For professionals working in healthcare support roles, grasping the legal and ethical frameworks that govern their practice is essential. These guidelines ensure both the safety of patients and the integrity of the profession. Knowledge of the relevant laws and regulations plays a critical part in shaping a competent and responsible healthcare provider. A solid understanding of these principles not only helps professionals avoid legal pitfalls but also enhances the quality of care they offer to patients.
In this section, we will explore the core principles that support the operational standards of healthcare support work. We will focus on the key legal concepts that every professional should be familiar with to navigate their responsibilities effectively. It is vital to comprehend the relationship between law and daily tasks, as well as the boundaries set by governing bodies to protect both the practitioners and the individuals they serve.
Preparation for any knowledge assessment on this subject involves more than just memorizing laws; it requires applying these concepts in practical situations. Professionals need to understand how legal frameworks influence the scope of their responsibilities and how they can ensure compliance. Mastery of these elements fosters confidence and competence, helping to avoid potential legal conflicts in the future.
Understanding Legal Responsibilities in Healthcare Practice
In any healthcare-related role, understanding the scope of legal obligations is crucial. Professionals must be aware of their duties, rights, and the potential consequences of their actions. Legal responsibilities ensure that individuals working in healthcare settings operate within the boundaries of established laws, maintaining both ethical standards and patient safety. Familiarity with these responsibilities helps to prevent malpractice and ensures that care is delivered appropriately.
Key Legal Principles for Healthcare Professionals
Healthcare practitioners are bound by various laws that dictate the standards of care and interactions with patients. These laws cover a range of topics, including patient privacy, informed consent, and the handling of medical records. Knowing these key principles can guide decision-making processes and minimize risks associated with non-compliance.
| Legal Principle | Description |
|---|---|
| Patient Confidentiality | Protecting patient information from unauthorized access, in line with privacy regulations. |
| Informed Consent | Ensuring patients understand and agree to treatment plans before procedures are carried out. |
| Scope of Practice | Clarifying the tasks and duties a professional is legally authorized to perform. |
Consequences of Legal Violations
Failure to adhere to legal requirements can result in significant consequences, ranging from professional disciplinary action to legal prosecution. Violations can damage reputations, disrupt careers, and compromise patient trust. It is important to regularly review and understand the laws governing one’s practice to avoid such outcomes.
Key Laws Governing Healthcare Practices
The healthcare industry is regulated by a variety of laws designed to ensure patient safety, quality of care, and ethical standards. These laws define the legal framework within which healthcare professionals operate, outlining their duties and responsibilities. Understanding the most important regulations is essential for anyone working in healthcare-related roles, as they directly affect day-to-day activities and interactions with patients.
Among the key legal areas that govern practice are those that address patient rights, confidentiality, and professional conduct. These regulations protect both patients and practitioners by establishing clear guidelines and expectations. Adherence to these laws ensures the integrity of the profession and minimizes the risk of legal complications.
Health Insurance Portability and Accountability Act (HIPAA) is one of the most crucial regulations concerning patient privacy. This law mandates that healthcare providers safeguard sensitive patient information and restricts unauthorized access. Practitioners must ensure that patient records are kept confidential and that any sharing of information is done only with explicit consent.
Informed Consent is another foundational concept. Healthcare providers must fully explain treatment options, procedures, and potential risks to patients, ensuring they make informed decisions before any procedure is carried out. This law upholds the principle that patients have the right to autonomy over their healthcare decisions.
Scope of Practice laws define the boundaries within which healthcare professionals can perform their duties. These regulations outline specific tasks that individuals are permitted to carry out based on their qualifications and licensure, preventing overstepping of professional limits.
Scope of Healthcare Support Professionals’ Practice
The scope of practice for healthcare support professionals defines the tasks and responsibilities they are legally authorized to perform. These guidelines ensure that practitioners operate within their competencies and qualifications, protecting both the patients and the professionals themselves. By understanding the limits and expectations of their role, healthcare workers can avoid legal issues and provide effective support to the healthcare team.
Typically, healthcare support professionals are responsible for assisting in various clinical and administrative tasks. The scope of their duties varies by region and is often determined by state regulations, licensing requirements, and the specific needs of the practice. These professionals are expected to work under the supervision of licensed healthcare providers, ensuring that all activities align with the established standards of care.
