When preparing for tests related to the heart and blood vessels, it is essential to focus on the core principles that govern their function. Understanding the mechanisms that control blood flow, the role of the heart in circulation, and how various conditions affect these processes will be key to mastering the material.
Mastering the fundamentals of heart function and vascular health is crucial. From the electrical signals that regulate heartbeat to the different types of blood vessels that support circulation, each component plays an important role in maintaining overall health. Emphasizing these aspects will provide a strong foundation for further study and understanding of related disorders.
Preparing for this topic involves not only memorizing specific terms but also developing a deep understanding of how the body works as a whole. It is important to approach the subject matter by breaking down complex processes into digestible concepts, making it easier to recall under exam conditions.
Heart and Blood Vessel Study Guide
Understanding the functions and mechanisms behind the heart’s operation and the blood flow through the body is critical for mastering related topics. This section highlights important aspects, focusing on the vital processes that maintain healthy circulation and how they can be impacted by various factors.
Key Concepts to Review
The primary focus should be on the heart’s anatomy, how it pumps blood, and the way the circulatory pathways are organized. Knowing how blood moves through different vessels, the role of arteries, veins, and capillaries, and the physiological processes behind blood pressure regulation are essential for grasping the material.
Common Disorders and Treatments
It’s also important to review various conditions that affect heart function, such as hypertension, arrhythmias, and heart failure. Familiarity with diagnostic procedures, treatment strategies, and medications used to manage these conditions will provide deeper insight into the subject.
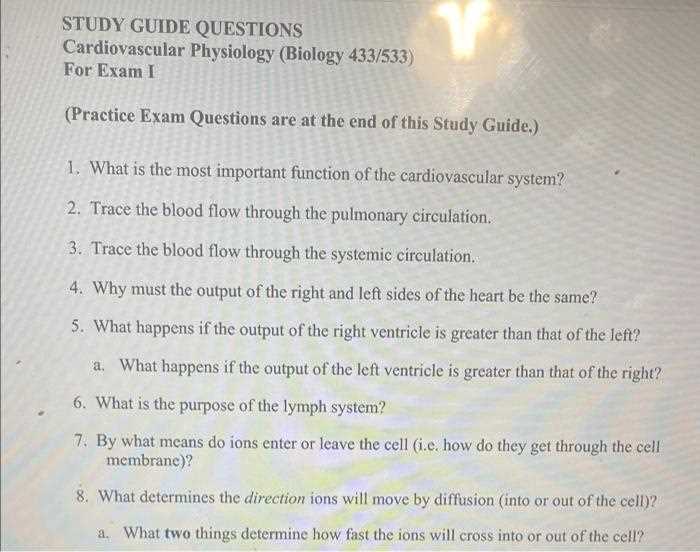
Key Concepts in Cardiovascular Physiology
Grasping the essential principles that govern the functioning of the heart and blood vessels is fundamental for understanding how circulation supports the body. This includes comprehending the processes of blood flow, the mechanical and electrical properties of the heart, and the regulation of pressure within the circulatory network.
Blood Flow and Circulation
The movement of blood throughout the body relies on a continuous and coordinated process. Key concepts to focus on include:
- The path of blood through the heart and major vessels.
- How oxygen and nutrients are delivered to tissues, while waste products are carried away.
- The role of the heart’s chambers in maintaining efficient circulation.
Pressure Regulation
Maintaining proper pressure within the blood vessels is crucial for overall health. Understanding the following will help clarify this process:
- How blood pressure is generated by the heart’s contractions.
- The factors that influence vascular resistance, such as blood volume and vessel elasticity.
- How hormonal and nervous systems contribute to regulating blood flow and pressure.
Important Heart Function Terms to Remember
Familiarity with the key terms related to heart activity is essential for understanding how the organ operates and maintains circulation. These terms are fundamental to grasping how the heart pumps blood, responds to various stimuli, and interacts with other parts of the body to support overall function.
Key Terms to Know
The following terms describe important aspects of heart function:
- Cardiac Cycle: The sequence of events that occur during one heartbeat, including contraction and relaxation phases.
- Stroke Volume: The amount of blood pumped by the heart in one contraction.
- Heart Rate: The number of heartbeats per minute, indicating the speed at which the heart pumps blood.
- Preload: The initial stretching of the heart muscle fibers before contraction, influenced by venous return.
- Afterload: The resistance the heart must overcome to eject blood during contraction.
Electrical Activity of the Heart
The electrical impulses driving the heart’s rhythm are vital to its function. Key terms include:
- SA Node: The natural pacemaker of the heart, initiating the electrical impulses that control heart rhythm.
- AV Node: A cluster of cells that transmits electrical signals from the atria to the ventricles.
- Action Potential: The electrical signal that triggers muscle contraction in the heart.
- ECG: A test that measures the electrical activity of the heart over time.
