As healthcare professionals or students pursuing a career in respiratory care, mastering the fundamental concepts related to chronic lung diseases is crucial. Thorough knowledge of key topics and conditions plays an essential role in delivering effective patient care and achieving success in assessments.
To excel in this area, it’s important to understand the disease mechanisms, common treatment protocols, and diagnostic tools used to evaluate lung function. By focusing on real-life scenarios and clinical application, you can enhance your ability to recall and apply information effectively.
In this guide, we will explore various aspects of respiratory health, offering insights into typical evaluation topics, the most commonly asked points, and the clinical reasoning behind effective management strategies. With the right approach, you’ll be well-equipped to tackle any challenge that comes your way in this field.
Key Concepts in Respiratory Health Assessment
When evaluating chronic lung conditions, it’s vital to grasp the underlying principles that guide clinical assessments. These concepts help healthcare professionals determine the severity of the disease, identify risk factors, and implement the most effective treatment plans. A strong understanding of these principles allows for better decision-making and improves patient outcomes.
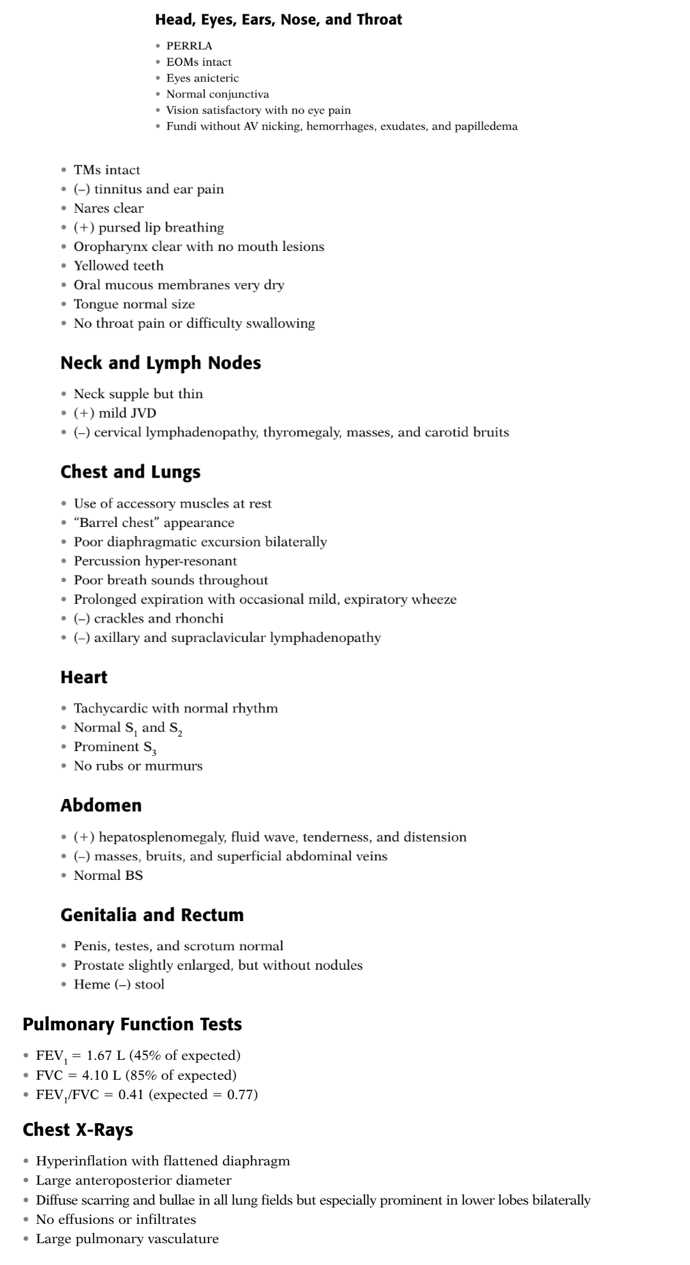
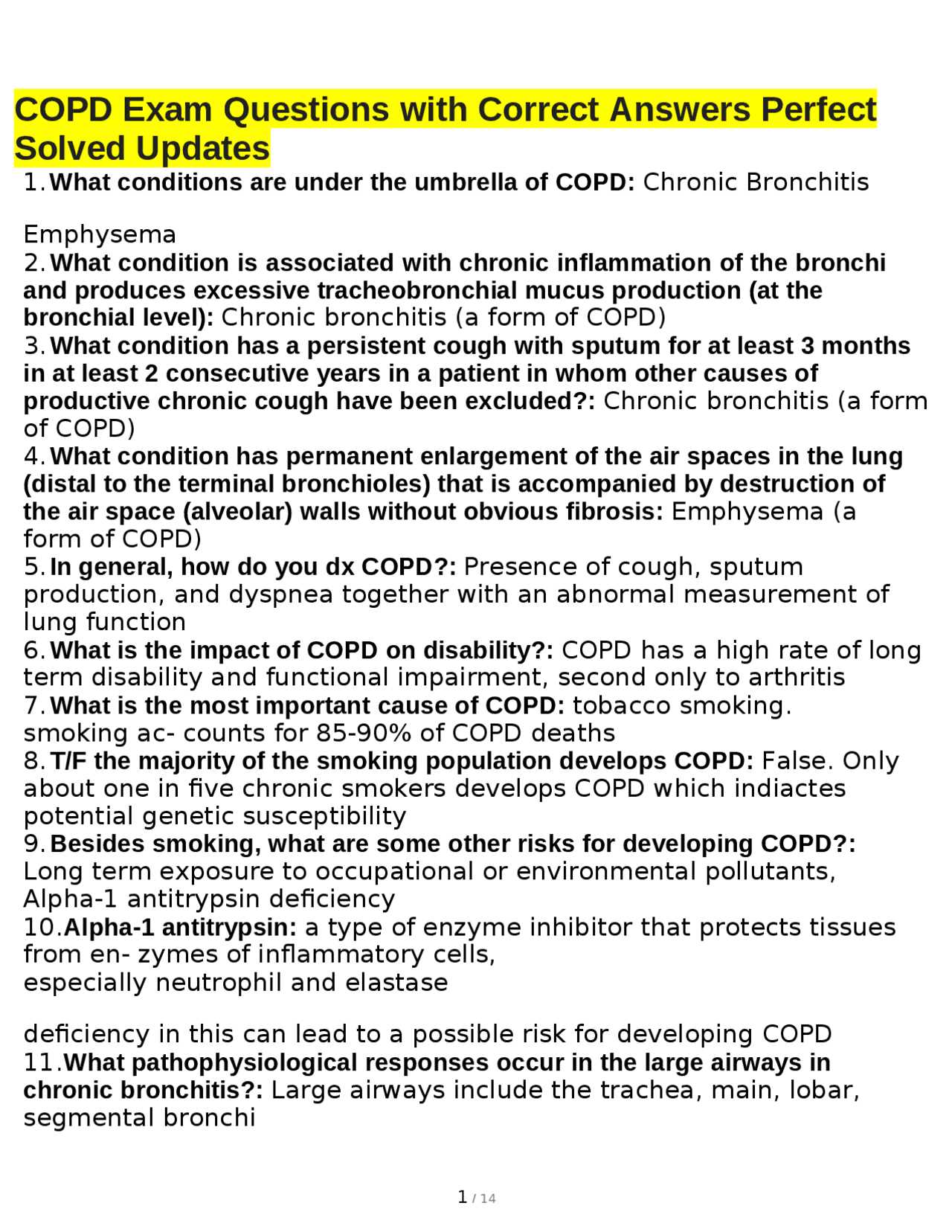