Some common tasks include patient preparation, assisting during procedures, sterilization of instruments, and managing patient records. However, it is crucial to understand that there are strict boundaries regarding what can and cannot be performed independently. For example, certain clinical procedures and decision-making responsibilities must always be carried out by a licensed professional, such as a doctor or dentist.
In some regions, the scope of practice is expanded through additional certifications or training, allowing professionals to perform a broader range of tasks. It is important for healthcare support professionals to stay informed about changes in regulations and guidelines to ensure they are practicing legally and competently.
Ethical Standards in Healthcare Work
Ethical standards in healthcare are essential for maintaining professionalism, trust, and patient safety. These principles guide healthcare providers in making decisions that prioritize the well-being of patients while adhering to legal and moral obligations. Ethical conduct ensures that healthcare professionals act in the best interests of those they care for and operate with integrity in all aspects of their work.
Core Ethical Principles
Healthcare professionals are expected to follow several fundamental ethical guidelines. These principles, such as beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), and autonomy (respecting patients’ rights to make informed decisions), form the foundation of ethical practice. Practitioners must always strive to uphold these values, ensuring that their actions are guided by respect for patient dignity and rights.
Professional Conduct and Integrity
Maintaining integrity and professionalism is crucial in healthcare work. Providers are expected to demonstrate honesty, transparency, and accountability in their interactions with patients and colleagues. Upholding high standards of ethical behavior fosters trust and strengthens the patient-provider relationship. This also extends to ensuring confidentiality and providing accurate information at all times.
Adhering to ethical guidelines not only protects the well-being of patients but also supports a positive and respectful healthcare environment. Professionals must be aware of ethical dilemmas that can arise in practice and navigate these challenges with care, always prioritizing the welfare of those they serve.
Preparing for Legal Knowledge Assessments
Preparing for legal knowledge assessments in healthcare requires a clear understanding of the relevant laws, ethical standards, and professional responsibilities that govern the field. These evaluations test not only theoretical knowledge but also the practical application of legal principles in everyday practice. Successful preparation involves both memorizing key concepts and developing the ability to apply them effectively in real-world scenarios.
To begin, it is important to focus on the core areas that will be covered in the assessment. These may include regulations surrounding patient care, privacy laws, scope of practice, and the ethical responsibilities of healthcare providers. A thorough understanding of these topics is essential for navigating the legal landscape of healthcare work confidently.
Additionally, practicing with sample questions and case studies can help reinforce knowledge and improve test-taking strategies. Familiarizing oneself with common legal scenarios and how to address them can provide valuable insights into how questions may be structured. It is also beneficial to review any relevant state or regional laws, as these can vary and may be a focus of the assessment.
Ultimately, consistent study, active engagement with legal materials, and mock testing are crucial for building confidence and mastering the necessary legal concepts. Preparing well ensures that professionals can not only pass their evaluations but also excel in providing ethical and lawful care to their patients.
Common Legal Issues in Healthcare Practices
In healthcare, professionals often face various legal challenges that can arise from patient interactions, procedural errors, and ethical dilemmas. These issues can have serious implications for both the practitioners and the individuals they serve. Being aware of these common legal matters helps professionals navigate their responsibilities effectively and minimize the risk of legal complications.
One common issue involves patient consent. Healthcare providers are required to fully inform patients about procedures, risks, and alternatives before any treatment is administered. Failure to obtain informed consent can lead to legal claims of malpractice or negligence. It is essential that practitioners ensure clear communication and obtain written consent in every instance where it is required.
Confidentiality is another critical legal consideration. Professionals are legally bound to protect patient privacy, following laws such as the Health Insurance Portability and Accountability Act (HIPAA). Unauthorized disclosure of patient information can result in severe legal penalties, including fines and loss of professional licensure.
Scope of practice is another area where legal issues often arise. Healthcare practitioners must work within the legal boundaries of their professional roles, as defined by state and local regulations. Overstepping these boundaries can lead to disciplinary action and, in some cases, legal prosecution. It is important for professionals to understand the limitations of their role and seek guidance when unsure about their responsibilities.