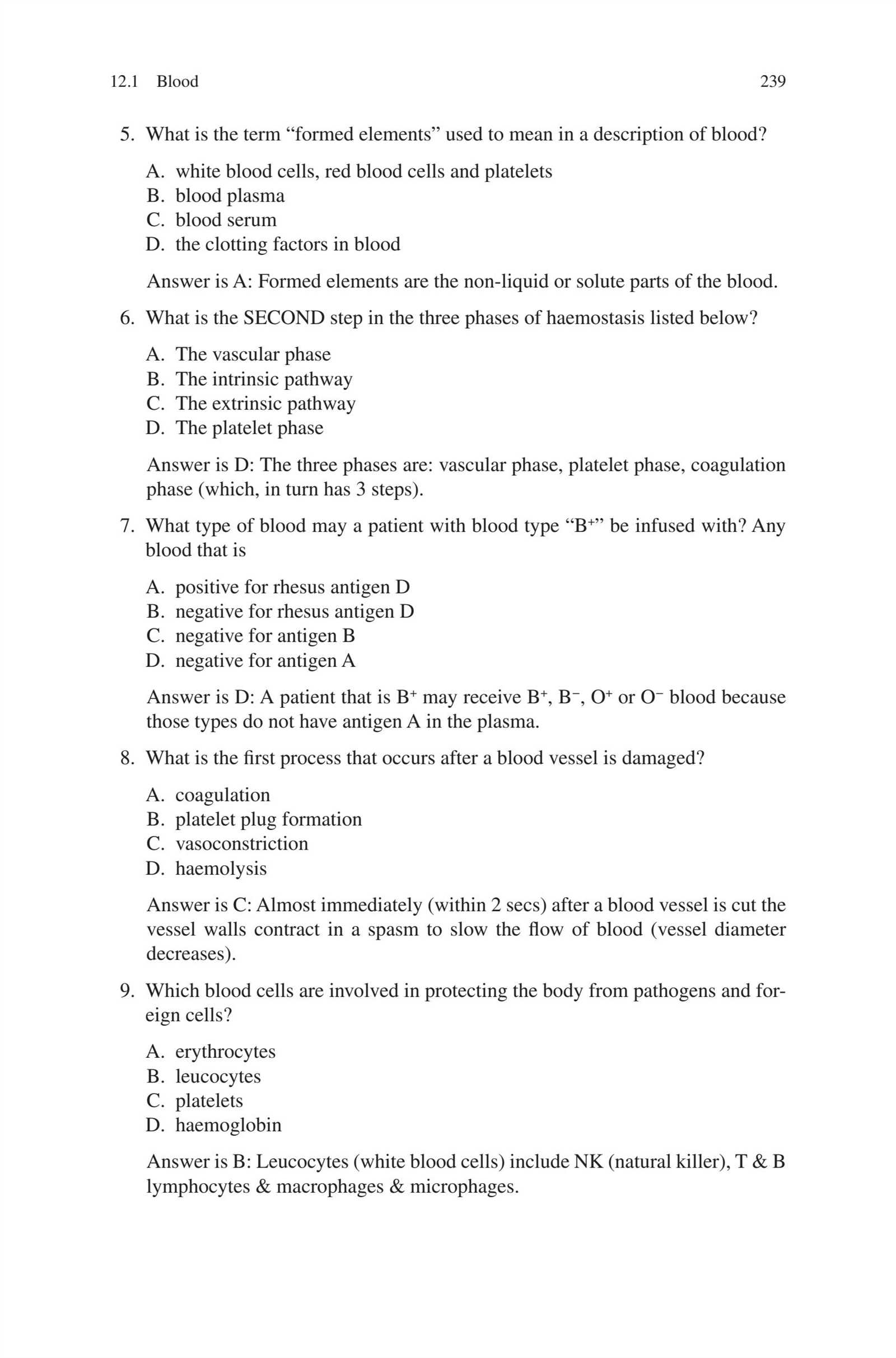
Common Topics on Blood Circulation
Understanding the flow of blood throughout the body is crucial for mastering the core concepts of circulation. Key areas to focus on include how blood travels through different vessels, the factors influencing flow, and how the body regulates this vital process to maintain overall health.
Blood Flow Pathways
The movement of blood is governed by a series of interconnected pathways. Focus on the following aspects:
- Heart Chambers: The role of the atria and ventricles in pumping blood to the lungs and the rest of the body.
- Vascular Network: The structure and function of arteries, veins, and capillaries in transporting blood.
- Pulmonary and Systemic Circulation: The pathways for oxygenated and deoxygenated blood.
Factors Affecting Blood Flow
Several factors influence the efficiency and pressure of blood circulation. Key topics include:
- Vascular Resistance: The role of blood vessel diameter, length, and elasticity in regulating flow.
- Blood Pressure: How heart function, blood volume, and resistance impact overall pressure.
- Cardiac Output: The amount of blood pumped by the heart per minute, influenced by stroke volume and heart rate.