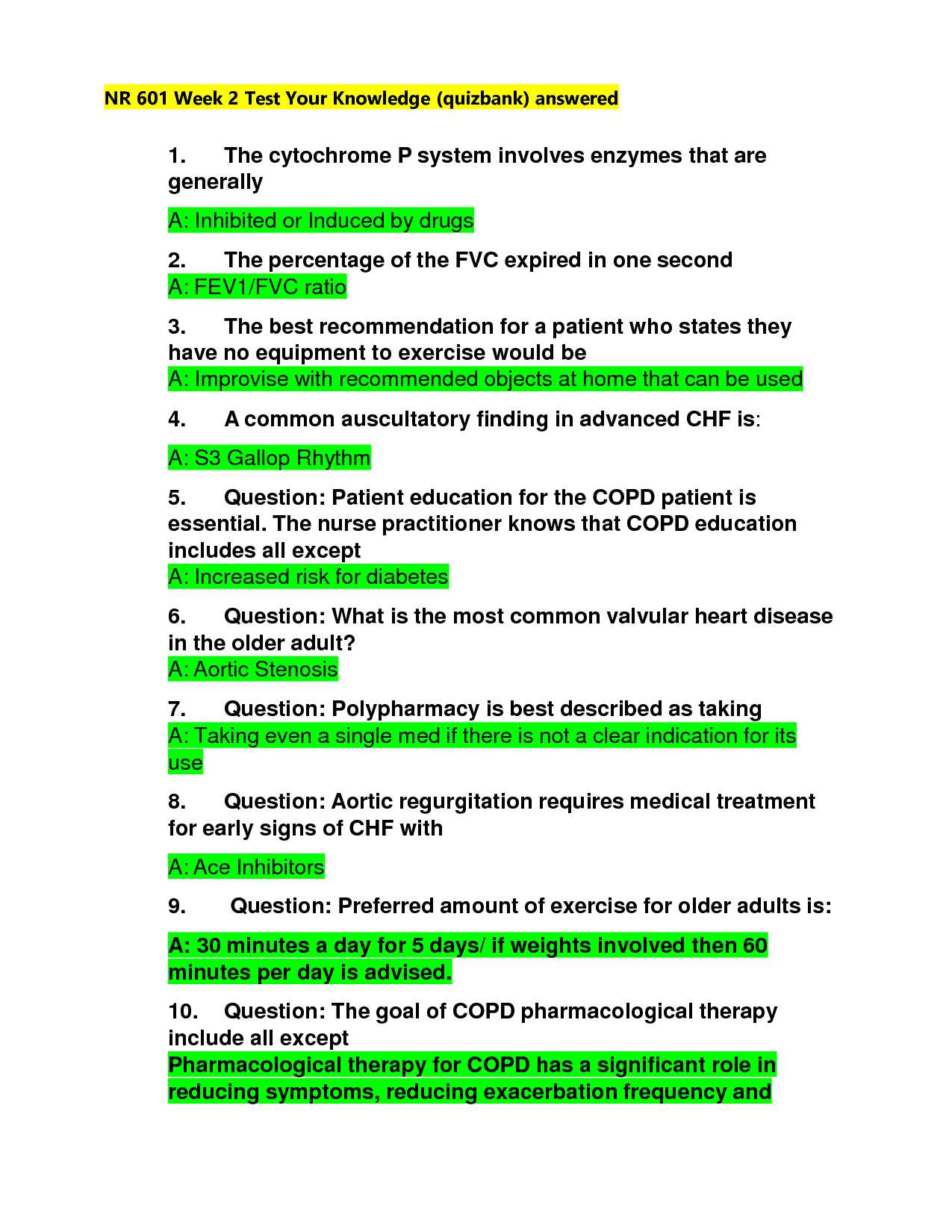
One of the core elements in this field is understanding lung function. Techniques such as spirometry are commonly used to measure airflow and assess how well the lungs are performing. The results of these tests provide essential insights into the degree of airflow limitation, which is a primary indicator of respiratory health.
Another important factor is recognizing the symptoms associated with chronic lung diseases. Symptoms like shortness of breath, chronic cough, and mucus production are often key signs of disease progression. Identifying these symptoms early can help in staging the condition and tailoring personalized management strategies.
It’s also crucial to consider the role of comorbidities in respiratory health. Conditions such as cardiovascular diseases, diabetes, and osteoporosis can complicate the management of lung diseases. A holistic approach that takes these additional factors into account ensures more comprehensive care for patients.
Understanding Respiratory Symptoms and Diagnosis
Accurately identifying the symptoms of chronic lung diseases is crucial for early detection and proper management. These conditions often develop gradually, and the early signs may be subtle, making it important to recognize them before they worsen. A thorough understanding of common symptoms can help healthcare professionals make informed decisions about patient care and treatment strategies.