Lastly, issues related to negligence and malpractice are frequent concerns. Errors in treatment, inadequate supervision, or failure to meet professional standards can result in lawsuits. Practitioners must adhere to established protocols and guidelines to minimize the risk of negligence claims.
Impact of State Regulations on Healthcare Support Professionals
State regulations play a crucial role in shaping the scope of practice, responsibilities, and professional conduct of healthcare support workers. These laws set specific guidelines for what duties can be performed, the qualifications required, and the ethical standards to follow. Understanding the impact of these regulations is essential for anyone working in healthcare, as they directly affect daily tasks, career advancement, and legal compliance.
Regulatory Authority and Licensing
Each state has its own regulatory body responsible for overseeing the certification and licensing of healthcare professionals. These organizations establish the qualifications, training requirements, and continuing education necessary to maintain licensure. The laws they enact define the boundaries of a professional’s role and determine whether additional certifications or permissions are required to perform certain tasks. Without a clear understanding of these state-specific rules, practitioners may inadvertently overstep their legal limits, leading to penalties or loss of licensure.
Variations Across States
It is important to note that regulations vary significantly between states. While some states may have broad allowances for healthcare support roles, others impose strict limitations on the duties these professionals can undertake. For example, some states may permit a wider range of clinical functions, while others may only allow specific administrative tasks. Healthcare workers need to stay informed about the specific laws in their state to ensure compliance and to avoid conflicts with regulatory authorities.
Role of Licensure in Healthcare Practice
Licensure is a critical aspect of healthcare practice, as it ensures that professionals have met the required standards of education, training, and competency. By granting licensure, regulatory bodies confirm that individuals possess the necessary skills and knowledge to provide safe and effective care. This process not only protects patients but also upholds the integrity of the healthcare profession, establishing a framework for accountability and trust.
Requirements for Obtaining Licensure
To obtain licensure, individuals must typically complete a specific educational program, pass relevant examinations, and meet continuing education requirements. The criteria for licensure may vary depending on the profession and the region, but the goal remains the same: to ensure that those entering the healthcare field are qualified to perform their roles effectively and ethically. For instance, licensure may require passing written and practical exams that test both theoretical knowledge and practical skills.
Impact on Professional Practice
Licensure has a significant impact on the practice of healthcare professionals. It serves as a formal recognition of an individual’s ability to perform their job within the boundaries of established standards. In addition to ensuring that practitioners have the requisite skills, licensure also provides a legal framework for accountability. Those who are licensed are held to professional and ethical standards, and failure to adhere to these standards can result in disciplinary action, including loss of licensure.
| Licensure Requirement | Purpose | Outcome |
|---|---|---|
| Education and Training | Ensure fundamental knowledge and skills | Prepared to perform duties safely and competently |
| Examinations | Assess understanding and practical application | Verify competency in required tasks |
| Continuing Education | Keep skills up-to-date and improve knowledge | Maintain licensure and stay current in the field |
Confidentiality and Patient Rights
Confidentiality is a cornerstone of trust between healthcare providers and patients. Protecting sensitive information ensures that individuals feel secure when seeking medical care, knowing their personal details will remain private. Alongside confidentiality, patient rights are fundamental principles that guarantee individuals are treated with respect, informed of their options, and empowered to make decisions regarding their healthcare.
One of the key aspects of patient confidentiality is the protection of medical records. Providers are legally required to safeguard patient information from unauthorized access or disclosure. Breaches of confidentiality, whether intentional or accidental, can lead to serious legal consequences, including fines and professional sanctions. It is essential for healthcare workers to be aware of the legal frameworks in place to protect patient privacy, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States.
Patient rights encompass a variety of protections, including the right to informed consent, the right to refuse treatment, and the right to access one’s medical records. These rights ensure that patients have control over their own healthcare decisions. Healthcare professionals must uphold these rights by providing clear, honest information and respecting the choices made by patients, as long as those choices do not endanger their health or well-being.
Understanding Professional Boundaries
Maintaining professional boundaries is essential for ensuring a safe and respectful environment in healthcare settings. These boundaries define the appropriate limits for interactions between healthcare providers and patients, helping to prevent conflicts of interest, exploitation, or misunderstandings. Understanding where these lines are drawn is crucial for fostering trust and ensuring ethical conduct in all aspects of care.