Understanding Blood Vessels and Their Role
Blood vessels play a crucial role in maintaining the body’s circulation, enabling the transport of oxygen, nutrients, and waste products. A clear understanding of how these vessels function is essential for grasping the dynamics of blood flow and the regulation of blood pressure throughout the body.
Types of Blood Vessels

The body relies on three main types of blood vessels, each with distinct characteristics and functions:
- Arteries: These vessels carry oxygen-rich blood away from the heart, with thick walls designed to withstand high pressure.
- Veins: Veins return deoxygenated blood to the heart, featuring valves that prevent backflow as blood moves at lower pressure.
- Capillaries: These tiny vessels connect arteries and veins, facilitating the exchange of gases, nutrients, and waste at the cellular level.
Function of Blood Vessels
Each type of vessel plays an essential role in maintaining proper circulation:
- Oxygen Transport: Arteries deliver oxygenated blood to tissues, while veins carry deoxygenated blood back to the heart.
- Nutrient Exchange: Capillaries allow for the exchange of nutrients and waste products between blood and tissues, supporting cellular function.
- Pressure Regulation: Blood vessels help regulate blood pressure through their elasticity and the contraction of smooth muscle in vessel walls.
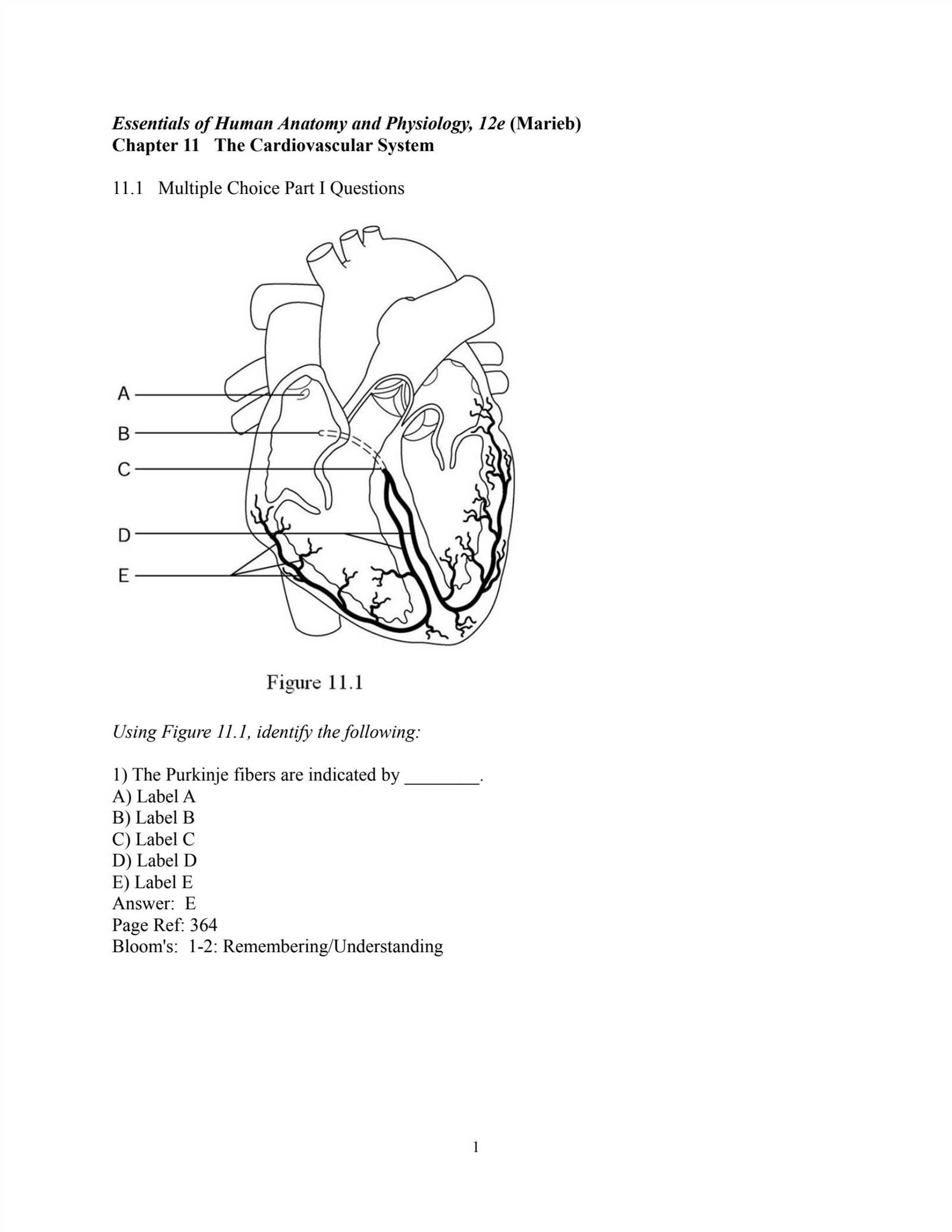
Examining the Heart’s Electrical System
The heart’s ability to maintain a steady rhythm and effectively pump blood throughout the body is driven by a complex electrical network. Understanding how electrical impulses are generated and transmitted within the heart is essential for grasping how this vital organ functions properly.