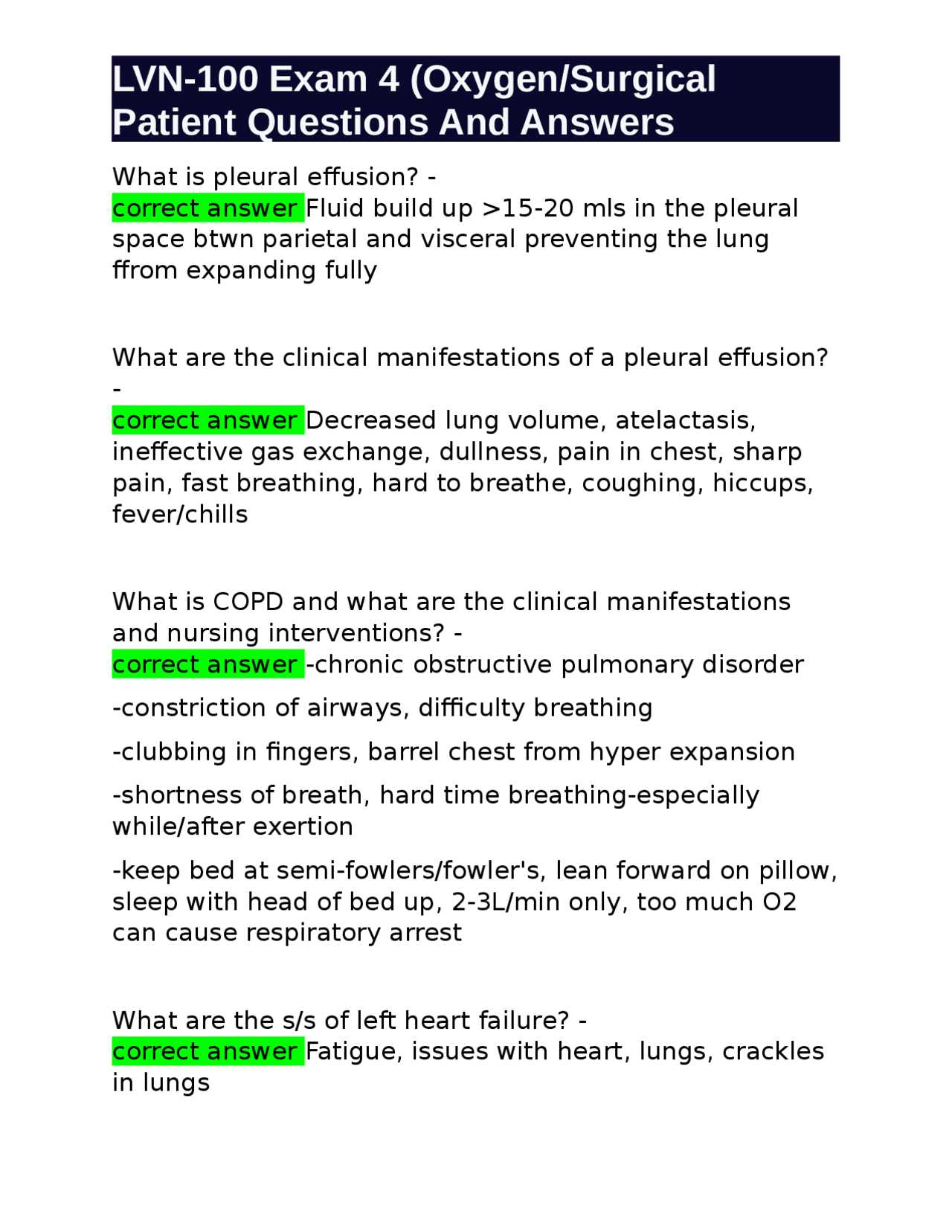
Typical symptoms of chronic lung diseases include persistent coughing, wheezing, shortness of breath, and frequent respiratory infections. These signs are often indicative of long-term damage to the airways and lung tissue. Patients may also experience difficulty breathing, particularly during physical activity, as the condition progresses.
Diagnosing such conditions involves a combination of clinical evaluations and diagnostic tests. Spirometry, a key diagnostic tool, measures how much air a person can exhale and how quickly. This test helps in determining the severity of airflow limitation and the overall lung function. Imaging studies, such as chest X-rays or CT scans, may also be used to assess the extent of lung damage.
Common Treatment Strategies for Chronic Respiratory Conditions
Managing chronic lung diseases requires a multifaceted approach that aims to reduce symptoms, improve quality of life, and prevent further complications. Treatment plans are tailored to the individual needs of patients, based on the severity of the condition, underlying health factors, and lifestyle considerations. Effective management involves a combination of medications, lifestyle changes, and supportive therapies.