Key Principles of Professional Boundaries
There are several core principles that guide the establishment and maintenance of professional boundaries in healthcare:
- Respect for Personal Space: Always maintain appropriate physical distance unless necessary for treatment.
- Clear Communication: Use respectful and professional language at all times. Avoid personal or overly familiar conversations.
- Confidentiality: Protect patient privacy and sensitive information to prevent unauthorized access or disclosure.
- Avoiding Conflicts of Interest: Do not engage in relationships that could interfere with professional duties or objectivity.
Recognizing Boundaries in Practice
It is important to recognize when professional boundaries are being crossed, either by the provider or the patient. Some common situations that may challenge these boundaries include:
- Personal Relationships: Engaging in personal relationships with patients outside the professional setting can compromise objectivity and create conflicts of interest.
- Gift-Giving: Accepting or giving personal gifts can lead to ethical dilemmas, as it may imply favoritism or a breach of professionalism.
- Overstepping Role Limits: Healthcare providers must stay within the scope of their defined role and avoid performing tasks outside their expertise or legal boundaries.
By consistently adhering to professional boundaries, healthcare providers ensure they act ethically, maintain patient trust, and prevent misunderstandings that could lead to legal or professional complications.
Legal Consequences of Violating Healthcare Regulations
Failure to comply with healthcare laws and regulations can lead to serious legal repercussions. Professionals in the healthcare field are expected to adhere to strict guidelines that govern their practice, from licensing and patient care to ethical conduct. Violating these rules not only jeopardizes patient safety but also exposes individuals to legal actions, fines, or even the loss of their professional license.
Types of Legal Violations
Healthcare workers may face various legal violations, including but not limited to:
- Unlicensed Practice: Practicing without the required certification or outside the scope of authorized duties.
- Negligence: Failure to provide adequate care, leading to patient harm or injury.
- Fraud: Providing false information on patient records, billing practices, or other official documents.
- Invasion of Privacy: Unauthorized sharing of patient information or violating confidentiality agreements.
Potential Legal Penalties
The consequences of violating healthcare regulations can vary depending on the severity of the offense, but typical legal penalties include:
| Violation | Potential Penalty |
|---|---|
| Unlicensed Practice | Fines, imprisonment, suspension or revocation of professional license |
| Negligence | Monetary damages, loss of license, lawsuits |
| Fraud | Criminal charges, civil penalties, prison time |
| Invasion of Privacy | Legal fines, loss of employment, lawsuits |
Healthcare professionals must be vigilant about their legal responsibilities to avoid these penalties and maintain a reputation for trustworthiness and competence in their field.
Test-Taking Strategies for Legal Knowledge Assessments
Preparing for legal knowledge assessments requires a focused approach, as these tests often involve complex concepts and detailed regulations. Developing effective strategies for navigating through these assessments can make a significant difference in performance. By mastering certain techniques and practicing key skills, candidates can enhance their chances of success and minimize test-related stress.
Effective Preparation Techniques
To ensure readiness for a legal knowledge assessment, consider these strategies:
- Understand the Core Material: Prioritize studying the most relevant legal concepts and regulations. Review official guidelines, state laws, and professional codes of conduct that are likely to appear in the test.
- Practice Past Questions: Familiarize yourself with the format of the questions by practicing with past assessments. This helps you get accustomed to the types of questions and how they are structured.
- Create a Study Schedule: Break down your study time into manageable sessions and focus on one topic at a time. Consistency over time is key to mastering complex content.
- Join Study Groups: Collaborating with peers in study groups can provide diverse insights into challenging topics and improve retention through discussion.
Test-Taking Tips
On the day of the assessment, these tips can help you navigate the test with confidence:
- Read Each Question Carefully: Ensure you understand what is being asked before selecting an answer. Look for key phrases that indicate the best response.
- Eliminate Clearly Wrong Answers: Narrow down your choices by eliminating any answers that are clearly incorrect. This increases your chances of selecting the right option.
- Manage Your Time: Keep track of time and pace yourself throughout the test. If you’re stuck on a question, move on and return to it later if needed.