Key Components of the Heart’s Electrical Network
The heart’s electrical conduction system consists of specialized cells that generate and carry electrical signals, ensuring the heart beats in a coordinated manner:
- SA Node: Known as the natural pacemaker, it initiates the electrical impulses that trigger heartbeats.
- AV Node: Located between the atria and ventricles, it delays the electrical signal slightly before sending it to the ventricles.
- Bundle of His: This pathway carries the electrical impulse from the AV node to the ventricles.
- Purkinje Fibers: These fibers distribute the electrical impulse to the muscle cells of the ventricles, causing them to contract.
How Electrical Impulses Control Heart Rhythm
The electrical impulses travel through the heart at precise intervals, ensuring that the atria and ventricles contract in the correct order. Key points to focus on include:
- Action Potential: The electrical signal that causes heart muscle cells to contract.
- Electrocardiogram (ECG): A test that records the electrical activity of the heart, providing valuable information about its rhythm and function.
- Arrhythmias: Irregular heartbeats that occur when the electrical impulses are disrupted, potentially leading to serious conditions.
Key Diseases Related to the Heart and Blood Vessels
Several conditions can significantly affect the function of the heart and blood vessels, leading to serious health complications. Understanding these diseases is crucial for recognizing risk factors, symptoms, and available treatment options that can improve patient outcomes.
Common Heart-Related Diseases
These diseases directly impact the heart’s ability to pump blood effectively or alter the normal flow of blood through the body:
- Coronary Artery Disease: Occurs when the blood vessels supplying the heart become narrowed or blocked, often leading to chest pain or heart attacks.
- Heart Failure: A condition where the heart is unable to pump blood efficiently, causing symptoms like shortness of breath, swelling, and fatigue.
- Arrhythmias: Irregular heartbeats that can cause the heart to beat too quickly, slowly, or erratically, potentially leading to complications such as strokes.
Vascular Diseases
Conditions affecting blood vessels can impair circulation and lead to increased risks of other health problems:
- Hypertension: High blood pressure, a condition where the force of blood against the walls of the arteries is consistently too high, damaging the heart and vessels.
- Atherosclerosis: The buildup of fatty deposits on the walls of arteries, which can restrict blood flow and increase the risk of heart attacks and strokes.
- Peripheral Artery Disease: A condition where the arteries in the limbs become narrowed, leading to poor circulation and an increased risk of infections and gangrene.
Common Heart and Blood Vessel Pathologies to Study
Understanding the most prevalent diseases affecting the heart and blood vessels is essential for recognizing their symptoms, causes, and treatment options. These pathologies often result in severe health complications and require a detailed study of their mechanisms, risk factors, and management strategies.
Heart Diseases
The following conditions are commonly studied due to their impact on the heart’s function:
- Myocardial Infarction: Often referred to as a heart attack, this occurs when blood flow to part of the heart is blocked, leading to tissue damage.
- Congestive Heart Failure: A condition where the heart is unable to pump blood effectively, causing fluid retention and difficulty breathing.
- Valvular Heart Disease: Involves the malfunction of one or more heart valves, leading to improper blood flow and increased strain on the heart.
Vascular Disorders
Diseases that affect blood vessels can lead to significant circulation problems, including:
- Stroke: A blockage or rupture of blood vessels in the brain, leading to sudden loss of function in certain parts of the body.
- Peripheral Arterial Disease (PAD): A condition where the arteries in the limbs become narrowed or blocked, causing pain and increasing the risk of infection.
- Aneurysms: Abnormal bulges in the walls of arteries, which can rupture and lead to life-threatening internal bleeding.
Techniques for Measuring Heart Function
Evaluating the performance of the heart is crucial for diagnosing potential issues and monitoring the overall health of an individual. Various methods are employed to assess the efficiency of heart contractions, blood flow, and electrical activity, each providing unique insights into the organ’s functionality.
Electrocardiogram (ECG)
An ECG is one of the most common tools used to measure the electrical activity of the heart. By recording the heart’s electrical impulses, it helps detect irregular heartbeats, heart attacks, and other abnormalities.
Echocardiography
This non-invasive technique uses sound waves to create detailed images of the heart’s structure and function. It allows healthcare providers to observe the heart’s chambers, valves, and blood flow, offering insights into any potential structural issues or fluid buildup.
Stress Testing
Stress tests measure the heart’s response to physical activity. By monitoring heart rate, blood pressure, and ECG during exercise, doctors can assess the heart’s ability to handle increased demand and detect hidden conditions like coronary artery disease.
Cardiac Catheterization
In this invasive procedure, a catheter is inserted into the heart through a blood vessel to measure pressures within the heart and arteries. It is often used to diagnose blockages, heart valve issues, and other conditions that may not be visible through non-invasive methods.