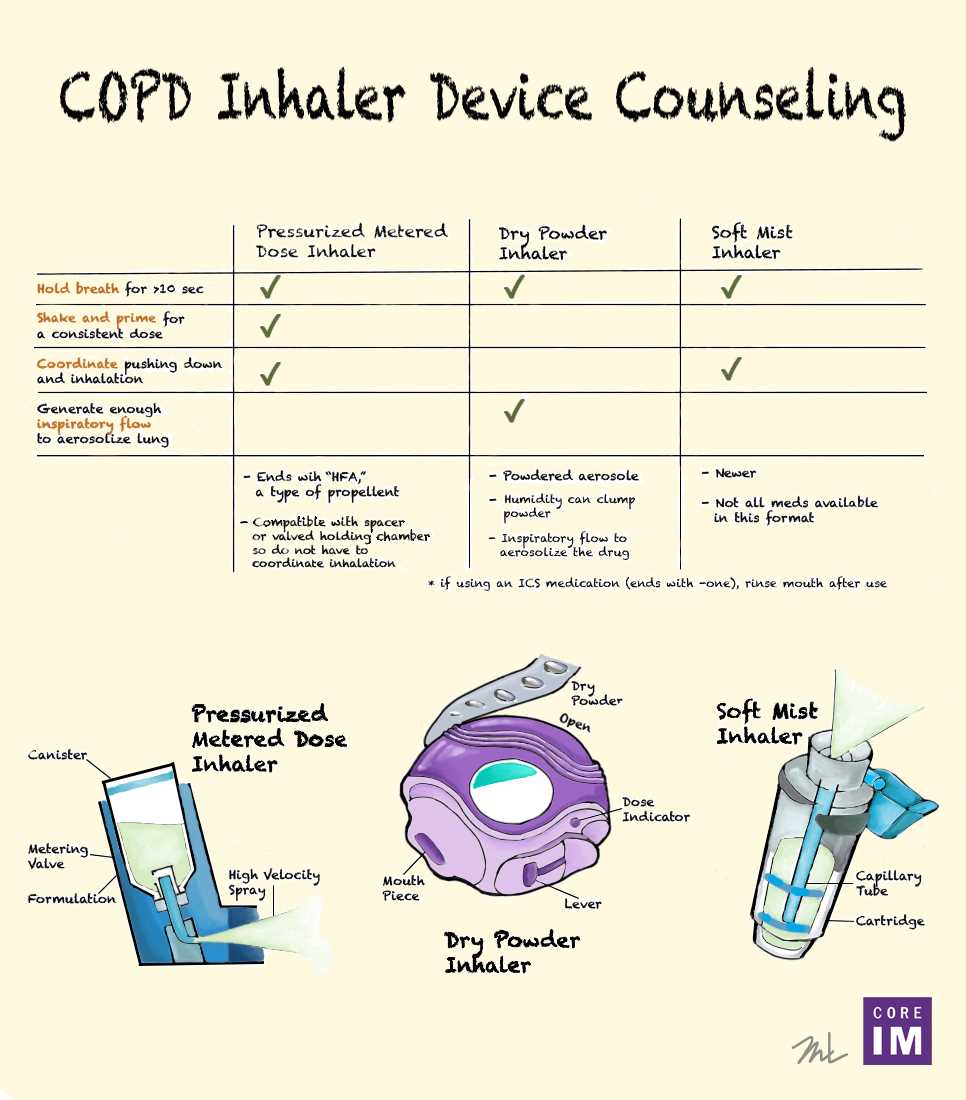
One of the primary treatments for managing chronic lung conditions is the use of inhalers containing bronchodilators and corticosteroids. Bronchodilators help relax the muscles around the airways, making it easier to breathe, while corticosteroids reduce inflammation within the lungs. In some cases, combination inhalers that contain both medications are prescribed for enhanced efficacy.
Oxygen therapy is another important treatment, particularly for patients with advanced stages of respiratory disease. This therapy helps to maintain adequate oxygen levels in the blood, improving overall respiratory function. Pulmonary rehabilitation, which includes physical exercises and breathing techniques, also plays a key role in improving endurance and reducing symptoms.
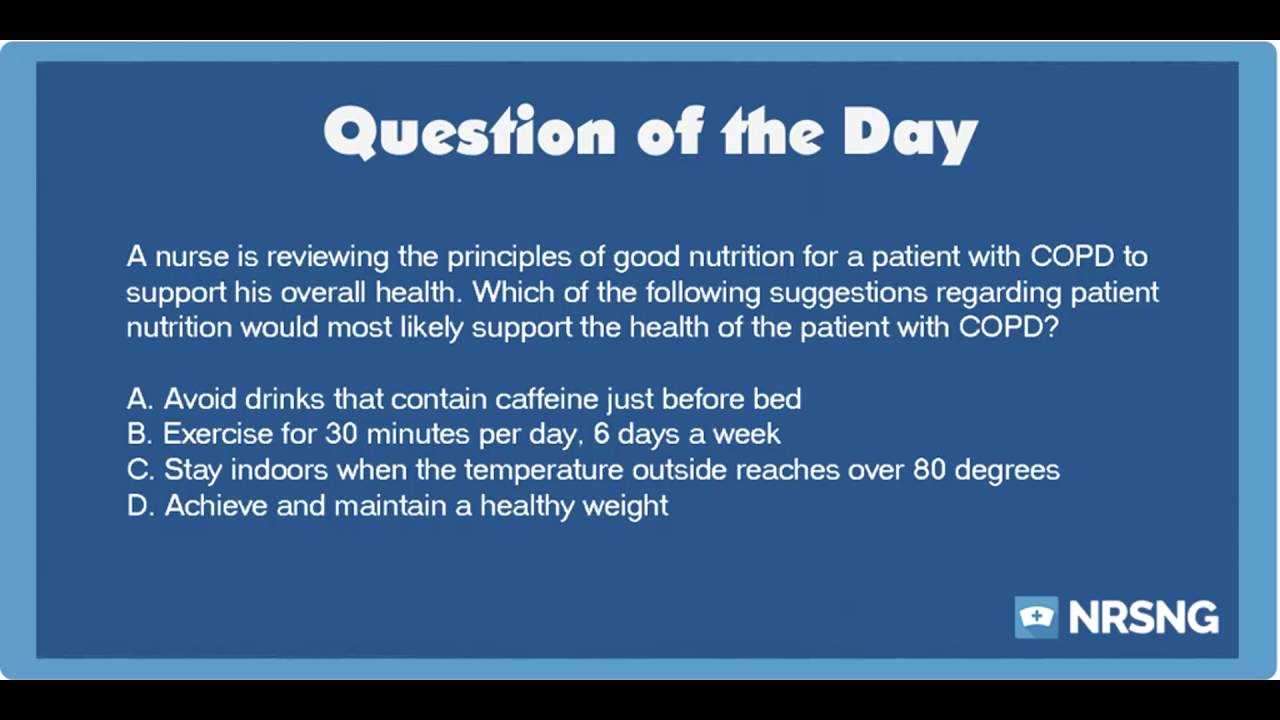
In addition to pharmacological treatments, lifestyle modifications are essential. Smoking cessation is the most important step in preventing further lung damage, as smoking accelerates the progression of respiratory conditions. Maintaining a healthy diet, staying active, and avoiding environmental irritants such as air pollution also contribute to better lung health and disease management.
Essential Management Considerations for Chronic Respiratory Conditions
Effective management of chronic lung diseases requires addressing a variety of factors that can influence disease progression, symptom control, and overall patient well-being. By asking the right questions, healthcare providers can better tailor treatment plans and ensure that patients receive the most appropriate care. These key considerations help ensure optimal outcomes and a personalized approach to managing the condition.
- What are the patient’s main symptoms? Understanding the severity of symptoms, such as breathlessness, coughing, or mucus production, is crucial in determining the best course of action for treatment.
- How is the patient’s lung function? Regular monitoring of lung function through tests like spirometry helps assess the progression of the disease and the effectiveness of the prescribed therapies.