- Stay Calm and Focused: Stress can hinder your performance, so maintain a calm demeanor. Take deep breaths and stay focused on one question at a time.
By applying these strategies, you can boost your confidence and improve your performance in legal assessments, ensuring that you are well-prepared to succeed.
Common Misconceptions About Healthcare Regulations

There are several misunderstandings when it comes to the rules and regulations governing healthcare practices. Many individuals in the field may be unsure of their legal responsibilities or may incorrectly assume certain practices are permitted. These misconceptions can lead to unintentional violations and legal challenges, making it essential to clarify the truth behind common myths surrounding healthcare law.
Misunderstood Legal Expectations
Here are some of the most frequent misconceptions related to healthcare laws:
- Assumption of Automatic Knowledge: Some professionals believe that they automatically know all the legal requirements simply by being trained in their field. In reality, laws and regulations often change, and ongoing education is necessary to stay compliant.
- Unawareness of Scope Limitations: Many assume they can perform certain tasks simply because they were taught them during their training. However, there are specific legal boundaries that define the scope of what one can and cannot do within their role.
- Confusion Between Ethical and Legal Obligations: While ethical guidelines and legal laws may overlap, they are not the same. Legal standards are enforceable by law, whereas ethical standards are more about professional integrity and personal values.
- Misinterpretation of Patient Confidentiality: Some believe that any discussion about a patient’s condition is permissible as long as it doesn’t involve sensitive details. However, strict privacy laws govern the sharing of patient information.
Legal Consequences of Misunderstandings
Failing to address these misconceptions can lead to serious legal issues. For instance, performing tasks outside the scope of one’s certification can result in penalties, including loss of professional license or even legal prosecution. It is critical to stay informed and adhere strictly to the rules governing the practice to avoid unintended violations.
By correcting these misconceptions, healthcare professionals can ensure they meet the legal standards required for safe and responsible practice.
How to Interpret Legal Terms in Healthcare
Interpreting legal terms accurately is crucial for anyone working in healthcare. Legal language is often complex, and understanding the meaning behind specific terms can significantly impact how one practices and adheres to regulations. A clear grasp of legal terminology ensures that professionals can navigate laws effectively, make informed decisions, and avoid unintentional violations.
Here are some strategies for interpreting legal terms in healthcare:
- Familiarize Yourself with Common Legal Phrases: Many legal terms are used repeatedly across different healthcare laws. Learning these common phrases, such as “informed consent” or “scope of practice,” will make it easier to understand their context in various situations.
- Break Down Complex Definitions: Legal definitions often consist of several components. Take the time to break down the term into its parts and understand each word’s meaning individually before putting them together. This approach can help clarify the overall meaning.
- Consult Legal Resources: If a term is unfamiliar, use legal dictionaries, official statutes, or consult a legal professional for clarification. Many healthcare-specific legal guides are available to help interpret complex terms.
- Understand Context: The meaning of legal terms can change depending on the context in which they are used. Always consider the surrounding legal text to better understand the application of a term.
By mastering legal terminology, professionals in healthcare can ensure they are following the correct procedures, providing safe services, and minimizing the risk of legal issues. A solid understanding of these terms not only protects patients but also upholds the integrity of the healthcare field.
Case Studies in Healthcare Law Practice

Case studies offer valuable insights into the application of legal principles in healthcare settings. By analyzing real-world examples, professionals can better understand how legal issues arise and how to address them effectively. These case studies often highlight common challenges faced by healthcare providers and help illustrate the consequences of failing to adhere to legal requirements.
Here are a few notable case studies that reflect common legal scenarios in healthcare practice:
- Informed Consent Disputes: One common issue involves the failure to properly inform patients about the risks of a procedure. In a recent case, a healthcare provider was sued for negligence when a patient experienced unexpected complications during a routine procedure, claiming they had not been properly informed of the potential risks. This case emphasized the importance of clear communication and documented consent before any treatment.
- Scope of Practice Violations: In another case, a healthcare worker was found to have performed tasks outside their authorized scope, leading to legal consequences. The provider argued that they had been instructed to perform the task by a superior, but the court ruled that the responsibility to understand and adhere to professional boundaries falls on the individual practitioner.