Diagnostic Tests in Heart and Blood Vessel Medicine
Accurate diagnosis of conditions affecting the heart and blood vessels is essential for effective treatment and management. Various diagnostic tests are utilized to assess the structure, function, and overall health of these vital organs. These tests provide valuable insights into potential issues, allowing healthcare providers to tailor treatment plans accordingly.
Non-Invasive Diagnostic Methods

Non-invasive tests are commonly used to monitor heart health without the need for surgery or penetration. These methods are safe and can offer a quick overview of potential problems:
- Electrocardiogram (ECG): Measures the electrical activity of the heart to detect irregularities such as arrhythmias or previous heart attacks.
- Echocardiogram: Uses sound waves to create images of the heart’s structure and movement, allowing doctors to evaluate the function of the heart valves and chambers.
- Ultrasound Doppler: Assesses blood flow through the arteries and veins, helping detect blockages or irregularities in circulation.
Invasive Diagnostic Techniques
In some cases, more detailed information is required, and invasive tests may be necessary. These methods provide a more direct and thorough analysis of heart and vessel function:
- Cardiac Catheterization: Involves inserting a catheter into the heart to measure blood pressure and obtain detailed images of the arteries.
- Coronary Angiography: A type of catheterization used to visualize the inside of blood vessels in the heart to identify blockages or narrowing.
- Electrophysiology Study: A procedure to study the electrical pathways in the heart, often used to diagnose arrhythmias or assess the heart’s electrical conduction system.
Vascular Disorders and Their Impact
Conditions that affect the blood vessels can have a significant impact on overall health, influencing circulation and the delivery of oxygen and nutrients to various organs. These disorders can lead to a range of complications, from minor discomfort to life-threatening situations, depending on the severity and location of the issue. Understanding the types of vascular disorders is essential for preventing, diagnosing, and managing these conditions effectively.
Types of Vascular Disorders
Vascular issues can involve the arteries, veins, or lymphatic system. Some of the most common disorders include:
- Atherosclerosis: A condition where fatty deposits build up in the arteries, narrowing and hardening them, which can lead to reduced blood flow and increase the risk of heart attacks or strokes.
- Varicose Veins: Swollen and twisted veins that typically occur in the legs. They can cause pain, swelling, and discomfort, and in severe cases, lead to blood clots or ulcers.
- Deep Vein Thrombosis (DVT): The formation of a blood clot in a deep vein, often in the legs, which can break free and travel to the lungs, causing a pulmonary embolism.
- Peripheral Artery Disease (PAD): A condition where narrowed arteries reduce blood flow to the limbs, causing pain, weakness, and in severe cases, tissue death.
- Aneurysm: An abnormal bulging of a blood vessel wall, which can rupture and cause life-threatening internal bleeding.
Impact of Vascular Disorders
The impact of vascular diseases varies depending on the type and severity of the condition. Some of the common effects include:
- Impaired Circulation: Reduced blood flow can lead to symptoms such as fatigue, dizziness, or cold extremities, and in severe cases, it can cause organ dysfunction.
- Increased Risk of Stroke or Heart Attack: Conditions like atherosclerosis or blood clots significantly increase the likelihood of life-threatening events, such as a stroke or heart attack.
- Chronic Pain or Discomfort: Disorders like varicose veins or PAD can lead to chronic pain, swelling, and difficulty walking or performing everyday tasks.
- Wound Healing Issues: Poor circulation caused by vascular diseases can make it difficult for wounds to heal, increasing the risk of infection and other complications.