- What medications are being used? Identifying the appropriate medications, including bronchodilators and anti-inflammatory drugs, is essential to control symptoms and improve lung function.
- Is there a smoking history? Smoking cessation is a critical part of treatment. Understanding the patient’s smoking history helps in developing strategies to stop smoking and prevent further lung damage.
- What comorbidities are present? Chronic diseases such as heart disease or diabetes can complicate treatment. Identifying these conditions ensures comprehensive care and reduces complications.
- What is the patient’s overall quality of life? Assessing how the condition affects daily activities, mental health, and social interactions helps in providing holistic care and setting realistic treatment goals.
- Has the patient received pulmonary rehabilitation? Pulmonary rehab programs can significantly improve physical endurance and lung capacity, especially in advanced stages of the condition.
By addressing these key questions, healthcare providers can develop a more comprehensive management plan that aligns with the patient’s needs and helps to improve their long-term health outcomes. Regular follow-ups and adjustments to the treatment plan are essential in maintaining optimal care as the disease progresses.
Key Medications for Chronic Respiratory Conditions
Managing chronic lung diseases effectively relies heavily on the proper use of medications. These treatments help alleviate symptoms, improve lung function, and prevent exacerbations. Understanding the different classes of medications and how they work is crucial for both healthcare providers and patients to achieve the best possible outcomes.
- Bronchodilators – These medications help relax the muscles around the airways, making it easier to breathe. There are two main types:
- SABA (Short-Acting Beta Agonists) – Provide quick relief during flare-ups by opening the airways rapidly. Common examples include albuterol and levalbuterol.
- LAMA (Long-Acting Muscarinic Antagonists) – Help to control symptoms over a longer period by relaxing the airway muscles. Examples include tiotropium and umeclidinium.
- Corticosteroids – These medications reduce inflammation in the airways, improving breathing and reducing the frequency of flare-ups. They are typically used in combination with bronchodilators for better control of symptoms. Common medications include fluticasone and budesonide.
- Combination Inhalers – These inhalers combine both bronchodilators and corticosteroids in one device, making it easier for patients to manage their treatment regimen. Examples include Symbicort (budesonide/formoterol) and Advair (fluticasone/salmeterol).
- Phosphodiesterase-4 Inhibitors – These drugs reduce inflammation and relax the airways. They are typically prescribed for patients with severe disease. Roflumilast is a commonly used medication in this class.
- Oxygen Therapy – For patients with severe lung damage, supplemental oxygen can help ensure that the body receives enough oxygen, especially during physical activities or sleep.
Each medication serves a specific purpose in managing chronic respiratory diseases, and the choice of treatment depends on the patient’s symptoms, disease severity, and overall health. It is important for patients to follow their prescribed treatment plan and consult with their healthcare providers regularly to ensure the medications are working effectively.
Practical Study Tips for Respiratory Health Assessments
Preparing for assessments related to chronic respiratory conditions requires a focused and strategic approach. Mastering the core concepts and practicing critical thinking will help you approach clinical scenarios with confidence. Below are some effective study tips that will improve retention and performance during your preparation.
Focus on Key Concepts and Pathophysiology
Understanding the underlying mechanisms of chronic lung diseases is crucial. Concentrate on how the disease affects lung function, the body’s response to treatment, and the progression of symptoms. Review the basics of lung anatomy, airflow limitation, and the role of inflammation in disease development. This foundational knowledge will help you apply clinical reasoning to various case scenarios.
Practice with Case Studies and Simulations
Case studies are an excellent way to apply theoretical knowledge to real-world situations. They challenge you to think critically about diagnosis, treatment options, and patient management. Using simulation exercises can help you improve your decision-making skills and familiarize yourself with the types of scenarios you may encounter. These exercises also allow you to practice prioritizing patient care based on severity and comorbidities.
By focusing on these study techniques and practicing regularly, you’ll be well-prepared to tackle any challenge related to respiratory health. Consistent practice and a deep understanding of the material will not only enhance your knowledge but also improve your clinical judgment.
Breathing Techniques for Chronic Respiratory Patients
Proper breathing techniques play a crucial role in managing chronic lung conditions. These methods can help patients control their breathlessness, reduce anxiety, and improve oxygen intake, ultimately enhancing their overall quality of life. By learning and practicing these techniques, patients can better manage symptoms and improve their ability to engage in daily activities.
| Technique | Description | Benefits |
|---|---|---|
| Diaphragmatic Breathing | This technique involves breathing deeply using the diaphragm, allowing the lungs to expand fully. It helps to slow down the breath and improve lung capacity. | Reduces shortness of breath, enhances lung efficiency, and promotes relaxation. |
| Pursed Lip Breathing | By inhaling through the nose and exhaling slowly through pursed lips, this technique helps keep the airways open for longer, allowing for easier exhalation. | Improves airflow, reduces the feeling of breathlessness, and stabilizes breathing during physical exertion. |
| Controlled Coughing | Controlled coughing helps clear mucus from the airways. Patients should take a deep breath, hold it, and then cough gently. | Clears the airways, reduces congestion, and prevents infections by expelling mucus effectively. |
| Box Breathing | Involves inhaling for four counts, holding the breath for four counts, exhaling for four counts, and holding again for four counts. | Promotes relaxation, reduces stress, and can help manage anxiety during episodes of breathlessness. |
Incorporating these techniques into daily routines can lead to better respiratory control and overall well-being. It’s important for patients to consult with healthcare professionals to learn these methods and practice them correctly, ensuring maximum benefit.
Understanding Respiratory Condition Complications
As chronic lung diseases progress, they can lead to a range of complications that significantly impact the patient’s health and quality of life. These complications often arise due to the ongoing strain on the respiratory system and the body’s response to impaired lung function. Recognizing and managing these issues is essential for improving patient outcomes and preventing further health deterioration.
Common Complications Associated with Chronic Respiratory Conditions
- Frequent Respiratory Infections: Patients with chronic lung diseases are more susceptible to respiratory infections such as pneumonia and bronchitis, which can worsen symptoms and lead to severe flare-ups.
- Heart Problems: Chronic lung conditions can increase the risk of cardiovascular diseases, including heart failure, due to the strain on the heart as it works harder to deliver oxygen throughout the body.
- Oxygen Deficiency: In advanced stages, inadequate oxygen levels can lead to hypoxemia, which affects other organs and systems, leading to organ damage.