- Patient Confidentiality Breach: A healthcare employee was terminated and faced legal action after they were found to have shared patient information without consent. This case underlined the significance of patient confidentiality laws and the severe penalties for violating them, whether intentional or accidental.
These case studies demonstrate the potential risks and legal consequences associated with various actions in the healthcare field. They serve as reminders that understanding and following the law is crucial for maintaining trust, avoiding litigation, and ensuring the well-being of both patients and professionals.
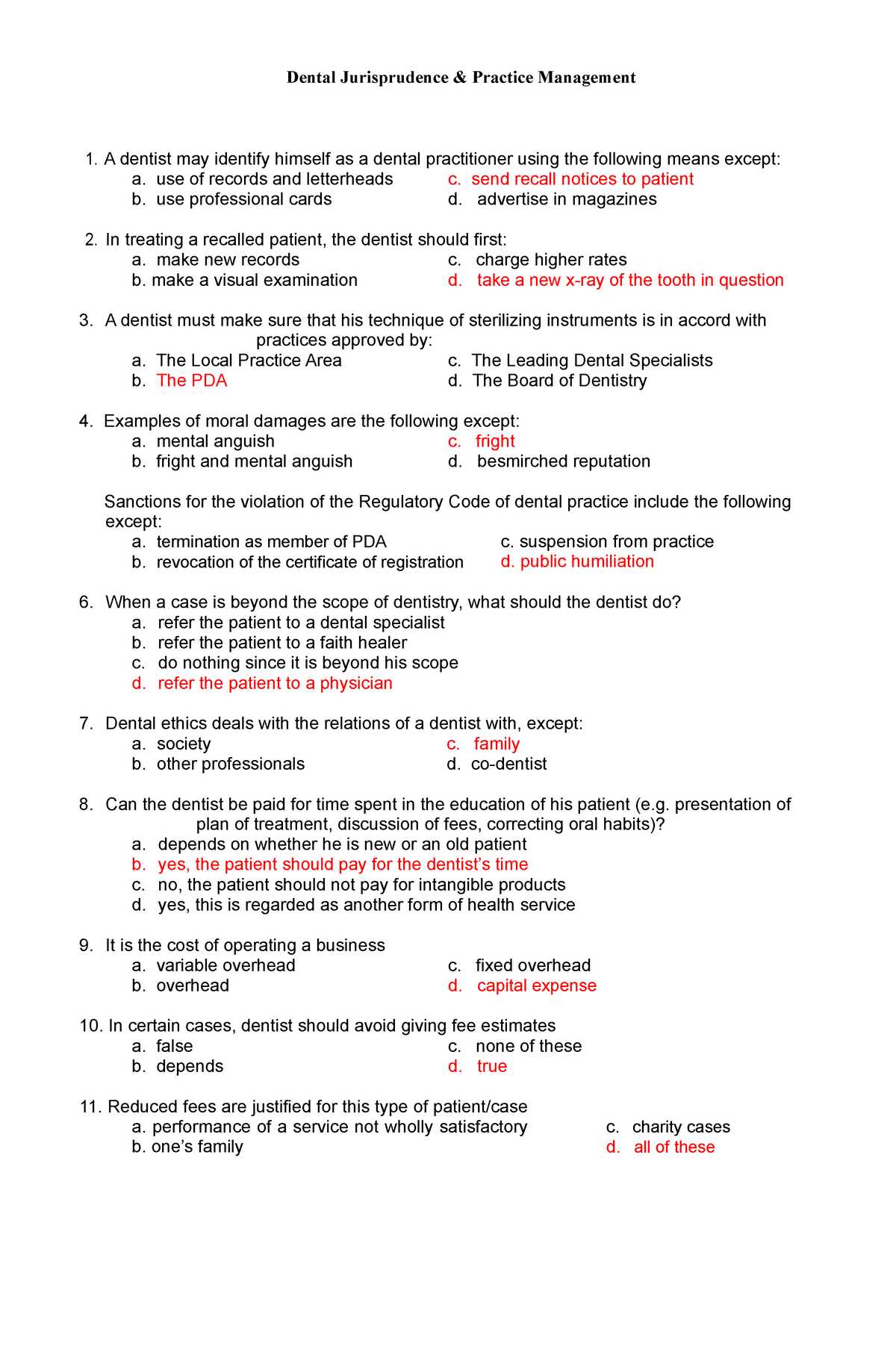
Reviewing Past Test Questions and Responses
Reviewing previous test questions and their corresponding responses is a valuable technique for preparing for any type of professional assessment. This practice helps individuals familiarize themselves with the types of questions they might encounter, the structure of the assessments, and the correct way to approach and answer them. By analyzing past scenarios, one can identify patterns in how questions are framed and better understand the reasoning behind correct responses.