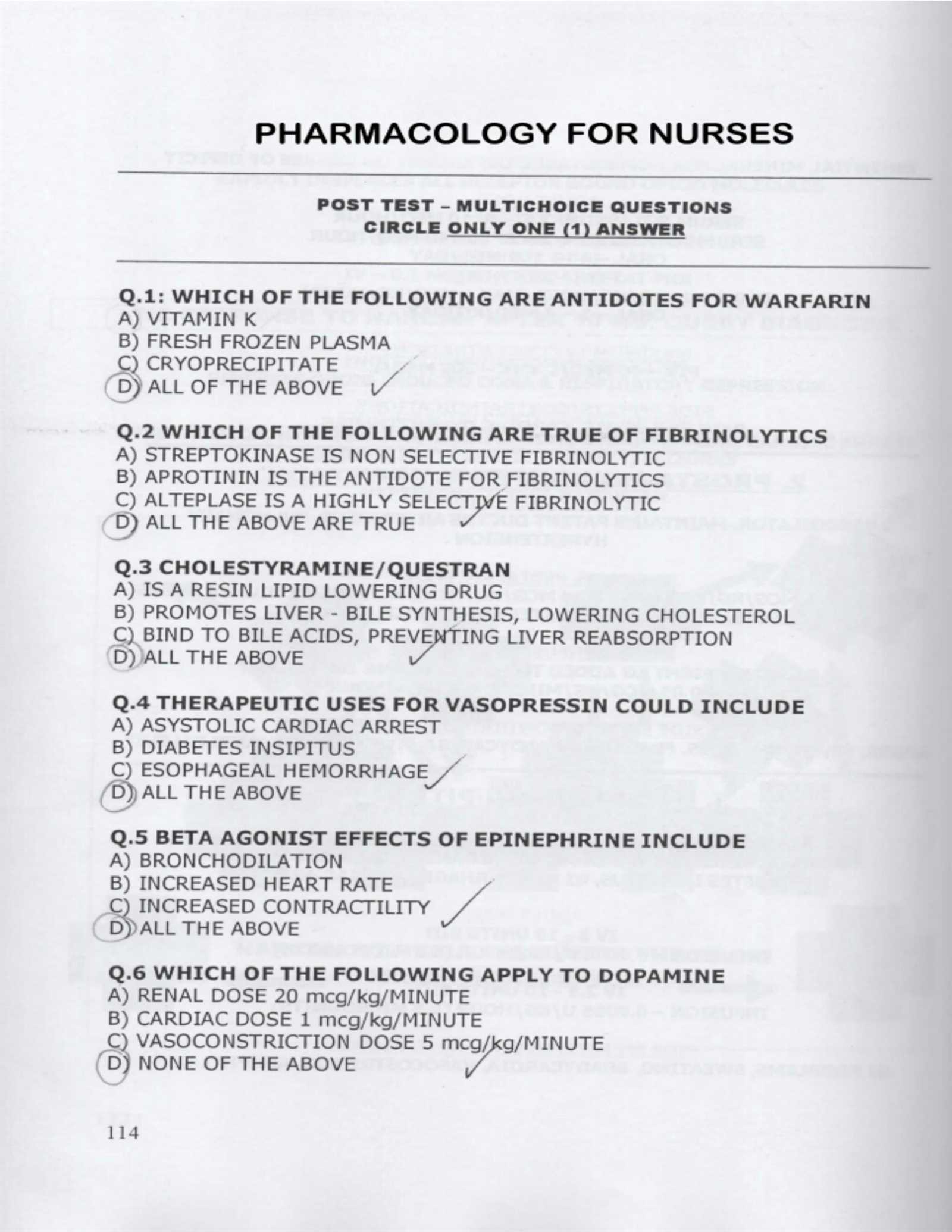
Cardiac Pharmacology for Exam Preparation
Understanding the role of medications in treating heart-related conditions is crucial for anyone studying heart health. Medications can have a direct effect on the function of the heart, influencing everything from blood pressure to heart rate and rhythm. This section will cover essential drugs, their mechanisms of action, and their clinical applications, all of which are important for mastering pharmacological concepts related to the heart.
Classes of Medications for Heart Conditions
Several classes of drugs are commonly prescribed to manage various heart conditions. These medications help regulate heart function, improve circulation, and prevent complications. The most important classes include:
- Beta-Blockers: These medications reduce heart rate and blood pressure by blocking the effects of adrenaline. They are often used in the treatment of hypertension, arrhythmias, and heart failure.
- ACE Inhibitors: Angiotensin-converting enzyme inhibitors relax blood vessels, reduce blood pressure, and improve heart function, particularly in patients with heart failure or after a heart attack.
- Diuretics: Often referred to as “water pills,” these drugs help reduce fluid buildup by increasing urine production, which is especially beneficial for patients with heart failure or high blood pressure.
- Calcium Channel Blockers: These drugs prevent calcium from entering the heart and blood vessel cells, leading to a decrease in heart rate and blood pressure. They are frequently used to treat hypertension, angina, and certain arrhythmias.
- Anticoagulants: These medications help prevent blood clots, reducing the risk of stroke and heart attack. They are commonly prescribed to patients with atrial fibrillation or those who have had previous heart attacks.
Pharmacokinetics and Monitoring
In addition to understanding the mechanisms of action, it is essential to know how the body absorbs, distributes, metabolizes, and excretes these medications. This is crucial for understanding dosing schedules, side effects, and potential interactions with other drugs:
- Absorption: The rate and extent to which a drug enters the bloodstream can impact its effectiveness, especially in patients with gastrointestinal issues.
- Metabolism: Many cardiac drugs are metabolized in the liver, which can affect drug levels and the likelihood of side effects, especially in older adults.
- Excretion: Drugs are often excreted through the kidneys. Impaired renal function can lead to drug accumulation, increasing the risk of toxicity.
- Monitoring: Regular monitoring of drug levels, kidney function, and electrolyte balance is essential to ensure that medications are working effectively and safely.
Managing Hypertension and Its Effects
High blood pressure is a common yet serious condition that can lead to various complications if not properly managed. Effective management is critical for reducing the risk of stroke, heart attack, kidney damage, and other serious health issues. This section explores the approaches to controlling blood pressure and the impacts of sustained high pressure on the body.