- Pulmonary Hypertension: High blood pressure in the arteries of the lungs can develop as a result of prolonged oxygen deprivation, contributing to further strain on the heart.
- Sleep Apnea: The interruption of normal breathing during sleep is common in individuals with chronic lung conditions, leading to poor sleep quality and daytime fatigue.
Managing Complications to Improve Outcomes
Effective management of complications involves close monitoring and appropriate interventions. Key strategies include:
- Vaccinations: Keeping up with flu and pneumonia vaccinations helps prevent infections that can lead to more severe health problems.
- Oxygen Therapy: For those with low oxygen levels, supplemental oxygen can improve oxygen saturation and reduce strain on the heart and other organs.
- Cardiovascular Monitoring: Regular heart check-ups and managing comorbidities such as high blood pressure can help reduce the risk of heart complications.
- Inhaled Medications: Proper use of inhalers and other prescribed treatments can help prevent flare-ups and manage symptoms, minimizing the risk of complications.
- Diet and Exercise: A healthy lifestyle with proper nutrition and regular physical activity can help strengthen the respiratory and cardiovascular systems, improving overall health.
Recognizing these complications early and implementing appropriate management strategies is critical to preventing further deterioration and improving the quality of life for patients living with chronic respiratory conditions.
Questions on Respiratory Condition Risk Factors
Understanding the risk factors associated with chronic lung diseases is essential for both prevention and early detection. These factors contribute to the development and progression of the condition, and recognizing them can lead to better management strategies. Identifying high-risk individuals allows healthcare professionals to provide targeted interventions and reduce the overall burden of the disease.
Key Risk Factors for Chronic Lung Diseases
| Risk Factor | Description | Impact |
|---|---|---|
| Smoking | Long-term smoking is the most significant risk factor, as it damages lung tissue and causes inflammation in the airways. | Increases the likelihood of developing chronic airflow limitations and worsens existing symptoms. |
| Exposure to Air Pollution | Long-term exposure to outdoor and indoor air pollution, such as fumes and dust, can irritate the lungs and contribute to respiratory problems. | Increases the risk of developing chronic respiratory diseases and exacerbates existing conditions. |
| Genetics | Some individuals inherit genetic conditions, such as alpha-1 antitrypsin deficiency, that predispose them to lung damage. | Increases vulnerability to lung tissue destruction and earlier onset of disease symptoms. |
| Occupational Hazards | Occupational exposure to harmful substances like chemicals, dust, and fumes can lead to lung damage over time. | Increases the risk of respiratory disease in workers exposed to hazardous environments. |
| Age | As individuals age, lung function naturally declines, making older adults more susceptible to developing chronic lung diseases. | Age-related decline in lung capacity and function contributes to the increased incidence of chronic respiratory conditions in the elderly. |
How to Mitigate These Risks
While some risk factors, such as genetics and age, are unavoidable, many can be mitigated through lifestyle changes and preventive measures. The most effective strategies include:
- Quitting Smoking: Ceasing smoking can significantly reduce the risk of developing chronic lung conditions and help slow disease progression.
- Reducing Exposure to Pollutants: Minimizing exposure to harmful chemicals and pollutants, both at work and at home, can protect lung health.
- Regular Health Screenings: Early detection through regular check-ups allows for timely intervention and better management of risk factors.
- Improving Air Quality: Using air purifiers and avoiding areas with high pollution levels can reduce the burden on the lungs.
By addressing these risk factors, individuals can greatly reduce their chances of developing chronic lung diseases and manage existing conditions more effectively.
Examining Respiratory Disease Pathophysiology Basics
Understanding the underlying mechanisms of chronic lung disorders is crucial for effective treatment and management. The pathophysiology of these conditions involves complex changes in lung tissue and airways that impair normal breathing. Recognizing these processes allows healthcare professionals to target specific areas of dysfunction and improve patient outcomes.
The primary cause of lung dysfunction in chronic respiratory diseases is the gradual damage to the lung tissue and the narrowing of the airways. Over time, this damage leads to reduced airflow and inefficient gas exchange, which in turn causes the hallmark symptoms of chronic breathlessness and reduced exercise capacity. The processes involved are often triggered by long-term exposure to harmful environmental factors such as smoking and pollutants.
| Pathophysiological Change | Description | Effect on Breathing |
|---|---|---|
| Airway Inflammation | Chronic irritation and inflammation of the airways lead to swelling, increased mucus production, and narrowing of the air passages. | Causes difficulty in airflow, leading to wheezing, shortness of breath, and coughing. |
| Loss of Elasticity | The lung tissue loses its natural elasticity, which hampers the lungs’ ability to expand and contract efficiently. | Results in difficulty exhaling and trapping air in the lungs, reducing oxygen intake and increasing carbon dioxide levels. |
| Alveolar Destruction | Damage to the alveoli (air sacs) impairs the gas exchange process, as the walls of the alveoli become weakened or destroyed. | Leads to reduced oxygen absorption and impaired carbon dioxide removal, causing low blood oxygen levels. |
| Increased Airway Resistance | Swelling and mucus build-up in the smaller airways increase resistance to airflow, making it harder to breathe. | Increases work of breathing, leading to fatigue, decreased activity tolerance, and a feeling of tightness in the chest. |
The pathophysiological changes described above are interrelated and contribute to the progressive nature of these conditions. Over time, as these processes worsen, patients may experience exacerbations, or periods of rapid symptom deterioration, requiring more intensive treatment.
By understanding these basic mechanisms, healthcare providers can offer better targeted therapies, such as bronchodilators, corticosteroids, and pulmonary rehabilitation, to manage symptoms and slow disease progression. Early intervention is key to improving quality of life and reducing the impact of the disease on daily activities.
Effective Respiratory Rehabilitation Programs
Rehabilitation programs play a crucial role in improving the quality of life for individuals living with chronic lung conditions. These structured programs are designed to enhance physical endurance, teach self-management strategies, and reduce the frequency of exacerbations. By addressing both the physical and emotional aspects of lung disease, rehabilitation efforts can significantly improve a patient’s overall well-being.
A comprehensive rehabilitation program typically includes a combination of exercise, education, and support, all aimed at helping individuals manage their condition more effectively. The goal is to strengthen the respiratory muscles, increase stamina, and promote long-term self-care. These programs are personalized to meet the specific needs of each patient, considering factors like disease severity and individual limitations.