The following steps can guide you through the process of reviewing and learning from previous test materials:
- Identify Key Themes: Examine the topics that were frequently tested in past assessments. This will allow you to prioritize your study sessions and ensure that you focus on the most relevant areas of knowledge.
- Understand Question Formats: Take note of the various question formats, such as multiple-choice, true/false, or case-based queries. Understanding how questions are structured can help you anticipate what to expect in future assessments.
- Analyze Correct Responses: For each question, carefully review the rationale behind the correct answers. Understanding why a particular answer is correct can deepen your comprehension of key concepts and help you apply that knowledge in different contexts.
- Practice with Mock Tests: After reviewing past questions and their answers, take mock tests to simulate the actual testing environment. This will help you improve your time management skills and boost your confidence.
Benefits of Reviewing Past Assessments
By reviewing previous assessments, you not only reinforce your understanding of key concepts but also improve your ability to perform under pressure. It allows you to gauge your progress and identify any gaps in knowledge that need further attention. Ultimately, consistent review helps ensure readiness and boosts overall performance on future evaluations.
Common Mistakes to Avoid
- Relying Solely on Past Questions: While reviewing past tests is helpful, it is important not to focus exclusively on them. Make sure you study the full scope of relevant material to ensure a well-rounded understanding.
- Not Reviewing Mistakes: Simply memorizing answers without understanding why they are correct or incorrect can hinder deeper learning. Take the time to reflect on your mistakes and learn from them.
Maintaining Professionalism in Dentistry
Upholding professionalism within the healthcare field is essential for building trust, ensuring quality care, and fostering a respectful environment for both patients and colleagues. This involves demonstrating a commitment to ethical behavior, adhering to regulatory standards, and maintaining high standards of competence in all aspects of practice. Professionals in this field are expected to represent their profession with integrity and to prioritize the well-being of those they serve.
Key aspects of professionalism in this field include:
- Respectful Communication: Clear and respectful communication with patients, team members, and others is crucial. It helps establish trust and ensures that all parties are informed and comfortable with procedures and treatments.
- Competence and Continuous Learning: Maintaining up-to-date knowledge of best practices, laws, and new technologies is vital. This ensures the quality of care provided is always at its highest level.
- Confidentiality: Protecting patient privacy and respecting their personal information is a fundamental component of professionalism. Professionals must comply with relevant privacy laws and ethical guidelines to safeguard sensitive data.
- Adherence to Ethical Standards: Professionals must follow ethical principles that guide decision-making and patient care. This includes honesty, integrity, and a commitment to doing what is best for the patient.
- Teamwork and Collaboration: Collaboration with colleagues is necessary to ensure effective treatment plans and a smooth working environment. Being an active and supportive team member enhances both patient care and the overall work experience.
Challenges to Maintaining Professionalism
- Burnout: Prolonged stress or emotional exhaustion can affect professional behavior and competence. It is important to manage workload and seek support when needed.
- Ethical Dilemmas: Professionals may encounter situations where there is a conflict between patient desires, ethical principles, and legal obligations. Navigating these challenges requires sound judgment and adherence to ethical guidelines.
Strategies for Upholding Professionalism
- Regular Training and Education: Engaging in ongoing education and training helps professionals stay informed about the latest developments in healthcare standards, regulations, and patient care techniques.
- Clear Boundaries: Establishing and maintaining appropriate boundaries with patients and colleagues ensures that relationships remain professional and respectful.
- Self-Reflection: Regular self-reflection and seeking feedback from others can help identify areas for improvement and encourage personal and professional growth.