretical knowledge you’ve gained. This practical approach will help reinforce your understanding and build confidence.
Stay Up-to-Date
The field of pediatric emergency care is always evolving, so it’s important to stay current with the latest guidelines, research, and practices. Regularly reviewing updated materials will help you remain prepared and informed.
- Participate in Continuing Education: Look for webinars, workshops, or additional courses that focus on advanced techniques and newer practices in pediatric care.
- Join Professional Communities: Engage with peer groups, both online and in person, to discuss new research and share knowledge with other professionals in the field.
By reflecting on your performance and actively addressing areas for improvement, you will be well-positioned for future success in pediatric care scenarios. Consistent learning and practice are key to becoming more proficient in this field.