- Exercise Training: Tailored physical activity routines help improve lung function, increase stamina, and reduce shortness of breath.
- Breathing Techniques: Patients are taught specialized breathing exercises to reduce the work of breathing and manage symptoms more effectively.
- Patient Education: Education sessions focus on disease management, symptom monitoring, and proper medication use.
- Psychosocial Support: Emotional and psychological support is provided to help patients cope with the challenges of living with a chronic condition.
- Nutrition Counseling: Healthy eating habits and weight management strategies are introduced to support overall health and reduce inflammation.
Through regular participation in rehabilitation programs, patients are not only able to manage their symptoms better but also gain a sense of control over their health. Many programs also offer guidance on lifestyle changes, including smoking cessation and avoiding environmental triggers, which are crucial for long-term disease management.
Ultimately, these rehabilitation programs aim to provide patients with the tools they need to lead an active, fulfilling life despite the limitations imposed by their respiratory condition. The goal is to minimize hospital visits and exacerbations, allowing individuals to remain as independent and active as possible.
Diagnostic Procedures for Respiratory Disorders Explained
Accurate diagnosis is essential for determining the appropriate treatment plan for individuals with chronic lung diseases. A variety of diagnostic tests and procedures are used to assess lung function, identify underlying conditions, and rule out other potential causes of respiratory symptoms. Understanding these diagnostic tools is key to ensuring early detection and effective management.
The diagnostic process typically begins with a thorough medical history review and physical examination, followed by specific tests designed to measure lung capacity, oxygen levels, and airflow. These tests help healthcare providers evaluate the severity of the condition and tailor treatment options to the individual’s needs.
- Pulmonary Function Tests (PFTs): These tests measure how much air the lungs can hold and how efficiently air is moved in and out. They include spirometry, which is often the first test conducted to assess lung function.
- Chest X-Ray: A chest X-ray helps identify structural changes in the lungs, such as hyperinflation or signs of lung infections, that may indicate chronic lung conditions.
- CT Scan: A high-resolution computed tomography (CT) scan provides detailed images of the lungs, helping detect emphysema, airway thickening, and other abnormalities that might not be visible on a regular X-ray.
- Arterial Blood Gas (ABG) Test: This test measures the levels of oxygen and carbon dioxide in the blood, helping to assess how well the lungs are exchanging gases and whether the patient needs supplemental oxygen.
- Oximetry: Pulse oximetry is a non-invasive test that measures blood oxygen levels using a small sensor attached to the fingertip. It provides quick feedback on oxygenation, particularly during physical activity or at rest.
- Exhaled Nitric Oxide Test: This test measures the amount of nitric oxide in the exhaled air, which can help identify inflammation in the airways and provide insight into disease severity.
Each of these tests provides valuable information that helps healthcare providers create a personalized treatment plan, targeting the areas most affected by the disease. While some of these procedures are conducted in a clinical setting, others may require follow-up assessments or ongoing monitoring to track changes in lung function over time.
By combining the results of these diagnostic tests with a patient’s symptoms and medical history, healthcare providers can accurately diagnose chronic respiratory diseases, determine their severity, and initiate the most appropriate treatment interventions.
Importance of Spirometry in Respiratory Health
Spirometry is one of the most valuable diagnostic tools used to assess lung function, playing a crucial role in evaluating various chronic respiratory conditions. It is a simple, non-invasive procedure that measures how much air a person can inhale and exhale, as well as how quickly the air moves in and out of the lungs. This test is essential for both diagnosing lung diseases and monitoring their progression over time.
Why Spirometry is Essential
Spirometry helps healthcare providers determine the severity of airflow limitation, which is a key factor in diagnosing chronic lung conditions. By measuring forced expiratory volume (FEV1) and forced vital capacity (FVC), spirometry gives a clear picture of lung function, allowing doctors to distinguish between different types of respiratory disorders. These measurements are crucial for both early detection and ongoing management.
Key Benefits of Spirometry
- Early Diagnosis: It enables early detection of lung impairments, often before symptoms become noticeable, leading to quicker interventions.
- Monitoring Disease Progression: Regular spirometry tests allow healthcare providers to track the progression of respiratory conditions and adjust treatment plans accordingly.
- Assessing Treatment Efficacy: Spirometry can be used to evaluate how well prescribed treatments are working, based on changes in airflow measurements.
- Risk Stratification: It helps in determining the degree of airway obstruction, which is essential for assessing the risk of complications and planning further care.
Overall, spirometry is indispensable in understanding the dynamics of lung health, guiding treatment decisions, and improving patient outcomes in individuals with chronic respiratory conditions. By providing objective data, it ensures that patients receive the most appropriate care tailored to their specific needs.
Latest Research in Chronic Respiratory Disease Treatment
Recent advances in the treatment of chronic lung conditions have been driven by groundbreaking studies and innovations in medical technology. Researchers continue to explore new therapies aimed at improving lung function, alleviating symptoms, and enhancing quality of life for patients. This evolving field is witnessing significant progress, with new treatments offering hope for better disease management and improved patient outcomes.
One of the most exciting areas of research is the development of targeted therapies that address the underlying mechanisms of respiratory impairments. These therapies aim to reduce inflammation and prevent further damage to the lungs, providing a more personalized approach to treatment. Clinical trials are also investigating the potential of new drug classes, including biologics, which target specific molecules involved in disease progression.
Another promising area of exploration is the integration of technology in treatment regimens. Digital health tools, such as mobile apps and wearable devices, are helping patients track their symptoms, medication usage, and overall health status. These innovations allow for more timely interventions and better management of chronic conditions outside of traditional clinical settings.
Additionally, there is growing interest in the role of lifestyle interventions, including pulmonary rehabilitation programs and smoking cessation initiatives, in improving patient outcomes. Research is focused on optimizing these non-pharmacological treatments to complement medical therapies, ensuring a holistic approach to disease management.
As the field continues to advance, these studies bring us closer to more effective treatments and a deeper understanding of chronic respiratory diseases. The goal remains to improve the lives of those affected by these conditions through innovative therapies and comprehensive care strategies.
Managing Respiratory Conditions During Exacerbations
During episodes of intensified symptoms, effective management is crucial to prevent further deterioration and minimize discomfort. These flare-ups can result from various triggers, including infections, environmental pollutants, or even changes in weather. Prompt intervention can make a significant difference in the overall health outcomes of individuals experiencing such events.