Effective Strategies for Controlling Blood Pressure
There are multiple methods for managing high blood pressure, ranging from lifestyle changes to medication. The goal is to lower blood pressure to within a healthy range and to maintain it over the long term. Key strategies include:
- Dietary Changes: A low-sodium, balanced diet rich in fruits, vegetables, and whole grains is essential for blood pressure control. The DASH (Dietary Approaches to Stop Hypertension) diet is frequently recommended.
- Physical Activity: Regular aerobic exercise, such as walking, swimming, or cycling, can help reduce blood pressure by improving heart health and circulation.
- Weight Management: Maintaining a healthy weight is crucial, as excess weight increases strain on the heart and contributes to high blood pressure.
- Stress Reduction: Chronic stress can elevate blood pressure. Relaxation techniques like meditation, yoga, and deep breathing can help manage stress.
- Medications: When lifestyle changes alone aren’t sufficient, antihypertensive medications may be prescribed to lower blood pressure effectively.
Potential Effects of Untreated High Blood Pressure
If left unmanaged, elevated blood pressure can cause significant damage to various organs. The long-term effects are often gradual but can have devastating consequences:
| Complication | Description |
|---|---|
| Heart Disease | High pressure forces the heart to work harder, increasing the risk of coronary artery disease, heart failure, and heart attacks. |
| Stroke | Increased pressure can damage blood vessels in the brain, raising the risk of a stroke. |
| Kidney Damage | Chronic high blood pressure can harm the kidneys, leading to kidney disease or even failure. |
| Vision Loss | Damage to the blood vessels in the eyes can lead to vision problems, including blindness. |
| Peripheral Artery Disease | High blood pressure can lead to narrowed arteries in the limbs, causing pain, numbness, or even amputation in severe cases. |
Early detection and consistent management of high blood pressure can significantly reduce the risk of these complications, enhancing overall health and well-being.
Heart Failure and Exam Strategies
Heart failure is a serious condition where the heart is unable to pump blood efficiently, leading to insufficient circulation throughout the body. Understanding the key concepts surrounding this condition is crucial for both diagnosis and treatment. This section discusses the fundamentals of heart failure and strategies to effectively assess the disease during a clinical evaluation.
Understanding the Key Aspects of Heart Failure
Heart failure can manifest in various forms, with the most common being left-sided, right-sided, and congestive heart failure. Each form has distinct symptoms and underlying causes. Early recognition of these signs is essential for proper intervention. Key elements to consider include:
- Symptoms: Fatigue, shortness of breath, swelling in the legs, and fluid retention are common symptoms.
- Causes: Conditions such as high blood pressure, coronary artery disease, and previous heart attacks can contribute to heart failure.
- Diagnosis: Proper diagnosis involves a combination of clinical examination, imaging tests like echocardiograms, and blood tests to measure biomarkers.
- Treatment: Management often includes medications, lifestyle changes, and in some cases, surgical interventions like heart transplants or device implants.
Approaching Heart Failure in Clinical Assessments
When assessing heart failure, it is important to take a comprehensive approach to evaluate the severity and potential causes. Key strategies for accurate evaluation include:
- Thorough Patient History: Identifying risk factors such as hypertension, diabetes, or a history of heart disease is vital for understanding the patient’s condition.
- Physical Examination: Listening for abnormal heart sounds, checking for fluid retention, and measuring blood pressure can provide important clues.
- Diagnostic Testing: Using tests like echocardiograms, chest X-rays, and blood tests (such as BNP levels) helps confirm the diagnosis and assess heart function.
- Continuous Monitoring: Monitoring the patient’s response to treatments and tracking their symptoms over time is essential for adjusting care plans.
Successful management of heart failure depends on accurate diagnosis and timely intervention. By focusing on these key strategies, healthcare professionals can improve patient outcomes and prevent further complications.
Examining the Atherosclerosis Process
Atherosclerosis is a chronic condition that involves the gradual buildup of plaque within the arteries, leading to narrowing and stiffening of the blood vessels. Over time, this can restrict blood flow and increase the risk of serious health issues, such as heart attacks, strokes, and peripheral artery disease. Understanding the stages of plaque formation, its causes, and the effects on the body is essential for effective prevention and treatment strategies.
The process begins with the damage to the inner walls of blood vessels, often due to factors such as high blood pressure, high cholesterol levels, or smoking. This damage triggers an inflammatory response, where white blood cells and other substances gather at the site. As time progresses, fatty deposits, cellular waste, and cholesterol accumulate, forming plaque. The buildup can eventually cause the artery to harden, reducing its elasticity and obstructing blood flow.
Several factors can accelerate the progression of atherosclerosis. These include poor diet, lack of physical activity, obesity, and genetic predispositions. Identifying and managing these risk factors is crucial in slowing down or even halting the disease progression.
As atherosclerosis progresses, it can lead to complications such as:
- Coronary artery disease: Narrowing of the arteries supplying the heart muscle, leading to chest pain (angina) or heart attacks.
- Stroke: Reduced blood flow to the brain, increasing the risk of a stroke.
- Peripheral artery disease: Reduced circulation to the limbs, often resulting in pain and reduced mobility.
Recognizing the signs of advanced atherosclerosis and taking preventive measures such as lifestyle changes, medication, and, in some cases, surgical interventions, can help manage the condition and reduce its life-threatening complications.
Arrhythmias and Their Clinical Significance
Irregularities in the heart’s rhythm are common occurrences that can significantly impact a person’s health. These irregularities, known as arrhythmias, involve the heart beating too fast, too slow, or in an erratic pattern. While some arrhythmias are harmless and may not require treatment, others can be life-threatening and require immediate medical intervention. Understanding the different types of arrhythmias, their causes, and the potential complications is crucial for effective diagnosis and management.
The heart relies on electrical signals to maintain a consistent rhythm. When these signals are disrupted, the heart’s normal rhythm is affected, leading to an arrhythmia. This disruption can occur in different parts of the heart, causing a variety of symptoms and potential complications. The clinical significance of arrhythmias lies in their ability to impair the heart’s ability to pump blood efficiently, which can result in poor circulation, organ dysfunction, and increased risk of stroke or sudden cardiac arrest.
Common Types of Arrhythmias
There are several types of arrhythmias, each with distinct characteristics and clinical implications. Some of the most common include:
- Atrial fibrillation (AFib): A rapid, irregular heartbeat originating in the atria, which can lead to blood clots, stroke, and heart failure if untreated.
- Bradycardia: An abnormally slow heart rate, which may lead to dizziness, fainting, or even cardiac arrest in severe cases.
- Tachycardia: An unusually fast heart rate that can lead to fatigue, shortness of breath, and an increased risk of heart failure or stroke.
- Ventricular fibrillation: A life-threatening arrhythmia in which the ventricles quiver instead of contracting properly, resulting in a loss of effective blood circulation and requiring immediate resuscitation.
Clinical Diagnosis and Treatment
The diagnosis of arrhythmias typically involves a combination of physical examination, patient history, and diagnostic tests such as an electrocardiogram (ECG). Once identified, treatment options vary depending on the type and severity of the arrhythmia. These may include medications, lifestyle changes, electrical cardioversion, or even implantation of a pacemaker or defibrillator for more severe cases.
Ultimately, early detection and appropriate management of arrhythmias are crucial for preventing complications such as stroke, heart failure, or sudden cardiac arrest. Regular monitoring and adherence to treatment plans can significantly improve the quality of life for individuals with arrhythmias.
Prevention and Treatment of Cardiovascular Diseases
Chronic conditions related to the heart and blood vessels can lead to severe complications, including stroke, heart failure, and other life-threatening events. Understanding how to prevent and manage these conditions is essential for maintaining long-term health. Prevention strategies focus on reducing risk factors, while treatment options aim to address existing problems and improve quality of life. Early detection, lifestyle adjustments, and appropriate medical interventions play key roles in both prevention and management.
Preventive Measures for Heart Health
Adopting a healthy lifestyle can significantly reduce the risk of developing heart-related diseases. Key preventive strategies include:
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding excessive salt, sugar, and unhealthy fats.
- Regular Exercise: Engaging in physical activity, such as walking, swimming, or cycling, for at least 150 minutes per week to improve heart function.
- Avoiding Smoking: Quitting smoking reduces the risk of plaque buildup in blood vessels and improves overall heart health.
- Moderating Alcohol Consumption: Limiting alcohol intake to recommended levels helps prevent high blood pressure and reduces the risk of heart disease.
- Stress Management: Practicing relaxation techniques such as yoga, meditation, or deep breathing to manage stress and protect heart health.
Treatment Options for Existing Heart Conditions
When heart or blood vessel problems are diagnosed, treatment options vary depending on the specific condition. Below are common treatment strategies:
| Treatment | Description |
|---|---|
| Medications | Drugs such as statins, beta-blockers, and ACE inhibitors are used to control blood pressure, cholesterol levels, and prevent blood clots. |
| Surgical Interventions | In cases of severe arterial blockage or heart valve issues, surgery may be required, including coronary artery bypass grafting (CABG) or valve repair/replacement. |
| Minimally Invasive Procedures | Techniques like angioplasty or stent placement can help open blocked arteries without the need for large incisions. |
| Pacemaker/Defibrillator | Implantation of devices to regulate heart rhythm in patients with arrhythmias or heart failure. |
| Rehabilitation Programs | Structured exercise and education programs to help individuals recover from heart events and improve overall cardiovascular health. |
Effective treatment often involves a combination of approaches tailored to the individual’s condition, emphasizing both medication and lifestyle changes. Ongoing monitoring and support are crucial to ensuring optimal management and preventing further complications.