One of the primary approaches to managing these episodes involves optimizing medication use. Short-acting bronchodilators are commonly prescribed to relieve airway constriction quickly. In some cases, corticosteroids may also be administered to reduce inflammation and control symptoms. It’s essential for healthcare providers to assess the severity of the episode and adjust medications accordingly to achieve the best possible result.
In more severe instances, supplemental oxygen therapy may be required to ensure adequate oxygen levels in the blood. Close monitoring of oxygen saturation is critical, as low levels can lead to complications. For patients with frequent exacerbations, establishing a personalized action plan in advance can help prevent unnecessary hospitalizations and facilitate quicker recovery at home.
Non-medication interventions are equally important in managing flare-ups. Ensuring proper hydration, maintaining a calm and restful environment, and encouraging controlled breathing exercises can contribute to symptom relief. These practices are often part of a comprehensive management strategy that supports both physical and emotional well-being during challenging periods.
Finally, it is essential for individuals to recognize the early warning signs of exacerbations. Increased shortness of breath, changes in mucus production, or a cough that worsens over time may indicate the onset of a flare-up. Educating patients and their caregivers on these signs ensures timely action and can significantly reduce the risk of complications.
Understanding Respiratory Disease Staging and Grading
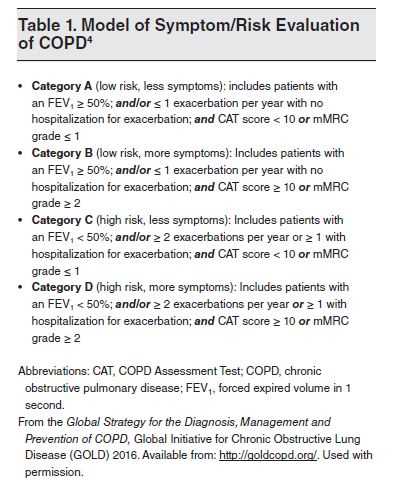
Classifying the severity of chronic lung diseases helps in providing targeted treatment and anticipating potential complications. These systems are based on various clinical parameters such as lung function, symptoms, and the frequency of exacerbations. By evaluating these factors, healthcare providers can identify the stage of the condition, allowing for better management and improved quality of life for patients.
Staging generally refers to the overall extent of the disease, while grading is focused on the severity of individual symptoms. The process involves a combination of physical examinations, symptom assessments, and lung function tests. This detailed evaluation helps determine appropriate interventions and monitor progression over time.
Staging System Overview
One commonly used method for staging is based on lung function measurements, specifically the forced expiratory volume in one second (FEV1). This test measures how much air a person can exhale in one second and is used to categorize the severity of airflow limitation.
| Stage | FEV1 (%) of Predicted Value | Severity |
|---|---|---|
| Stage 1 | 80% or more | Mild |
| Stage 2 | 50-79% | Moderate |
| Stage 3 | 30-49% | Severe |
| Stage 4 | Less than 30% | Very Severe |
Grading Symptom Severity
Grading the severity of symptoms often involves assessing shortness of breath, cough, and mucus production. This can be done using various scales such as the Modified Medical Research Council (mMRC) dyspnea scale or the COPD Assessment Test (CAT). Both tools help healthcare providers understand the functional limitations that patients experience, which is critical for creating an effective treatment plan.
Grading also takes into account the frequency of exacerbations and hospitalizations, as these factors contribute to a patient’s overall prognosis. For example, individuals who experience frequent flare-ups may be categorized into higher severity grades, requiring more aggressive management strategies to prevent further decline.
By using both staging and grading systems, healthcare providers are equipped to assess disease progression more accurately, tailor treatment plans accordingly, and help patients better manage their condition over time.
Improving Quality of Life with Chronic Lung Conditions
Enhancing the well-being of individuals with chronic respiratory diseases involves adopting a multi-faceted approach. This includes both medical treatments and lifestyle changes aimed at improving lung function, reducing symptoms, and increasing overall physical and mental health. Managing these conditions effectively helps patients regain control of their daily activities and enhances their ability to live more comfortably.
Several strategies can be utilized to improve the quality of life, from breathing exercises to physical rehabilitation programs, as well as psychological support. It is essential to address not only the physical limitations but also the emotional and mental health challenges that often accompany chronic respiratory conditions.
Key Strategies for Improving Daily Life
- Breathing Techniques: Incorporating specific exercises, such as diaphragmatic breathing or pursed-lip breathing, can help reduce shortness of breath and improve oxygen intake. These techniques help patients manage respiratory distress and enhance their ability to perform daily tasks.
- Regular Physical Activity: Engaging in tailored exercise routines helps increase stamina and muscle strength, which can significantly improve mobility and reduce the feeling of fatigue. Simple walking, swimming, or strength training may be adapted to a person’s abilities.
- Medication Adherence: Consistently following prescribed medication regimens, including inhalers or oral medications, plays a critical role in managing symptoms and preventing flare-ups. Monitoring the correct use of medications can help maintain stable lung function and reduce complications.
- Nutritional Support: A balanced diet is essential for maintaining a healthy weight and supporting lung function. Patients should focus on foods rich in vitamins and antioxidants, which can help reduce inflammation and improve overall health.
- Psychological Support: Mental well-being is crucial in chronic illness management. Accessing therapy, joining support groups, or practicing mindfulness techniques can significantly alleviate feelings of anxiety or depression that may arise due to the disease.
Additional Considerations for Enhanced Wellness
- Smoking Cessation: One of the most impactful steps is quitting smoking, as it is a primary cause of lung damage. Support programs, medications, and counseling can greatly increase the success rates of quitting.
- Vaccinations: Receiving vaccinations for flu, pneumonia, and other respiratory infections can help reduce the risk of serious complications and prevent further lung damage.
- Environmental Factors: Minimizing exposure to air pollutants, allergens, and other irritants can help reduce symptom exacerbation. Maintaining good indoor air quality and avoiding secondhand smoke are essential steps in reducing lung strain.
By implementing these strategies, individuals with chronic lung conditions can manage their symptoms more effectively, improving their overall quality of life and maintaining greater independence in daily activities. Comprehensive care that addresses both physical and emotional aspects is crucial for long-term success.